Ewha Med J.
2013 Dec;36(Suppl):S5-S8. 10.12771/emj.2013.36.S.S5.
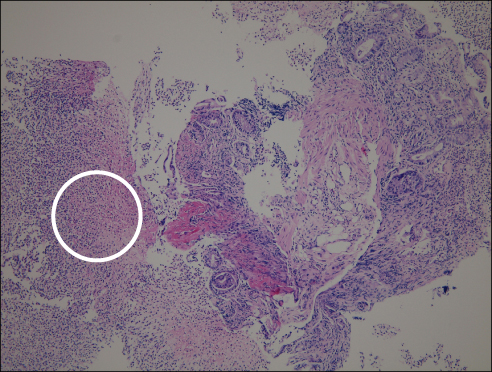
Clostridium difficile Colitis after Topical Ophthalmic Use of Levofloxacin
- Affiliations
-
- 1Department of Internal Medicine, Daerim Saint Mary's Hospital, Seoul, Korea. loveandy@hanmail.net
- KMID: 1726726
- DOI: http://doi.org/10.12771/emj.2013.36.S.S5
Abstract
- Clostridium difficile colitis (CDC) has been associated with virtually all available antibiotics. It is well known that administration of drugs by the ocular route can result in systemic absorption with the possibility of systemic effect. We report a case of a 74-year-old woman who was treated with 0.5% levofloxacin eyedrops for ten weeks running for the post operative management of two separate bilateral cataract surgeries. Toxin assay for C. difficile was positive and the endoscopic findings were compatible with CDC. The plasma concentrations reached after intraocular administration of levofloxacin seem so trivial, but the administration of topical agents could make accumulated effect and be a potential cause of systemic toxicity.
MeSH Terms
Figure
Reference
-
1. Larson HE, Price AB, Honour P, Borriello SP. Clostridium difficile and the aetiology of pseudomembranous colitis. Lancet. 1978; 1:1063–1066.2. Fraunfelder FT, Bagby GC Jr, Kelly DJ. Fatal aplastic anemia following topical administration of ophthalmic chloramphenicol. Am J Ophthalmol. 1982; 93:356–360.3. Coleman AL, Diehl DL, Jampel HD, Bachorik PS, Quigley HA. Topical timolol decreases plasma high-density lipoprotein cholesterol level. Arch Ophthalmol. 1990; 108:1260–1263.4. Bowman RJ, Cope J, Nischal KK. Ocular and systemic side effects of brimonidine 0.2% eye drops (Alphagan) in children. Eye (Lond). 2004; 18:24–26.5. Centers for Disease Control and Prevention (CDC). Severe Clostridium difficile-associated disease in populations previously at low risk: four states, 2005. MMWR Morb Mortal Wkly Rep. 2005; 54:1201–1205.6. Cohen SH, Gerding DN, Johnson S, Kelly CP, Loo VG, McDonald LC, et al. Clinical practice guidelines for Clostridium difficile infection in adults: 2010 update by the society for healthcare epidemiology of America (SHEA) and the infectious diseases society of America (IDSA). Infect Control Hosp Epidemiol. 2010; 31:431–455.7. Muto CA, Pokrywka M, Shutt K, Mendelsohn AB, Nouri K, Posey K, et al. A large outbreak of Clostridium difficile-associated disease with an unexpected proportion of deaths and colectomies at a teaching hospital following increased fluoroquinolone use. Infect Control Hosp Epidemiol. 2005; 26:273–280.8. Vistakon Pharmaceuticals LLC. DailyMed: Quixin (levofloxacin) solution [Internet]. Bethesda (MD): National Institutes of Health, Health & Human Services;2011. cited 2013 Mar. Available from: http://dailymed.nlm.nih.gov/dailymed/lookup.cfm?setid=09b3a912-97f9-45ae-a162-9f45c860dc22.9. Gaynor BD, Chidambaram JD, Cevallos V, Miao Y, Miller K, Jha HC, et al. Topical ocular antibiotics induce bacterial resistance at extraocular sites. Br J Ophthalmol. 2005; 89:1097–1099.10. Nelson WL, Fraunfelder FT, Sills JM, Arrowsmith JB, Kuritsky JN. Adverse respiratory and cardiovascular events attributed to timolol ophthalmic solution, 1978-1985. Am J Ophthalmol. 1986; 102:606–611.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Characteristics of Clostridium difficile colitis
- The Risk Factors of Clostridium difficile Colitis in Colorectal Surgery
- Left-sided Ulcerative Colitis Reactivated and Aggravated during Clostridium difficile Infection
- A Case of Pseudomembranous Colitis due to Clostridium difficile
- Clostridium difficile Infection: A Worldwide Disease