J Cerebrovasc Endovasc Neurosurg.
2014 Jun;16(2):125-130. 10.7461/jcen.2014.16.2.125.
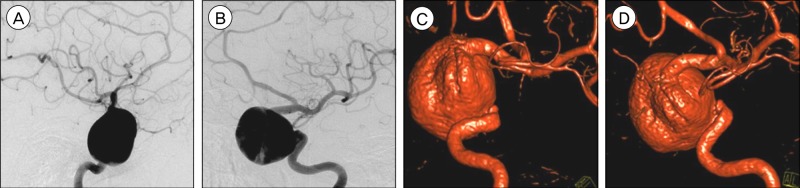
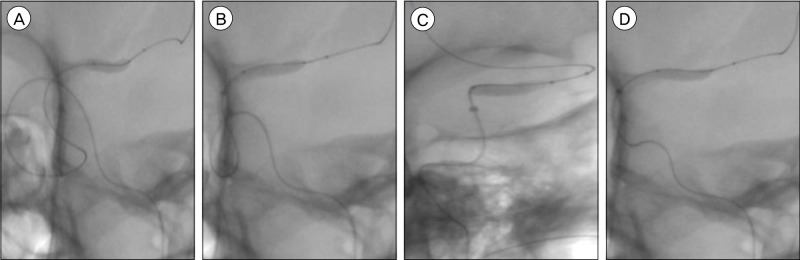
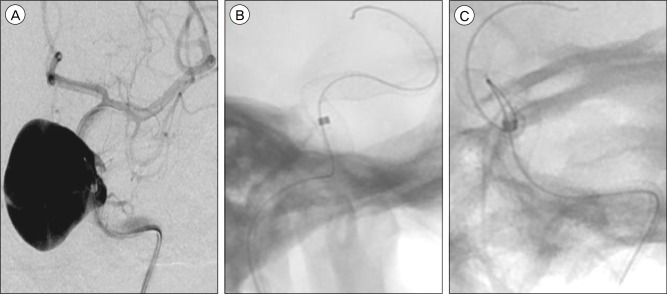
Balloon Anchor Technique for Pipeline Embolization Device Deployment Across the Neck of a Giant Intracranial Aneurysm
- Affiliations
-
- 1University of Virginia, Department of Neurological Surgery, Charlottesville, VA, United States. kcl3j@hscmail.mcc.virginia.edu
- 2University of Virginia, Department of Radiology, Charlottesville, VA, United States.
- KMID: 1963181
- DOI: http://doi.org/10.7461/jcen.2014.16.2.125
Abstract
- Treatment of giant intracranial aneurysms, via either surgical or endovascular approaches, is associated with a high level of technical difficulty as well as a high rate of treatment-related morbidity and mortality. Flow-diverting stents, such as the Pipeline embolization device (PED), have drastically altered the therapeutic strategies for the treatment of giant aneurysms. Gaining endovascular access using a microcatheter to the portion of the parent artery distal to the aneurysm neck is requisite for safe and effective stent deployment. Giant aneurysms are often associated with vascular tortuosity, which necessitates significant catheter support systems to enable maneuvering of PEDs across the aneurysm neck. This is also required in order to reduce the probability of stent herniation within giant aneurysms. We report on a case of a giant supraclinoid internal carotid artery (ICA) aneurysm which was treated successfully with a PED utilizing a balloon anchor technique to facilitate direct microcatheter access across the aneurysm neck.
Keyword
MeSH Terms
Figure
Cited by 1 articles
-
Endovascular Management of Intracranial Aneurysms: Advances in Stenting Techniques and Technology
Dale Ding
J Cerebrovasc Endovasc Neurosurg. 2015;17(4):331-333. doi: 10.7461/jcen.2015.17.4.331.
Reference
-
1. Becske T, Kallmes DF, Saatci I, McDougall CG, Szikora I, Lanzino G, et al. Pipeline for uncoilable or failed aneurysms: results from a multicenter clinical trial. Radiology. 2013; 6. 267(3):858–868. PMID: 23418004.
Article2. Cantore G, Santoro A, Guidetti G, Delfinis CP, Colonnese C, Passacantilli E. Surgical treatment of giant intracranial aneurysms: current viewpoint. Neurosurgery. 2008; 10. 63(4 Suppl 2):279–289. discussion 289-90. PMID: 18981833.
Article3. Cekirge SH, Yavuz K, Geyik S, Saatci I. HyperForm balloon-assisted endovascular neck bypass technique to perform balloon or stent-assisted treatment of cerebral aneurysms. AJNR Am J Neuroradiol. 2007; 8. 28(7):1388–1390. PMID: 17698548.
