J Korean Surg Soc.
2012 Feb;82(2):63-69. 10.4174/jkss.2012.82.2.63.
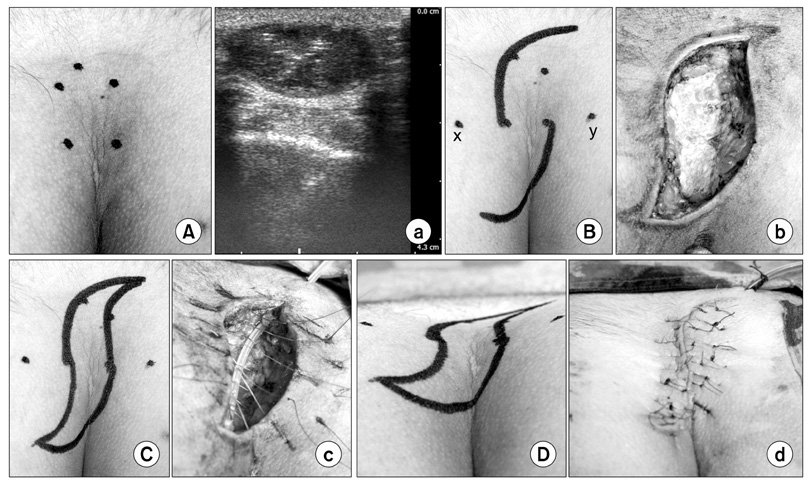
S-plasty for pilonidal disease: modified primary closure reducing tension
- Affiliations
-
- 1Department of Surgery, Armed Forces Capital Hospital, Seongnam, Korea. worms99@hanmail.net
- KMID: 2212203
- DOI: http://doi.org/10.4174/jkss.2012.82.2.63
Abstract
- PURPOSE
S-plasty for pilonidal disease reduces the tension on the midline by distributing it diagonally and flattening the natal cleft. The aim of this study was to evaluate the outcomes of S-plasty on simple midline primary closure and the clinical features of pilonidal patients in a low incidence country.
METHODS
S-plasty was applied on 17 patients from July 2008 to October 2010. Data of these patients were collected with computerized prospective database forms during a perioperative period and via telephone interview for follow-up. Surgical site infection (SSI) was defined according to the Center for Disease Control guidelines. The severity of surgical site infection was graded.
RESULTS
All patients were treated with primary S-plasty. Two patients (11.7%) developed low grade SSI. The average healing time after S-plasty was 18.1 days. No recurrences were observed. The mean follow-up period was 13.5 months (range, 6 to 33 months).
CONCLUSION
We have shown that primary S-plasty for pilonidal disease is simple, and its surgical outcomes are compatible to the results of other surgical treatments. We present primary S-plasty as a feasible treatment option in a low incidence country.
Keyword
MeSH Terms
Figure
Reference
-
1. Allen-Mersh TG. Pilonidal sinus: finding the right track for treatment. Br J Surg. 1990. 77:123–132.2. Thompson MR, Senapati A, Kitchen P. Simple day-case surgery for pilonidal sinus disease. Br J Surg. 2011. 98:198–209.3. Aldemir M, Kara IH, Erten G, Taçyildiz I. Effectiveness of collagenase in the treatment of sacrococcygeal pilonidal sinus disease. Surg Today. 2003. 33:106–109.4. Armstrong JH, Barcia PJ. Pilonidal sinus disease. The conservative approach. Arch Surg. 1994. 129:914–917.5. Karydakis GE. Easy and successful treatment of pilonidal sinus after explanation of its causative process. Aust N Z J Surg. 1992. 62:385–389.6. Washer JD, Smith DE, Carman ME, Blackhurst DW. Gluteal fascial advancement: an innovative, effective method for treating pilonidal disease. Am Surg. 2010. 76:154–156.7. Karydakis GE. New approach to the problem of pilonidal sinus. Lancet. 1973. 2:1414–1415.8. Kitchen PR. Pilonidal sinus: experience with the Karydakis flap. Br J Surg. 1996. 83:1452–1455.9. Mentes O, Bagci M, Bilgin T, Coskun I, Ozgul O, Ozdemir M. Management of pilonidal sinus disease with oblique excision and primary closure: results of 493 patients. Dis Colon Rectum. 2006. 49:104–108.10. Krand O, Yalt T, Berber I, Kara VM, Tellioglu G. Management of pilonidal sinus disease with oblique excision and bilateral gluteus maximus fascia advancing flap: result of 278 patients. Dis Colon Rectum. 2009. 52:1172–1177.11. Paolo B, Stefania R, Massimiliano C, Stefano A, Andrea P, Giorgio L. Modified S-plasty: an alternative to the elliptical excision to reduce the length of suture. Dermatol Surg. 2003. 29:394–398.12. Hallock GG. Is there a "learning curve" for muscle perforator flaps? Ann Plast Surg. 2008. 