Yonsei Med J.
2007 Feb;48(1):90-96. 10.3349/ymj.2007.48.1.90.
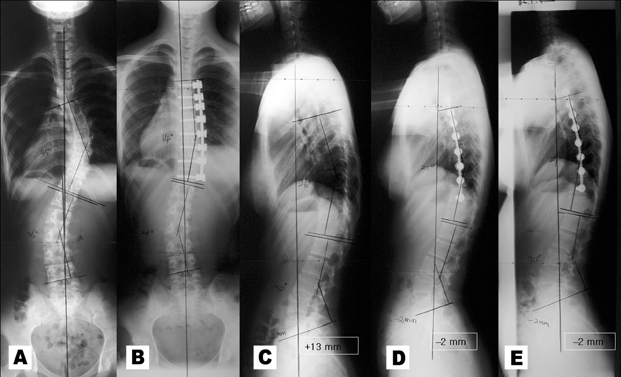
Sagittal Plane Analysis of Adolescent Idiopathic Scoliosis after VATS (Video-Assisted Thoracoscopic Surgery) Anterior Instrumentations
- Affiliations
-
- 1Department of Orthopaedic Surgery, Young-Dong Severance Hospital, Yonsei University College of Medicine, Seoul, Korea. os3410@yumc.yonsei.ac.kr
- 2Department of Orthopaedic Surgery, Samsung Medical Center, Sungkyunkwan University, Seoul, Korea.
- KMID: 1093528
- DOI: http://doi.org/10.3349/ymj.2007.48.1.90
Abstract
- Radiographic sagittal plane analysis of VATS (video-assisted thoracoscopic surgery) anterior instrumentation for adolescent idiopathic scoliosis. This is retrospective study. To report, in details about effects of VATS anterior instrumentation on the sagittal plane. Evaluations of the surgical outcome of scoliosis have primarily studied in coronal plane correction, functional, and cosmetic aspects. Sagittal balance, as well as coronal balance, is important in functional spine. Recently, scoliosis surgery applying VATS has been increasingly performed. Its outcome has been reported several times; however, according to our search of the literature, the only one study partially mentioned. The study population was a total of 42 cases of idiopathic scoliosis patients (8 male, 34 female). Their mean age was 15.6 years (13 to 18 years). The 18 cases were Lenke IA type, 16 cases were Lenke IB type, and 8 cases were Lenke IC type. The preoperative Cobb's angle was 54.5 +/- 13.9 degrees. All patients were followed up for a minimum of 2 years and implanted, on average, at the 5.9 level (5 to 8 levels). The most proximal implant was the 4th thoracic spine, and the most distal implant was the 1st lumbar spine. Whole spine standing PA and lateral radiographs were taken before surgery, 2 months after surgery, and at the last follow up (range 24-48 months, mean 35 months). The C7 plumbline proximal junctional measurement (PJM), distal junctional measurement (DJM), thoracic kyphosis, and lumbar lordosis angles were measured and compared. In all cases, follow-ups were possible and survived till the last follow up. The Cobb's angle in coronal plane at the last follow up was 19.7 +/- 9.3 degrees and was corrected to 63.8% on average. The preoperative C7 sagittal plumbline before surgery was -13.9 +/- 29.1mm, the final follow up was -9.9 +/- 23.8mm, and the average positive displacement was 4mm. Thoracic kyphosis was increased from preoperative 18.2 +/- 7.7 degrees to 22.4 +/- 7.2 degrees on average at the last follow up, and the increase was, on average, 4.2 degrees. The PJM angel was increased from 6.2 +/- 4.3 degrees preoperative to 8.8 +/- 3.7 degrees at the last follow up, and the increment was, on the average, 2.6 degrees. The DJM angle before surgery was 6.8 +/- 5.1 degrees and 6.7 +/- 4 degrees at the last follow up, and did not change noticeably. Preoperative lumbar lordosis was 42 +/- 10.7 degrees and 43.5 +/- 11.1 degrees after surgery. Similarly, it did not change greatly. The scoliosis surgery applying VATS displaced the C7 sagittal plumb line by 4mm to the anteriorly, increased thoracic kyphosis by 4.2 degrees, and increased PJM by 2.6 degrees. DJM and lumbar lordosis, before and after operation, were not significantly different. Although the surgical technique of VATS thoracic instrumentation is difficult to make the normal thoracic kyphosis, an acceptable sagittal balance can be obtained in Lenke type I adolescent idiopathic scoliosis using VATS.