Article4. Chalouhi N, Starke RM, Yang S, Bovenzi CD, Tjoumakaris S, Hasan D, et al. Extending the indications of flow diversion to small, unruptured, saccular aneurysms of the anterior circulation. Stroke. 2014; 1. 45(1):54–58. PMID: 24253543.
Article5. Chalouhi N, Tjoumakaris S, Dumont AS, Gonzalez LF, Randazzo C, Starke RM, et al. Treatment of posterior circulation aneurysms with the pipeline embolization device. Neurosurgery. 2013; 6. 72(6):883–889. PMID: 23407289.
Article6. Colby GP, Gomez JF, Lin LM, Paul AR, Coon AL. In situ removal of the pipeline embolization device: the 'corking' and 'pseudo-corking' techniques. J Neurointerv Surg. 2013; 3. 5(2):e6. PMID: 22362818.
Article7. Cruz JP, O'Kelly C, Kelly M, Wong JH, Alshaya W, Martin A, et al. Pipeline embolization device in aneurysmal subarachnoid hemorrhage. AJNR Am J Neuroradiol. 2013; 2. 34(2):271–276. PMID: 23064594.
Article8. Ding D, Liu KC. Microsurgical extraction of a malfunctioned pipeline embolization device following complete deployment. J Cerebrovasc Endovasc Neurosurg. 2013; 9. 15(3):241–245. PMID: 24167807.
Article9. Drake CG. Giant intracranial aneurysms: experience with surgical treatment in 174 patients. Clin Neurosurg. 1979; 26:12–95. PMID: 544122.
Article10. Edwards L, Kota G, Morris PP. The sea anchor technique: a novel method to aid in stent-assisted embolization of giant cerebral aneurysms. J Neurointerv Surg. 2013; 11. 5(6):e39. PMID: 22952247.
Article11. Fargen KM, Velat GJ, Lawson MF, Hoh BL, Mocco J. The stent anchor technique for distal access through a large or giant aneurysm. J Neurointerv Surg. 2013; 7. 5(4):e24. PMID: 22544820.
Article12. Fiorella D, Lylyk P, Szikora I, Kelly ME, Albuquerque FC, McDougall CG, et al. Curative cerebrovascular reconstruction with the Pipeline embolization device: the emergence of definitive endovascular therapy for intracranial aneurysms. J Neurointerv Surg. 2009; 7. 1(1):56–65. PMID: 21994109.
Article13. Jahromi BS, Mocco J, Bang JA, Gologorsky Y, Siddiqui AH, Horowitz MB, et al. Clinical and angiographic outcome after endovascular management of giant intracranial aneurysms. Neurosurgery. 2008; 10. 63(4):662–674. discussion 674-5. PMID: 18981877.
Article14. Nelson PK, Lylyk P, Szikora I, Wetzel SG, Wanke I, Fiorella D. The pipeline embolization device for the intracranial treatment of aneurysms trial. AJNR Am J Neuroradiol. 2011; 1. 32(1):34–40. PMID: 21148256.
Article15. Parkinson RJ, Eddleman CS, Batjer HH, Bendok BR. Giant intracranial aneurysms: endovascular challenges. Neurosurgery. 2006; 11. 59(5 Suppl 3):S103–S112. discussion S103-13. PMID: 17053593.
Article16. Pistocchi S, Blanc R, Bartolini B, Piotin M. Flow diverters at and beyond the level of the circle of willis for the treatment of intracranial aneurysms. Stroke. 2012; 4. 43(4):1032–1038. PMID: 22282890.
Article17. Shigematsu T, Fujinaka T, Yoshimine T, Imamura H, Ishii A, Sakai C, et al. Endovascular therapy for asymptomatic unruptured intracranial aneurysms: JR-NET and JR-NET2 findings. Stroke. 2013; 10. 44(10):2735–2742. PMID: 23899916.18. Siddiq F, Adil MM, Kainth D, Moen S, Qureshi AI. The emergence of endovascular treatment-only centers for treatment of intracranial aneurysms in the United States. J Stroke Cerebrovasc Dis. 2013; 11. 22(8):e504–e510. PMID: 23810350.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Open-cell Stent Deployment across the Wide Neck of a Large Middle Cerebral Aneurysm Using the Stent Anchor Technique
- Pipeline Embolization Device for Giant Internal Carotid Artery Aneurysms: 9-Month Follow-Up Results of Two Cases
- Microsurgical Extraction of a Malfunctioned Pipeline Embolization Device Following Complete Deployment
- Treatment for Giant Fusiform Aneurysm Located in the Cavernous Segment of the Internal Carotid Artery Using the Pipeline Embolization Device
- Microsurgical Strategies Following Failed Endovascular Treatment with the Pipeline Embolization Device: Case of a Giant Posterior Cerebral Artery Aneurysm