J Korean Soc Spine Surg.
2013 Sep;20(3):123-128. 10.4184/jkss.2013.20.3.123.
Subacute Delayed Ascending Myelopathy after Spinal Cord Injury from Flexion-distraction Injury of Low Thoracic Spine: A Case Report
- Affiliations
-
- 1Department of Orthopedic Surgery, Seoul National University College of Medicine, Korea. bschang@snu.ac.kr
- KMID: 1487979
- DOI: http://doi.org/10.4184/jkss.2013.20.3.123
Abstract
- STUDY DESIGN: A case report.
OBJECTIVES
To report a rare case of subacute delayed ascending myelopathy. SUMMARY OF LITERATURE REVIEW: After low spinal cord injury, the cord injury may proceed to a proximal level and lead to subacute delayed ascending myelopathy. The patient suffered from orthostatic hypotension, weakness and sensory loss in the upper extremities and dyspnea. MRI showed more proximal progression of the spinal cord injury. There is no prevention or treatment for this condition.
MATERIALS AND METHODS
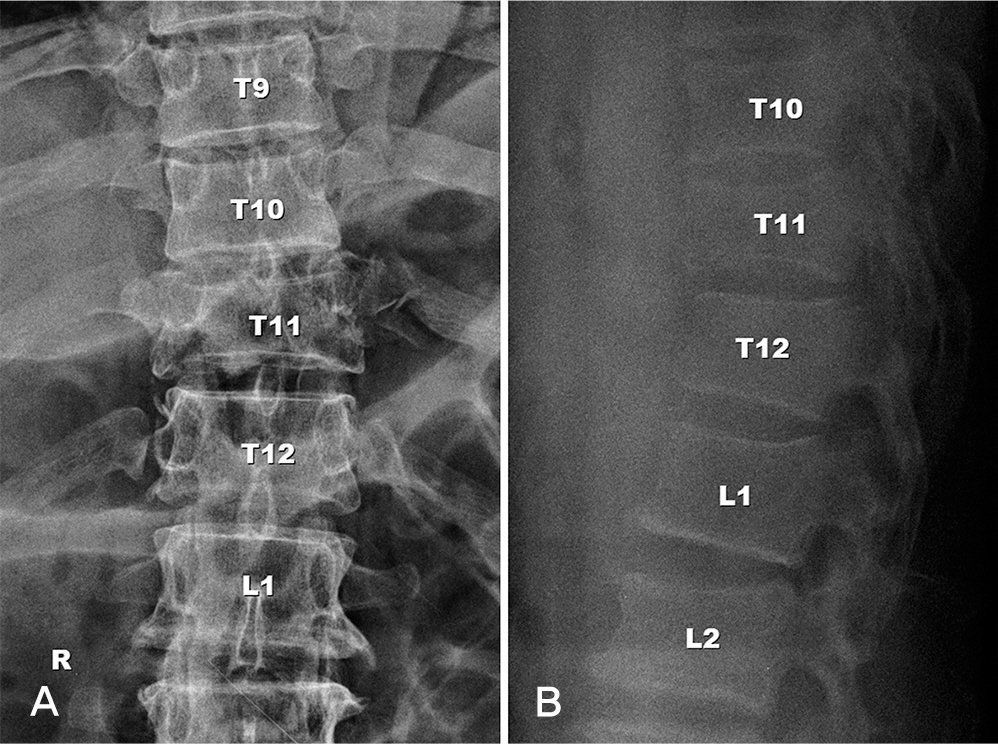
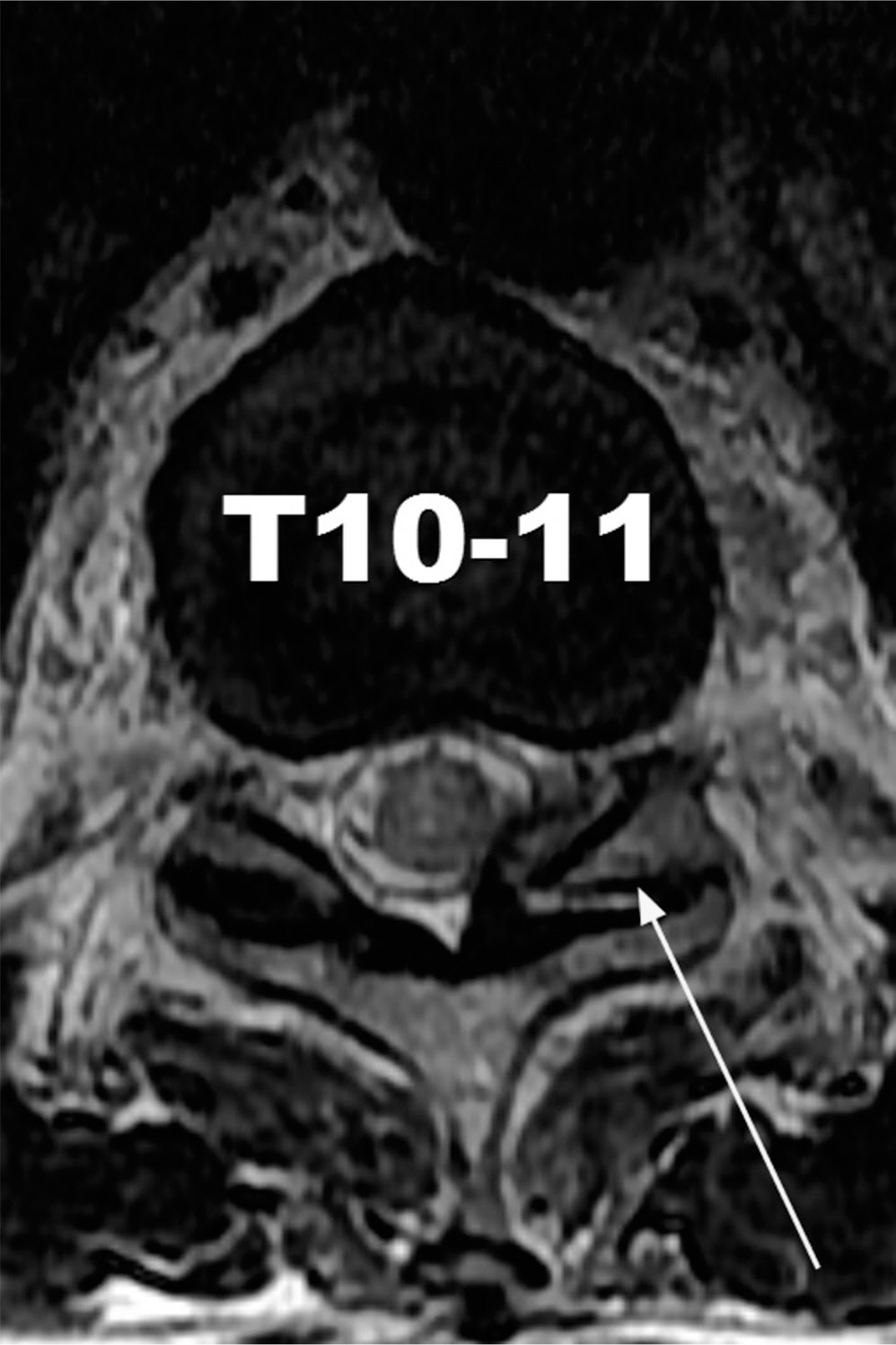
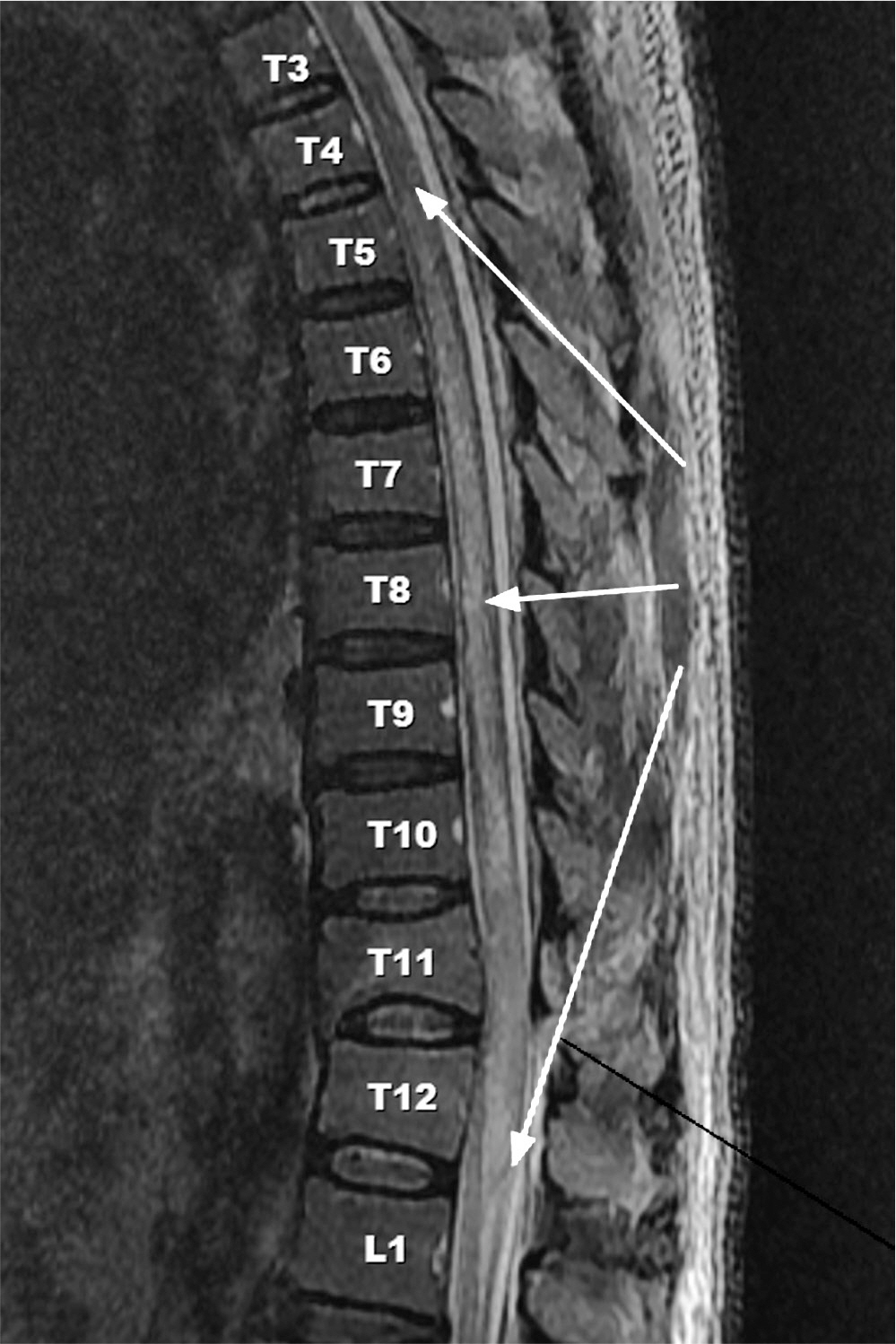
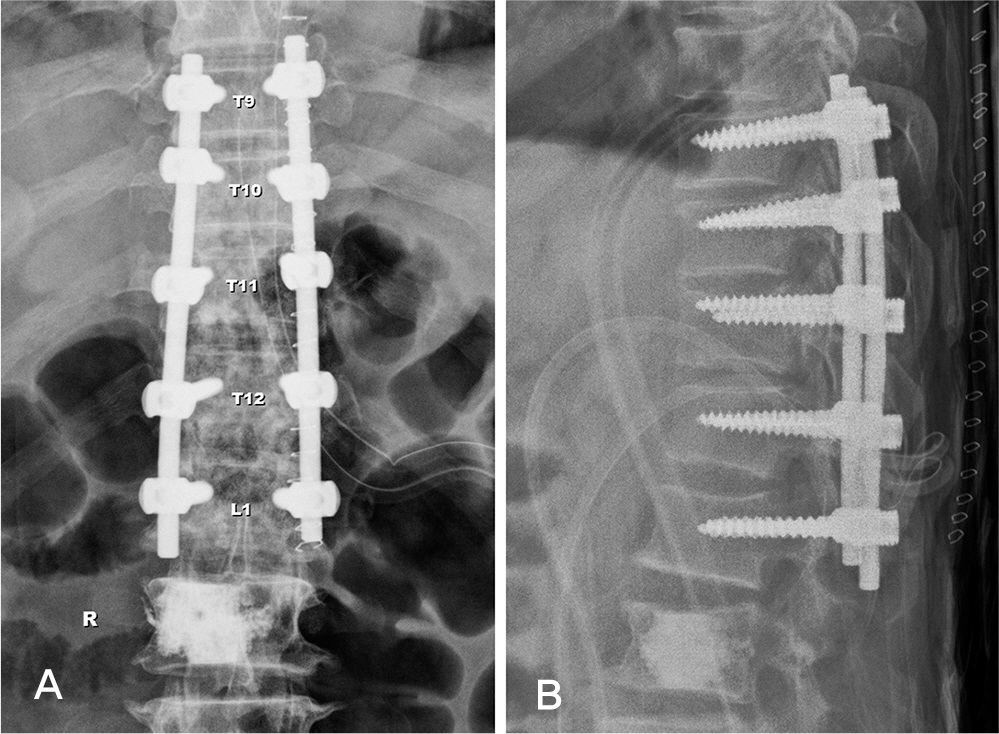
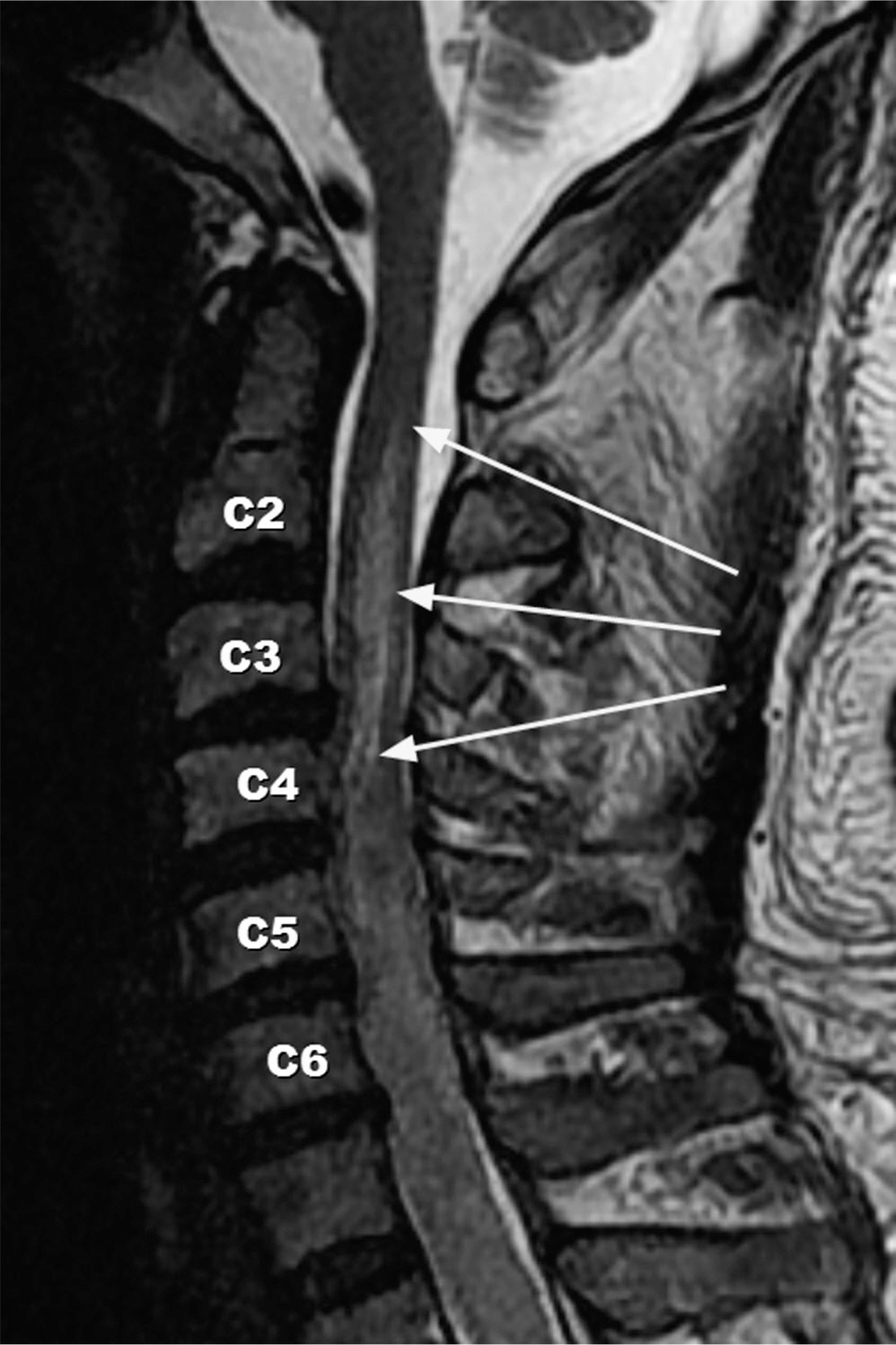
A 62-year-old man fell from heights and had 11th thoracic spine flexion-distraction injury. Upon arrival at the hospital, he was found to suffer from lower extremity weakness and sensory loss, but showed no neurologic