Korean J Lab Med.
2009 Apr;29(2):140-144. 10.3343/kjlm.2009.29.2.140.
A Case of Disseminated Melioidosis in a Migrant Worker from Thailand
- Affiliations
-
- 1Department of Internal Medicine, Chung-Ang University College of Medicine, Seoul, Korea. drjwchung@cau.ac.kr
- 2Department of Laboratory Medicine, Chung-Ang University College of Medicine, Seoul, Korea.
- 3Division of Epidemic Intelligence Service, Korea Centers for Disease Control and Prevention, Seoul, Korea.
- KMID: 854972
- DOI: http://doi.org/10.3343/kjlm.2009.29.2.140
Abstract
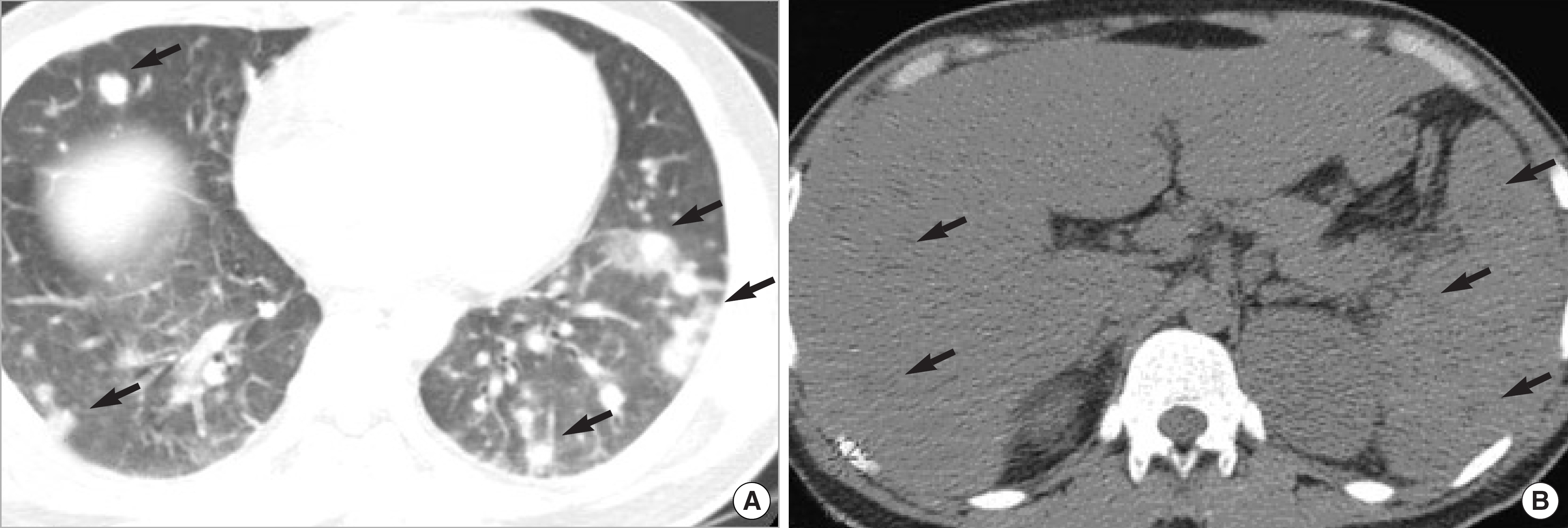
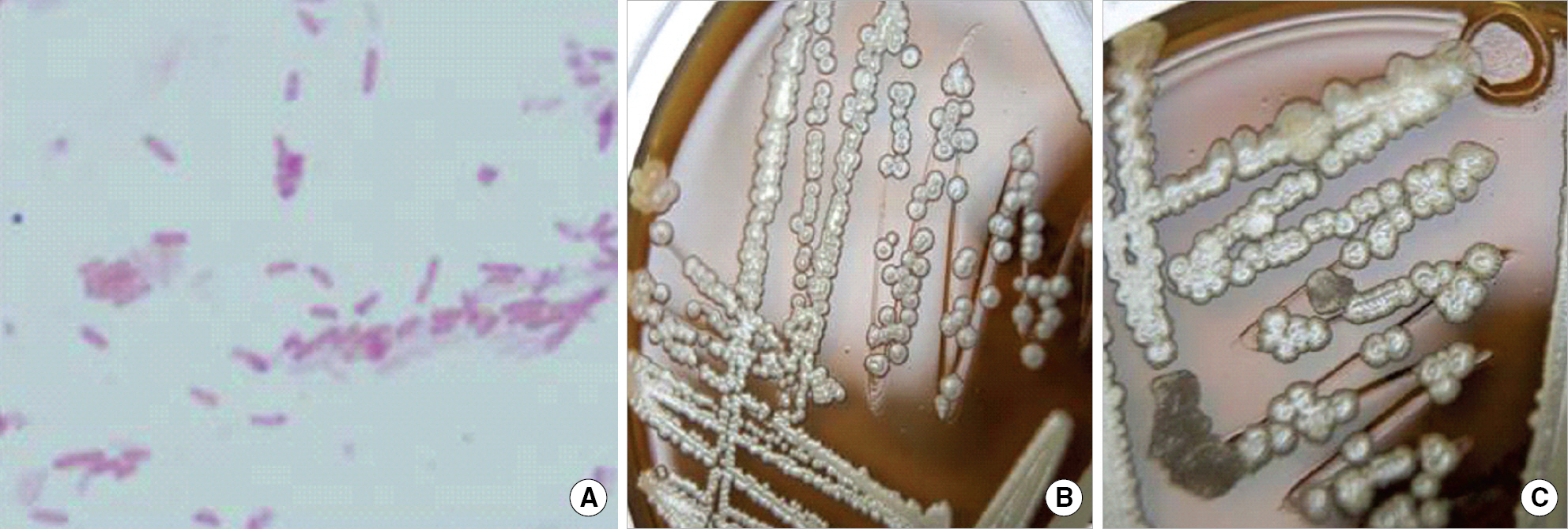
- With globalization, foreign patients are frequently encountered at the clinical practice in Korea. As the number of migrant workers from Southeast Asia has been notably rising since the late 1990's, unfamiliar tropical infectious diseases that they bring out, may give great challenges to the routine clinical practice in Korea. Melioidosis is a community-acquired infection caused by a gram-negative bacillus, Burkholderia pseudomallei. It has been endemic in Southeast Asia and Northern Australia, where B. pseudomallei is a soil saprophyte and