Microsurgical Extraction of a Malfunctioned Pipeline Embolization Device Following Complete Deployment
- Affiliations
-
- 1Department of Neurological Surgery, University of Virginia, Charlottesville, VA, United States of America. kcl3j@hscmail.mcc.virginia.edu
- KMID: 1491446
- DOI: http://doi.org/10.7461/jcen.2013.15.3.241
Abstract
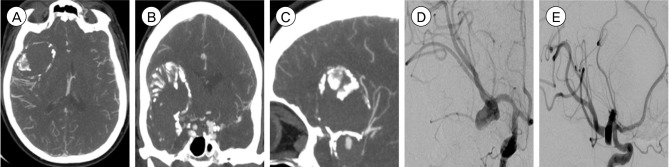
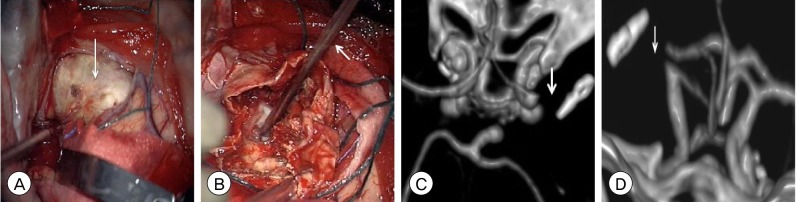
- The Pipeline Embolization Device (PED) is an effective treatment approach for complex intracranial aneurysms. Intraprocedural complications during PED deployment are seldom reported. We report a rare complication of a PED malfunction identified immediately following complete deployment during endovascular treatment of a giant middle cerebral artery (MCA) bifurcation aneurysm. After multiple failed attempts at endovascular retrieval of the malfunctioned PED, the patient was taken for microsurgical extraction due to accumulation of thrombus on the proximal unopened portion of the stent and widespread distal dissemination of emboli. After removing the PED from the vessel lumen and resecting the giant aneurysm, we could not reanastamose the proximal MCA to the distal segment. The management of PED malfunction is poorly understood. While removal of an incompletely deployed PED may be undertaken with limited adverse effects, retrieval of a fully deployed PED is associated with a much higher risk of morbidity. Until larger case series of such complications better define the risks and benefits of endovascular or microsurgical retrieval of malfunctioned PEDs, the management of these rare intraprocedural complications will be based on the unique aspects of each individual case and the expertise of the treating neurointerventionalist.
Keyword
MeSH Terms
Figure
Cited by 4 articles
-
Balloon Anchor Technique for Pipeline Embolization Device Deployment Across the Neck of a Giant Intracranial Aneurysm
Dale Ding, Robert M. Starke, Avery J. Evans, Mary E. Jensen, Kenneth C. Liu
J Cerebrovasc Endovasc Neurosurg. 2014;16(2):125-130. doi: 10.7461/jcen.2014.16.2.125.Microsurgical Strategies Following Failed Endovascular Treatment with the Pipeline Embolization Device: Case of a Giant Posterior Cerebral Artery Aneurysm
Dale Ding, Robert M. Starke, Kenneth C. Liu
J Cerebrovasc Endovasc Neurosurg. 2014;16(1):26-31. doi: 10.7461/jcen.2014.16.1.26.Endovascular Management of Intracranial Aneurysms: Advances in Stenting Techniques and Technology
Dale Ding
J Cerebrovasc Endovasc Neurosurg. 2015;17(4):331-333. doi: 10.7461/jcen.2015.17.4.331.Inadvertent Complication of a Pipeline Embolization Device for Treatment with Vertebral Artery Dissecting Aneurysm : Distal Tip Fracture of Delivery Wire
Jung Soo Park, Hyo Sung Kwak, Jong Myong Lee
J Korean Neurosurg Soc. 2016;59(5):521-524. doi: 10.3340/jkns.2016.59.5.521.
Reference
-
1. International Study of Unruptured Intracranial Aneurysms Investigators. Unruptured intracranial aneurysms-risk of rupture and risks of surgical intervention. N Engl J Med. 1998; 12. 339(24):1725–1733. PMID: 9867550.2. Becske T, Kallmes DF, Saatci I, McDougall CG, Szikora I, Lanzino G, et al. Pipeline for Uncoilable or Failed Aneurysms: Results from a Multicenter Clinical Trial. Radiology. 2013; 6. 267(3):858–868. PMID: 23418004.
