Korean J Radiol.
2011 Feb;12(1):25-33. 10.3348/kjr.2011.12.1.25.
Collateral Ventilation to Congenital Hyperlucent Lung Lesions Assessed on Xenon-Enhanced Dynamic Dual-Energy CT: an Initial Experience
- Affiliations
-
- 1Department of Radiology and the Research Institute of Radiology, Asan Medical Center, University of Ulsan College of Medicine, Seoul 138-736, Korea. hwgoo@amc.seoul.kr
- 2Department of Thoracic and Cardiovascular Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul 138-736, Korea.
- 3Department of Neonatology, Asan Medical Center, University of Ulsan College of Medicine, Seoul 138-736, Korea.
- KMID: 991679
- DOI: http://doi.org/10.3348/kjr.2011.12.1.25
Abstract
OBJECTIVE
We wanted to evaluate the resistance to collateral ventilation in congenital hyperlucent lung lesions and to correlate that with the anatomic findings on xenon-enhanced dynamic dual-energy CT.
MATERIALS AND METHODS
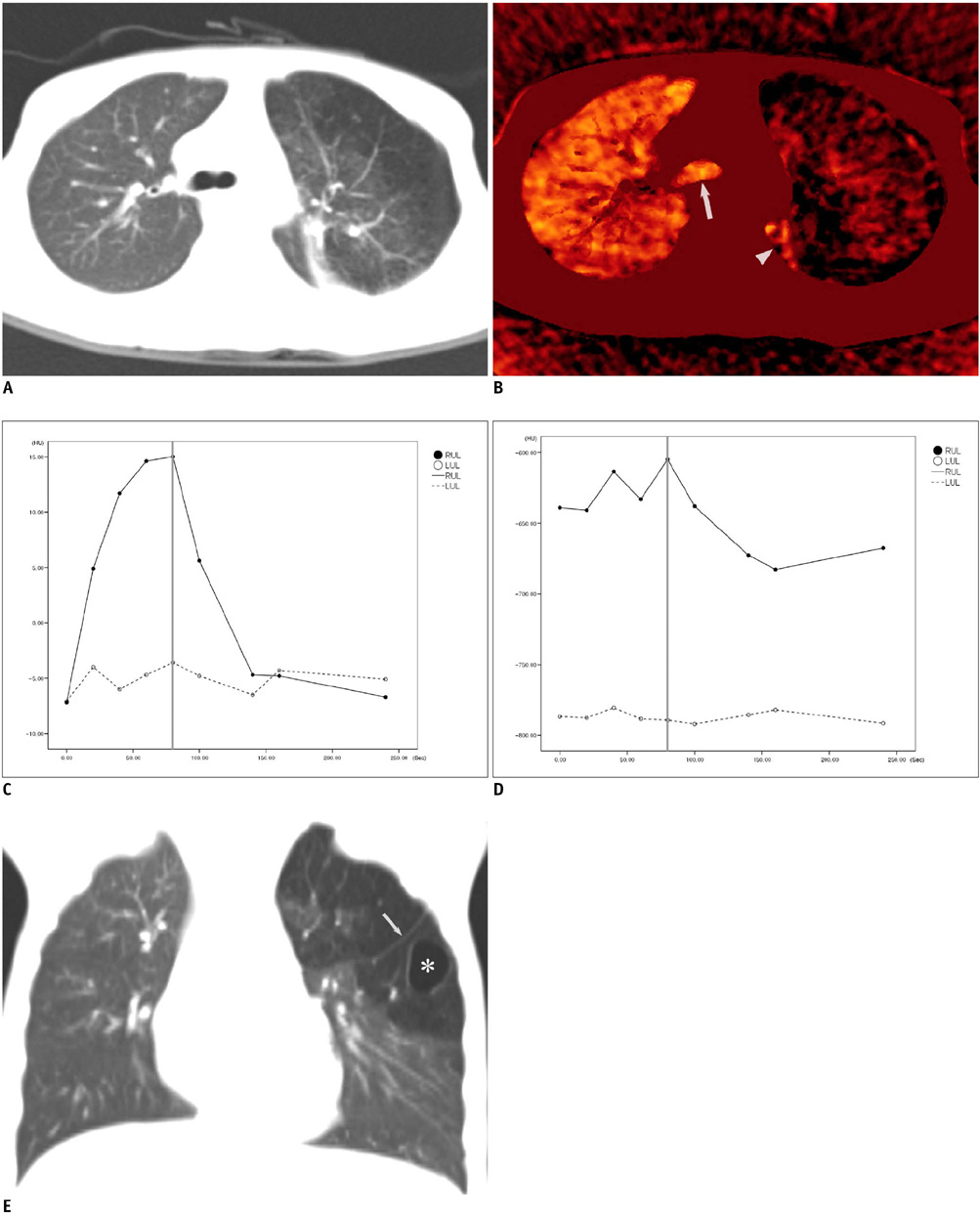
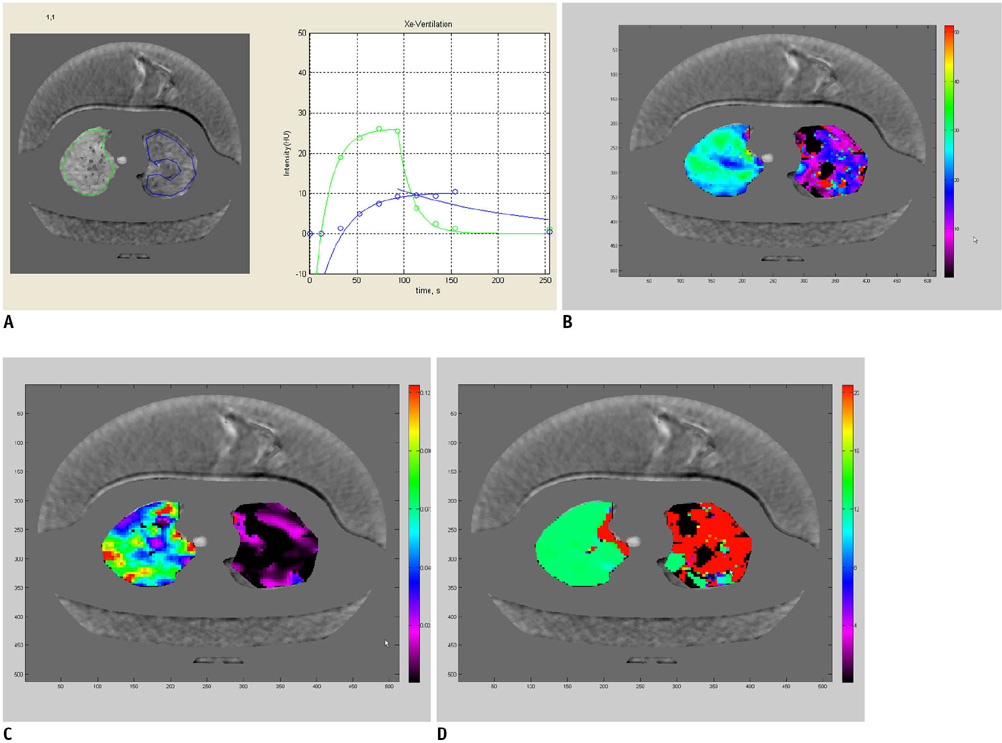
Xenon-enhanced dynamic dual-energy CT was successfully and safely performed in eight children (median age: 5.5 years, 4 boys and 4 girls) with congenital hyperlucent lung lesions. Functional assessment of the lung lesions on the xenon map was done, including performing a time-xenon value curve analysis and assessing the amplitude of xenon enhancement (A) value, the rate of xenon enhancement (K) value and the time of arrival value. Based on the A value, the lung lesions were categorized into high or low (A value > 10 Hounsfield unit [HU]) resistance to collateral ventilation. In addition, the morphologic CT findings of the lung lesions, including cyst, mucocele and an accessory or incomplete fissure, were assessed on the weighted-average CT images. The xenon-enhanced CT radiation dose was estimated.
RESULTS
Five of the eight lung lesions were categorized into the high resistance group and three lesions were categorized into the low resistance group. The A and K values in the normal lung were higher than those in the low resistance group. The time of arrival values were delayed in the low resistance group. Cysts were identified in five lesions, mucocele in four, accessory fissure in three and incomplete fissure in two. Either cyst or an accessory fissure was seen in four of the five lesions showing high resistance to collateral ventilation. The xenon-enhanced CT radiation dose was 2.3 +/- 0.6 mSv.
CONCLUSION
Xenon-enhanced dynamic dual-energy CT can help visualize and quantitate various degrees of collateral ventilation to congenital hyperlucent lung lesions in addition to assessing the anatomic details of the lung.