invades the host through inoculation or inhalation. It frequently presents as an acute septicemia with a high mortality rate of 40%, mainly in patients with chronic underlying diseases, such as diabetes mellitus. Recently, we encountered a case of fatal disseminated melioidosis in a migrant worker from Thailand. We suggest an importance of melioidosis as a cause of community-acquired sepsis in migrant workers from Southeast Asia.
MeSH Terms
Figure
Cited by 3 articles
-
Septicemic Melioidosis Presenting as Head and Neck Abscesses
So Yeon Park, Cheol-In Kang, Eun-Jeong Joo, Young Eun Ha, Chang-Seok Ki, Nam Yong Lee, Doo Ryeon Chung, Kyong Ran Peck, Jae-Hoon Song
Infect Chemother. 2012;44(4):315-318. doi: 10.3947/ic.2012.44.4.315.A Case of Ceftazidime-Nonsusceptible Burkholderia pseudomallei Infection
Eunkyoung You, Mi Jeong Seo, Young Jin Kim, Myung Jae Park, Hee Joo Lee
Lab Med Online. 2015;5(4):219-222. doi: 10.3343/lmo.2015.5.4.219.The Laboratory Diagnosis of Melioidosis in a Korean Patient
Yong-Woo Shin, Min-Hee Cho, Jeong-Hoon Chun, Changmu Kim, Hee-Bok Oh, Gi-Eun Rhie, Cheon-Kwon Yoo
J Bacteriol Virol. 2011;41(1):19-25. doi: 10.4167/jbv.2011.41.1.19.