symptom in his upper extremities. Two days later, we performed posterior instrumentation with fusion, and no postoperative neurologic symptom change was detected. One week after the fall, he suffered from dyspnea, upper extremity weakness and sensory loss. MRI was taken and we discovered that his spinal cord injury had proceeded to the 2nd cervical spine level.
RESULTS
Three months later, he showed little improvement in his upper extremity motor power, but not to the extent of the previous low spinal injury.
CONCLUSION
Physicians should pay attention to the upper extremity and respiratory function of the patient with low spinal cord injury, because the level of spinal cord injury may proceed to a proximal level.
MeSH Terms
Figure
Reference
-
1. Schmidt BJ. Subacute delayed ascending myelopathy after low spine injury: case report and evidence of a vascular mechanism. Spinal Cord. 2006; 44:322–5.
Article2. Belanger E, Picard C, Lacerte D, Lavallee P, Levi AD. Subacute posttraumatic ascending myelopathy after spinal cord injury. Report of three cases. J Neurosurgery. 2000; 93:294–9.3. Aito S, El Masry WS, Gerner HJ, et al. Ascending myelopathy in the early stage of spinal cord injury. Spinal Cord. 1999; 37:617–23.
Article4. Tator CH, Fehlings MG. Review of the secondary injury theory of acute spinal cord trauma with emphasis on vascular mechanisms. J Neurosurgery. 1991; 75:15–26.
Article5. Sliwa JA, Maclean IC. Ischemic myelopathy: a review of spinal vasculature and related clinical syndromes. Arch Phys Med Rehabil. 1992; 73:365–72.
Article6. Cassar-Pullicino VN, Colhoun E, McLelland M, Mc-Call IW, el Masry W. Hemodynamic alterations in the paravertebral venous plexus after spinal injury. Radiology. 1995; 197:659–63.
Article7. Frankel HL. Ascending cord lesions in the early stages following spinal injury. Paraplegia. 1969; 7:111–8.8. Kumar A, Kumar J, Garg M, Farooque K, Gamanagatti S, Sharma V. Posttraumatic subacute ascending myelopathy in a 24-year-old male patient. Emerg Radiol. 2010; 17:249–52.
Article