Keyword
MeSH Terms
Figure
Cited by 2 articles
-
An Engineering View on Megatrends in Radiology: Digitization to Quantitative Tools of Medicine
Namkug Kim, Jaesoon Choi, Jaeyoun Yi, Seungwook Choi, Seyoun Park, Yongjun Chang, Joon Beom Seo
Korean J Radiol. 2013;14(2):139-153. doi: 10.3348/kjr.2013.14.2.139.Dual-Energy CT: New Horizon in Medical Imaging
Hyun Woo Goo, Jin Mo Goo
Korean J Radiol. 2017;18(4):555-569. doi: 10.3348/kjr.2017.18.4.555.
Reference
-
1. Lee EY, Boiselle PM, Cleveland RH. Multidetector CT evaluation of congenital lung anomalies. Radiology. 2008. 247:632–648.2. Chae EJ, Seo JB, Goo HW, Kim N, Song KS, Lee SD, et al. Xenon ventilation CT with a dual-energy technique of dual-source CT: initial experience. Radiology. 2008. 248:615–624.3. Goo HW, Yang DH, Hong SJ, Yu J, Kim BJ, Seo JB, et al. Xenon ventilation CT using dual-source and dual-energy technique in children with bronchiolitis obliterans: correlation of xenon and CT density values with pulmonary function test results. Pediatr Radiol. 2010. 40:1490–1497.4. Goo HW, Chae EJ, Seo JB, Hong SJ. Xenon ventilation CT using a dual-source dual-energy technique: dynamic ventilation abnormality in a child with bronchial atresia. Pediatr Radiol. 2008. 38:1113–1116.5. Chae EJ, Seo JB, Lee J, Kim N, Goo HW, Lee HJ, et al. Xenon ventilation imaging using dual-energy computed tomography in asthmatics: initial experience. Invest Radiol. 2010. 45:354–361.6. Kang MJ, Park CM, Lee CH, Goo JM, Lee HJ. Dual-energy CT: clinical applications in various pulmonary diseases. Radiographics. 2010. 30:685–698.7. Park EA, Goo JM, Park SJ, Lee HJ, Lee CH, Park CM, et al. Chronic obstructive pulmonary disease: quantitative and visual ventilation pattern analysis at xenon ventilation CT performed by using a dual-energy technique. Radiology. 2010. 256:985–997.8. Kosuda S, Kadota Y, Kusano S, Sekine I. A combined study of Tc-99m Technegas and Xe-133 gas in suspected congenital bronchial atresia. Clin Nucl Med. 2003. 28:243–244.9. Kamata S, Usui N, Kamiyama M, Nose K, Sawai T, Fukuzawa M. Long-term outcome in patients with prenatally diagnosed cystic lung disease: special reference to ventilation and perfusion scan in the affected lung. J Pediatr Surg. 2006. 41:2023–2027.10. Suga K, Hara A, Matsumoto T, Matsunaga N. Intralobar bronchopulmonary sequestration: evidence of air trapping shown by dynamic xenon-133 SPECT. Br J Radiol. 2001. 74:657–661.11. Yang DH, Goo HW. Pediatric 16-slice CT protocols: radiation dose and image quality. J Korean Radiol Soc. 2008. 59:333–347.12. Cetti EJ, Moore AJ, Geddes DM. Collateral ventilation. Thorax. 2006. 61:371–373.13. Kety SS. The theory and applications of the exchange of inert gas at the lungs and tissues. Pharmacol Rev. 1951. 3:1–41.14. Chae EJ, Seo JB, Kim N, Song KS, Shin JH, Kim TH, et al. Collateral ventilation in a canine model with bronchial obstruction: assessment with xenon-enhanced dual-energy CT. Radiology. 2010. 255:790–798.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Collateral Ventilation Quantification Using Xenon-Enhanced Dynamic Dual-Energy CT: Differences between Canine and Swine Models of Bronchial Occlusion
- Redistributed Regional Ventilation after the Administration of a Bronchodilator Demonstrated on Xenon-Inhaled Dual-Energy CT in a Patient with Asthma
- Visual and Quantitative Assessments of Regional Xenon-Ventilation Using Dual-Energy CT in Asthma-ChronicObstructive Pulmonary Disease Overlap Syndrome:A Comparison with Chronic Obstructive PulmonaryDisease
- Dual-Energy CT: New Horizon in Medical Imaging
- Bronchogenic carcinoma manifesting unilateral hyperlucent lung: CT features