Reference
-
1.Song JH. Travel medicine: prevention of infectious diseases during travel. Korean J Intern Med. 2000. 59:254–60. (송재훈. 여행의학: 해외여행시의감염예방. 대한내과학회지 2000;59: 254-60.).2.Korea National Statistical Office. International statistics yearbook: Korea National Statistical Office. 2008. 80. (통계청.국제통계연감.2008:80. ).3.Cheng AC., Currie BJ. Melioidosis: epidemiology, pathophysiology, and management. Clin Microbiol Rev. 2005. 18:383–416.
Article4.White NJ., Dance DA., Chaowagul W., Wattanagoon Y., Wuthiekanun V., Pitakwatchara N. Halving of mortality of severe melioidosis by ceftazidime. Lancet. 1989. 2:697–701.
Article5.Seok HJ., Kim JI., Lee JH., Choo EJ., Kwak YG., Jang SS, et al. A case of septicemia and septic pneumonia due to Burkholderia pseudomallei. Infect Chemother. 2004. 36:114–7. (석현정, 김재일, 이장한, 추은주, 곽이경, 장성수등. Burkholderia pseudomallei에의한균혈증과패혈폐렴 1예. 감염과화학요법 2004;36: 114-7.).6.Lee SW., Yi J., Joo SI., Kang YA., Yoon YS., Yim JJ, et al. A case of melioidosis presenting as migrating pulmonary infiltration: the first case in Korea. J Korean Med Sci. 2005. 20:139–42.
Article7.Clinical and Laboratory Standards Institute. Performance standards for antimicrobial susceptibility testing; eighteenth informational supplement. M100-S18. Wayne, PA: CLSI;2008.8.Whitmore A., Krishnaswami CS. An account of the discovery of a hitherto undescribed infective disease occurring among the population of Rangoon. Ind Med Gaz. 1912. 47:262–7.9.Stanton AT., Fletcher W. Melioidosis, a new disease of the tropics. Trans Fourth Congress Far East Assoc Trop Med. 1921. 2:196–8.10.Division of Epidemic Intelligence Service, Korea Centers for Disease Control and Prevention. Public Health Weekly Report. 2008. 1:504–5. (질병관리본부 전염병대응센터 역학조사팀. 유비저에 의한 사망사례역학조사최종결과. 주간건강과질병 2008;1: 504-5.).11.White NJ. Melioidosis. Lancet. 2003. 361:1715–22.
Article12.Currie BJ. Burkholderia pseudomallei and Burkholderia mallei: melioidosis and glanders. Mandell G, Bennet JE, editors. Principles and practices of infectious diseases. 6th ed.Philadelphia: Elsevier;2005. p. 2622–32.13.Gan YH. Interaction between Burkholderia pseudomallei and the host immune response: sleeping with the enemy? J Infect Dis. 2005. 192:1845–50.14.Siegel JD, Rhinehart E, Jackson M, Chiarello L, the Healthcare Infection Control Practices Advisory Committee. Guideline for isolation precautions: preventing transmission of infectious agents in healthcare settings. 2007. http://www.cdc.gov/ncidod/dhqp/pdf/guidelines/Isolation2007.pdf. (last opened Mar 06. 2009).15.Centers for Disease Control and Prevention (CDC). Laboratory exposure to Burkholderia pseudomallei-Los Angeles, California, 2003. MMWR Morb Mortal Wkly Rep. 2004. 53:988–90.16.Peacock SJ., Schweizer HP., Dance DA., Smith TL., Gee JE., Wuthiekanun V, et al. Management of accidental laboratory exposure to Burkholderia pseudomallei and B. mallei. Emerg Infect Dis. 2008. 14:e2.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical and Imaging Findings of Musculoskeletal Melioidosis in the Right Hip: A Case Report
- Factors Influencing Level of Health Literacy of Migrant Workers in Korea
- The Results of Survey for Hansen's Disease of the Migrant Worker
- Septicemic Melioidosis Presenting as Head and Neck Abscesses
- Epidemiological Aspects of Imported Melioidosis in Korea and Japan, 2011 to 2020