Keyword
Figure
Cited by 2 articles
-
Video-Assisted Thoracoscopic Surgery for Correction of Adolescent Idiopatic Scoliosis: Comparison of 4.5 mm versus 5.5 mm Rod Constructs
Hak Sun Kim, Jin Oh Park, Ankur Nanda, Phillip Anthony Kho, Jin Young Kim, Hwan Mo Lee, Seong Hwan Moon, Jung Won Ha, Eun Kyoung Ahn, Dong Eun Shin, Sung Jun Kim, Eun Su Moon
Yonsei Med J. 2010;51(5):753-760. doi: 10.3349/ymj.2010.51.5.753.Polyaxial Screws with Thick Rod versus Monoaxial Screws with Thin Rod in Video-Assisted Thoracoscopic Scoliosis Surgery (VATS)
Hak Sun Kim, Ju Young Kim, Jin Oh Park, Seong Hwan Moon, Hwan Mo Lee, Jung Won Ha, Ho Joong Kim, Huan Wei, Su Keon Lee, Eun Su Moon
J Korean Soc Spine Surg. 2008;15(1):9-17. doi: 10.4184/jkss.2008.15.1.9.
Reference
-
1. De Jonge T, Dubousset JF, Illes T. Sagittal plane correction in idiopathic scoliosis. Spine. 2002. 27:754–760.
Article2. Rhee JM, Bridwell KH, Won DS, Lenke LG, Chotigavanichaya C, Hanson DS. Sagittal plane analysis of adolescent idiopathic scoliosis: the effect of anterior versus posterior instrumentation. Spine. 2002. 27:2350–2356.
Article3. Bridwell KH, Betz R, Capelli AM, Huss G, Harvey C. Sagittal plane analysis in idiopathic scoliosis patients treated with Cotrel-Dubousset instrumentation. Spine. 1990. 15:921–926.
Article4. Mac-Thiong JM, Labelle H, Charlebois M, Huot MP, de Guise JA. Sagittal plane analysis of the spine and pelvis in adolescent idiopathic scoliosis according to the coronal curve type. Spine. 2003. 28:1404–1409.
Article5. Betz RR, Harms J, Clements DH 3rd, Lenke LG, Lowe TG, Shufflebarger HL, et al. Comparison of anterior and posterior instrumentation for correction of adolescent thoracic idiopathic scoliosis. Spine. 1999. 24:225–239.
Article6. Vedantam R, Lenke LG, Bridwell KH, Linville DL, Blanke K. The effect of variation in arm position on sagittal spinal alignment. Spine. 2000. 25:2204–2209.
Article7. Lenke LG, Newton PO, Marks MC, Blanke KM, Sides B, Kim YJ, et al. Prospective pulmonary function comparison of open versus endoscopic anterior fusion combined with posterior fusion in adolescent idiopathic scoliosis. Spine. 2004. 29:2055–2060.
Article8. Newton PO, Marks M, Faro F, Betz R, Clements D, Haher T, et al. Use of video-assisted thoracoscopic surgery to reduce perioperative morbidity in scoliosis surgery. Spine. 2003. 28:S249–S254.
Article9. Picetti GD 3rd, Ertl JP, Bueff HU. Endoscopic instrumentation, correction, and fusion of idiopathic scoliosis. Spine J. 2001. 1:190–197.
Article10. Newton PO, Shea KG, Granlund KF. Defining the pediatric spinal thoracoscopy learning curve: sixty-five consecutive cases. Spine. 2000. 25:1028–1035.
Article11. Kim HS, Choi YR, Lee HM, Moon SH, Kim KH, Park JO, et al. Learning curve for the thoracoscopic correction of spinal deformities. J Korean Soc Spine Surg. 2003. 10:261–268.
Article12. Lee GA, Betz RR, Clements DH 3rd, Huss GK. Proximal kyphosis after posterior spinal fusion in patients with idiopathic scoliosis. Spine. 1999. 24:795–799.
Article13. Bernhardt M, Bridwell KH. Segmental analysis of the sagittal plane alignment of the normal thoracic and lumbar spines and thoracolumbar junction. Spine. 1989. 14:717–721.
Article14. Sweet FA, Lenke LG, Bridwell KH, Blanke KM. Maintaining lumbar lordosis with anterior single solid-rod instrumentation in thoracolumbar and lumbar adolescent idiopathic scoliosis. Spine. 1999. 24:1655–1662.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Video-Assisted Thoracoscopic Surgery Plus Lumbar Mini-Open Surgery for Adolescent Idiopathic Scoliosis
- Management of Complications During Video-Assisted Thoracic Surgery Lung Resection and Lymph Node Dissection
- Polyaxial Screws with Thick Rod versus Monoaxial Screws with Thin Rod in Video-Assisted Thoracoscopic Scoliosis Surgery (VATS)
- Video-assisted thoracoscopic lobectomy for lung cancer
- Sagittal Plane Lumbar Responses after Anterior Selective Thoracic Fusion for Main Thoracic Adolescent Idiopathic Scoliosis