Infect Chemother.
2012 Feb;44(1):31-34. 10.3947/ic.2012.44.1.31.
A Rare Case of Pericardial Actinomycosis
- Affiliations
-
- 1Department of Internal Medicine, Yonsei University Wonju College of Medicine, Wonju, Korea. hyksos@yonsei.ac.kr
- 2Department of Pathology, Yonsei University Wonju College of Medicine, Wonju, Korea.
- 3Department of Thoracic and Cardiovascular Surgery, Yonsei University Wonju College of Medicine, Wonju, Korea.
- KMID: 1782396
- DOI: http://doi.org/10.3947/ic.2012.44.1.31
Abstract
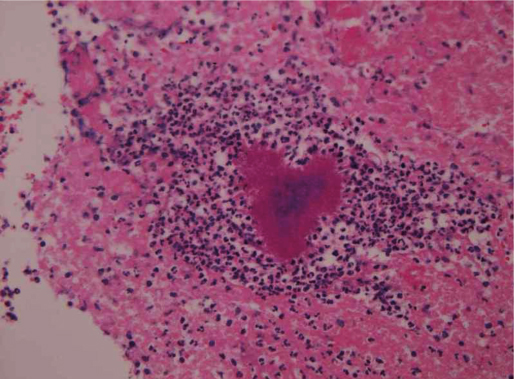
- Actinomycosis is a common chronic suppurative and granulomatous infection caused by anaerobic or microphilic bacteria primarily from the genus Actinomyces. However, Actinomyces is a rare cause of pericarditis. We experienced a rare case of pericardial actinomycosis. A previously healthy 44-year-old man presented with 3 days of fever, chest pain, and clinical signs of congestive heart failure. Chest computed tomography showed pericardial effusion, pericardial thickening, and bilateral pleural effusion. A subxiphoidpericardiotomy was performed, and a histological specimen was taken from the pericardium. A histological section of the pericardium showed an actinomycotic granule (sulfur granule). His symptoms and signs improved after administration of piperacillin/tazobactam and steroids. He was uneventfully discharged on oral amoxicillin/clavulanate. He recovered fully with no recurrence after six months of follow-up.
Keyword
MeSH Terms
Figure
Reference
-
1. Russo T. Fauci AS, Braunwald E, Kasper DL, Hauser SL, Longo DL, Jameson JL, Loscalzo J, editors. Actinomycosis. Harrison's principles of internal medicine. 2008. 17th ed. USA: McGraw-Hill;996–999.2. Schlossberg D, Franco-Jove D, Woodward C, Shulman J. Pericarditis with effusion casued by Actinomyces israelii. Chest. 1976. 69:680–682.
Article3. Jánoskuti L, Lengyel M, Fenyvesi T. Cardiac actinomycosis in a patient presenting with acute cardiac tamponade and a mass mimicking pericardial tumour. Heart. 2004. 90:e27.
Article4. Kim DJ, Rhu HU, Park JE, Jung SU, Kim GH, Koo BW, Lee IS. A case of pericardial actinomycosis with acute myocardial infarction and cerebral infarction: mimicking pericardial tuberculosis. Korean J Med. 2005. 69:555–560.5. Shinagawa N, Yamaguchi E, Takahashi T, Nishimura M. Pulmonary actinomycosis followed by pericarditis and intractable pleuritis. Intern Med. 2002. 41:319–322.
Article6. Hsieh MJ, Liu HP, Chang JP, Chang CH. Thoracic actinomycosis. Chest. 1993. 104:366–370.
Article7. Cornell A, Shookhoff HB. Actinomycosis of the heart simulating rheumatic fever: report of three cases of cardiac actinomycosis, with a review of the literature. Arch Intern Med. 1944. 74:11–27.8. Fife TD, Finegold SM, Grennan T. Pericardial actinomycosis: case report and review. Rev Infect Dis. 1991. 13:120–126.
Article9. Klacsmann PG, Bulkley BH, Hutchins GM. The changed spectrum of purulent pericarditis: an 86 year autopsy experience in 200 patients. Am J Med. 1977. 63:666–673.10. Datta JS, Raff MJ. Actinomycotic pleuropericarditis. Am Rev Respir Dis. 1974. 110:338–341.11. Moniruddin ABM, Begum H, Nahar K. Actinomycosis: an update. Medicine today. 2010. 33:43–47.
Article12. Acevedo F, Baudrand R, Letelier LM, Gaete P. Actinomycosis: a great pretender: case reports of unusual presentations and a review of the literature. Int J Infect Dis. 2008. 12:358–362.
Article13. Slutzker AD, Claypool WD. Pericardial actinomycosis with cardiac tamponade from a contiguous thoracic lesion. Thorax. 1989. 44:442–443.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of pericardial actinomycosis with acute myocardial infarction and cerebral infarction: mimicking pericardial tuberculosis
- A Case of Actinomycosis of the Maxillary Sinus Accompanied with Fungal Ball
- Actinomycosis in Urachal Sinus: A Case Report
- Two Cases of Vesical Actinomycosis Misdiagnosed as Bladder Tumor
- A Case of Pelvic Actinomycosis Simulating Metastatic Ovarian Cancer