60:146–149.13. Ferriman D, Gallwey JD. Clinical assessment of body hair growth in women. J Clin Endocrinol Metab. 1961. 21:1440–1447.14. Horan TC, Andrus M, Dudeck MA. CDC/NHSN surveillance definition of health care-associated infection and criteria for specific types of infections in the acute care setting. Am J Infect Control. 2008. 36:309–332.15. Clavien PA, Barkun J, de Oliveira ML, Vauthey JN, Dindo D, Schulick RD, et al. The Clavien-Dindo classification of surgical complications: five-year experience. Ann Surg. 2009. 250:187–196.16. Dindo D, Demartines N, Clavien PA. Classification of surgical complications: a new proposal with evaluation in a cohort of 6336 patients and results of a survey. Ann Surg. 2004. 240:205–213.17. Russell L. Physiology of the skin and prevention of pressure sores. Br J Nurs. 1998. 7:10841088–1092. 1096 passim18. Mentes O, Bagci M, Bilgin T, Ozgul O, Ozdemir M. Limberg flap procedure for pilonidal sinus disease: results of 353 patients. Langenbecks Arch Surg. 2008. 393:185–189.19. Unalp HR, Derici H, Kamer E, Nazli O, Onal MA. Lower recurrence rate for Limberg vs. V-Y flap for pilonidal sinus. Dis Colon Rectum. 2007. 50:1436–1444.20. Petersen S, Koch R, Stelzner S, Wendlandt TP, Ludwig K. Primary closure techniques in chronic pilonidal sinus: a survey of the results of different surgical approaches. Dis Colon Rectum. 2002. 45:1458–1467.21. Popeskou S, Christoforidis D, Ruffieux C, Demartines N. Wound infection after excision and primary midline closure for pilonidal disease: risk factor analysis to improve patient selection. World J Surg. 2011. 35:206–211.22. Akinci OF, Coskun A, Uzunköy A. Simple and effective surgical treatment of pilonidal sinus: asymmetric excision and primary closure using suction drain and subcuticular skin closure. Dis Colon Rectum. 2000. 43:701–706.23. McCallum IJ, King PM, Bruce J. Healing by primary closure versus open healing after surgery for pilonidal sinus: systematic review and meta-analysis. BMJ. 2008. 336:868–871.24. Can MF, Sevinc MM, Hancerliogullari O, Yilmaz M, Yagci G. Multicenter prospective randomized trial comparing modified Limberg flap transposition and Karydakis flap reconstruction in patients with sacrococcygeal pilonidal disease. Am J Surg. 2010. 200:318–327.25. Ewing JA, Rouse BA. Hirsutism, race and testosterone levels: comparison of East Asians and Euroamericans. Hum Biol. 1978. 50:209–215.26. Obesity: preventing and managing the global epidemic. Report of a WHO consultation. World Health Organ Tech Rep Ser. 2000. 894:i–xii. 1–253.27. Wen CP, David Cheng TY, Tsai SP, Chan HT, Hsu HL, Hsu CC, et al. Are Asians at greater mortality risks for being overweight than Caucasians? Redefining obesity for Asians. Public Health Nutr. 2009. 12:497–506.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Removal Skin Tumors of 4 Cases by Using the Modified S-plasty
- Clinical Evaluation of Wide Excision and Simple Primary Closure of Pilonidal Sinus
- A Case of Pilonidal Sinus Mimicking Inflammatory Epidermal Cyst
- Comparative analysis of the same technique-the same surgeon approach in the surgical treatment of pilonidal sinus disease: a retrospective cohort study
- Specimen index may be a predictive factor for recurrence after primary closure of pilonidal disease