Article3. Cantore G, Santoro A, Guidetti G, Delfinis CP, Colonnese C, Passacantilli E. Surgical treatment of giant intracranial aneurysms: Current viewpoint. Neurosurgery. 2008; 10. 63(4 Suppl 2):279–289. discussion 289-90. PMID: 18981833.
Article4. Chen M, Goldstein-Smith L. Endovascular rescue of a misshapen intracranial stent: Report of two cases. J Neurointerv Surg. 2011; 3. 3(1):25–26. PMID: 21990782.
Article5. Colby GP, Gomez JF, Lin LM, Paul AR, Coon AL. In situ removal of the pipeline embolization device: The 'corking' and 'pseudo-corking' techniques. J Neurointerv Surg. 2013; 3. 5(2):e6. PMID: 22362818.
Article6. Fargen KM, Velat GJ, Lawson MF, Mocco J, Hoh BL. Review of reported complications associated with the Pipeline Embolization Device. World Neurosurg. 2012; Mar-Apr. 77(3-4):403–404. PMID: 22360865.
Article7. Fiorella D, Lylyk P, Szikora I, Kelly ME, Albuquerque FC, McDougall CG, et al. Curative cerebrovascular reconstruction with the Pipeline embolization device: The emergence of definitive endovascular therapy for intracranial aneurysms. J Neurointerv Surg. 2009; 7. 1(1):56–65. PMID: 21994109.
Article8. McAuliffe W, Wycoco V, Rice H, Phatouros C, Singh TJ, Wenderoth J. Immediate and midterm results following treatment of unruptured intracranial aneurysms with the pipeline embolization device. AJNR Am J Neuroradiol. 2012; 1. 33(1):164–170. PMID: 21979492.
Article9. Nelson PK, Lylyk P, Szikora I, Wetzel SG, Wanke I, Fiorella D. The pipeline embolization device for the intracranial treatment of aneurysms trial. AJNR Am J Neuroradiol. 2011; 1. 32(1):34–40. PMID: 21148256.
Article10. Oh Y, Hwang DH, Ko YH, Kang IW, Kim IS, Hur CW. Foreign body removal by snare loop: During intracranial stent procedure. Neurointervention. 2012; 2. 7(1):50–53. PMID: 22454786.
Article11. Parkinson RJ, Eddleman CS, Batjer HH, Bendok BR. Giant intracranial aneurysms: Endovascular challenges. Neurosurgery. 2006; 11. 59(5 Suppl 3):S103–S112. discussion S3-13. PMID: 17053593.
Article12. Raftopoulos C, Goffette P, Billa RF, Mathurin P. Transvascular coil hooking procedure to retrieve an unraveled Guglielmi detachable coil: Technical note. Neurosurgery. 2002; 4. 50(4):912–914. discussion 914-5. PMID: 11904050.
Article13. Wiebers DO, Whisnant JP, Huston J 3rd, Meissner I, Brown RD Jr, Piepgras DG, et al. Unruptured intracranial aneurysms: Natural history, clinical outcome, and risks of surgical and endovascular treatment. Lancet. 2003; 7. 362(9378):103–110. PMID: 12867109.
Article14. Yu SC, Kwok CK, Cheng PW, Chan KY, Lau SS, Lui WM, et al. Intracranial aneurysms: Midterm outcome of pipeline embolization device- A prospective study in 143 patients with 178 aneurysms. Radiology. 2012; 12. 265(3):893–901. PMID: 22996749.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Microsurgical Strategies Following Failed Endovascular Treatment with the Pipeline Embolization Device: Case of a Giant Posterior Cerebral Artery Aneurysm
- Pipeline Embolization Device for Giant Internal Carotid Artery Aneurysms: 9-Month Follow-Up Results of Two Cases
- Flow diverter stenting for intracranial aneurysms in the pediatric population: Two case reports and literature review
- Treatment for Giant Fusiform Aneurysm Located in the Cavernous Segment of the Internal Carotid Artery Using the Pipeline Embolization Device
- Balloon Anchor Technique for Pipeline Embolization Device Deployment Across the Neck of a Giant Intracranial Aneurysm