J Korean Surg Soc.
2012 Dec;83(6):367-373. 10.4174/jkss.2012.83.6.367.
Specimen index may be a predictive factor for recurrence after primary closure of pilonidal disease
- Affiliations
-
- 1Department of Surgery, Selcuk University Selcuklu Medical School, Konya, Turkey. halptekin@hotmail.com
- 2Department of Surgery, Bandirma Country Hospital, Balikesir, Turkey.
- KMID: 1437532
- DOI: http://doi.org/10.4174/jkss.2012.83.6.367
Abstract
- PURPOSE
The aim of the present study was to evaluate the predictive value of volume of the specimen/body mass index (VS/BMI) ratio for recurrence after surgical therapy of pilonidal disease.
METHODS
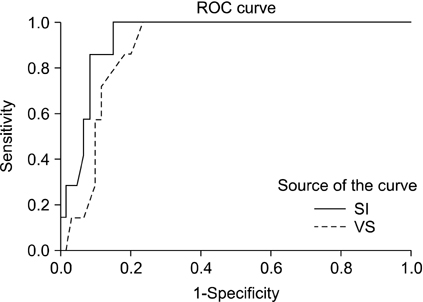
Ninety-eight patients with primary pilonidal disease were enrolled in this study. The VS/BMI ratio was calculated for each patient. This ratio was defined as the specimen index (SI). VS, BMI and SI were evaluated to determine whether there is a relationship between these parameters and recurrence of pilonidal disease. In addition, the predictive ability of SI for recurrence was analyzed by receiver operating characteristic (ROC) curve.
RESULTS
VS and SI were found to be higher in patients with recurrence. ROC curve analysis showed that VS and SI are predictive factors for recurrence in patients treated with primary closure, nevertheless our new index had higher sensitivity and specificity than VS (sensitivity 85.7% vs 71.4% and specificity 90.7% vs 85.1%, respectively). The cut-off level for the greatest sensitivity and specificity for SI was 1.29.
CONCLUSION
Recurrence is higher in patients with high VS regardless of the operation method. SI may be a predictive value in patients treated with primary closure.
Keyword
Figure
Reference
-
1. Sondenaa K, Andersen E, Nesvik I, Soreide JA. Patient characteristics and symptoms in chronic pilonidal sinus disease. Int J Colorectal Dis. 1995. 10:39–42.2. Dwight RW, Maloy JK. Pilonidal sinus; experience with 449 cases. N Engl J Med. 1953. 249:926–930.3. Arumugam PJ, Chandrasekaran TV, Morgan AR, Beynon J, Carr ND. The rhomboid flap for pilonidal disease. Colorectal Dis. 2003. 5:218–221.4. Yilmaz S, Kirimlioglu V, Katz D. Role of simple V-Y advancement flap in the treatment of complicated pilonidal sinus. Eur J Surg. 2000. 166:269.5. Cubukçu A, Gonullu NN, Paksoy M, Alponat A, Kuru M, Ozbay O. The role of obesity on the recurrence of pilonidal sinus disease in patients, who were treated by excision and Limberg flap transposition. Int J Colorectal Dis. 2000. 15:173–175.6. Quinodoz PD, Chilcott M, Grolleau JL, Chavoin JP, Costagliola M. Surgical treatment of sacrococcygeal pilonidal sinus disease by excision and skin flaps: the Toulouse experience. Eur J Surg. 1999. 165:1061–1065.7. Solla JA, Rothenberger DA. Chronic pilonidal disease. An assessment of 150 cases. Dis Colon Rectum. 1990. 33:758–761.8. Zimmerman CE. Outpatient excision and primary closure of pilonidal cysts and sinuses. Long-term follow-up. Am J Surg. 1984. 148:658–659.9. Ertan T, Koc M, Gocmen E, Aslar AK, Keskek M, Kilic M. Does technique alter quality of life after pilonidal sinus surgery? Am J Surg. 2005. 190:388–392.10. Akca T, Colak T, Ustunsoy B, Kanik A, Aydin S. Randomized clinical trial comparing primary closure with the Limberg flap in the treatment of primary sacrococcygeal pilonidal disease. Br J Surg. 2005. 92:1081–1084.11. Anderson JH, Yip CO, Nagabhushan JS, Connelly SJ. Day-case Karydakis flap for pilonidal sinus. Dis Colon Rectum. 2008. 51:134–138.12. Sakr M, El-Hammadi H, Moussa M, Arafa S, Rasheed M. The effect of obesity on the results of Karydakis technique for the management of chronic pilonidal sinus. Int J Colorectal Dis. 2003. 18:36–39.13. Arda IS, Guney LH, Sevmis S, Hicsonmez A. High body mass index as a possible risk factor for pilonidal sinus disease in adolescents. World J Surg. 2005. 29:469–471.14. Madbouly KM. Day-case Limberg flap for recurrent pilonidal sinus: does obesity complicate the issue? Am Surg. 2010. 76:995–999.15. Popeskou S, Christoforidis D, Ruffieux C, Demartines N. Wound infection after excision and primary midline closure for pilonidal disease: risk factor analysis to improve patient selection. World J Surg. 2011. 35:206–211.16. Williams RS. A simple technique for successful primary closure after excision of pilonidal sinus disease. Ann R Coll Surg Engl. 1990. 72:313–314.17. Gilani SN, Furlong H, Reichardt K, Nasr AO, Theophilou G, Walsh TN. Excision and primary closure of pilonidal sinus disease: worthwhile option with an acceptable recurrence rate. Ir J Med Sci. 2011. 180:173–176.18. McCallum IJ, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ. 2008. 336:868–871.19. Mahdy T. Surgical treatment of the pilonidal disease: primary closure or flap reconstruction after excision. Dis Colon Rectum. 2008. 51:1816–1822.20. Akin M, Leventoglu S, Mentes BB, Bostanci H, Gokbayir H, Kilic K, et al. Comparison of the classic Limberg flap and modified Limberg flap in the treatment of pilonidal sinus disease: a retrospective analysis of 416 patients. Surg Today. 2010. 40:757–762.21. Gurer A, Gomceli I, Ozdogan M, Ozlem N, Sozen S, Aydin R. Is routine cavity drainage necessary in Karydakis flap operation? A prospective, randomized trial. Dis Colon Rectum. 2005. 48:1797–1799.22. Topgul K, Ozdemir E, Kilic K, Gokbayir H, Ferahkose Z. Long-term results of limberg flap procedure for treatment of pilonidal sinus: a report of 200 cases. Dis Colon Rectum. 2003. 46:1545–1548.23. Muzi MG, Milito G, Cadeddu F, Nigro C, Andreoli F, Amabile D, et al. Randomized comparison of Limberg flap versus modified primary closure for the treatment of pilonidal disease. Am J Surg. 2010. 200:9–14.24. Kaymakcioglu N, Yagci G, Simsek A, Unlu A, Tekin OF, Cetiner S, et al. Treatment of pilonidal sinus by phenol application and factors affecting the recurrence. Tech Coloproctol. 2005. 9:21–24.25. Kim JK, Jeong JC, Lee JB, Jung KH, Bae BK. S-plasty for pilonidal disease: modified primary closure reducing tension. J Korean Surg Soc. 2012. 82:63–69.26. Bissett IP, Isbister WH. The management of patients with pilonidal disease: a comparative study. Aust N Z J Surg. 1987. 57:939–942.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Evaluation of Wide Excision and Simple Primary Closure of Pilonidal Sinus
- A Case of Pilonidal Sinus Mimicking Inflammatory Epidermal Cyst
- Comparison of Limberg flap and excision and primary closure of pilonidal sinus disease, in terms of quality of life and complications
- S-plasty for pilonidal disease: modified primary closure reducing tension
- Comparative analysis of the same technique-the same surgeon approach in the surgical treatment of pilonidal sinus disease: a retrospective cohort study