Korean J Radiol.
2003 Sep;4(3):163-169. 10.3348/kjr.2003.4.3.163.
A Comparative Experimental Study of the, In-vitro Efficiency of Hypertonic, Saline-Enhanced Hepatic Bipolar and, Monopolar Radiofrequency Ablation
- Affiliations
-
- 1Department of Radiology, Seoul National University College of Medicine; Institute of Radiation Medicine, SNUMRC (Seoul National University Medical Research Center) ; Clinical Research Institute, Seoul National University Hospital. leejm@radcom.snu.ac.kr
- KMID: 754020
- DOI: http://doi.org/10.3348/kjr.2003.4.3.163
Abstract
OBJECTIVE
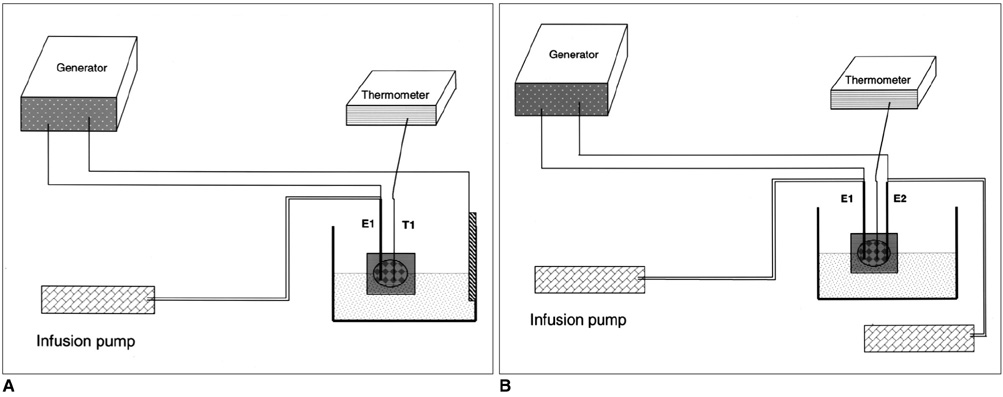
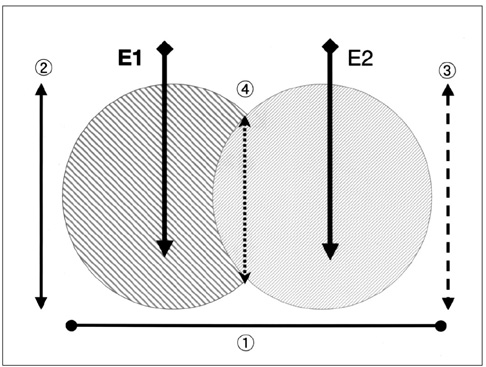
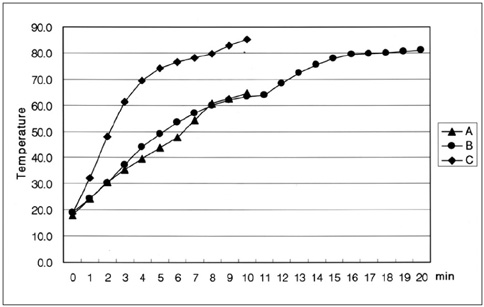
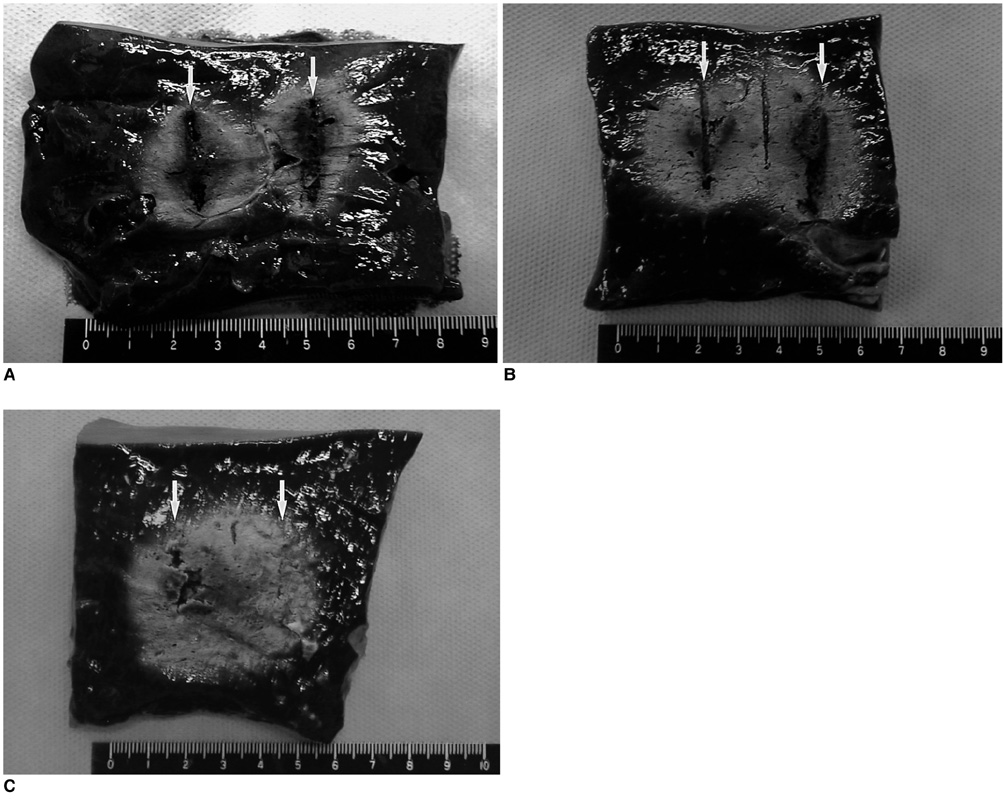
To compare the in-vitro efficiency of a hypertonic saline (HS) -enhanced bipolar radiofrequency (RF) system with monopolar RF applications by assessing the temperature profile and dimensions of RF-created coagulation necrosis in bovine liver. MATERIALS AND METHODS: A total of 27 ablations were performed in explanted bovine livers. After placement of two 16-gauge open-perfused electrodes at an interelectrode distance of 3 cm, 5% HS was instilled into tissue at a rate of 1 mL/min through the electrode. Seventeen thermal ablation zones were created in the monopolar mode (groups A, B), and ten more were created using the two open-perfused electrodes in the bipolar mode (group C). RF was applied to each electrode for 5 mins (for a total of 10 mins, group A) or 10 mins (for a total of 20 mins, group B) at 50W in the sequential monopolar mode, or to both electrodes for 10 min in the bipolar mode (group C). During RF instillation, we measured tissue temperature at the midpoint between the two electrodes. The dimensions of the thermal ablation zones and changes in impedance and wattage during RFA were compared between the groups. RESULTS: With open-perfusion electrodes, the mean accumulated energy output value was lower in the bipolar mode (group C: 26675+/-3047 Watt's) than in the monopolar mode (group A: 28778+/-1300 Watt's) but the difference was not statistically significant (p > 0.05). In the bipolar mode, there were impedance rises of more than 700 omega during RF energy application, but in the monopolar modes, impedance did not changed markedly. In the bipolar mode, however, the temperature at the mid-point between the two probes was higher (85degrees C) than in the monopolar modes (65degrees C, 80degrees C for group A, B, respectively) (p < 0.05). In addition, in HS-enhanced bipolar RFA (group C), the shortest diameter at the midpoint between the two electrodes was greater than in either of the monopolar modes: 5.4+/-5.6 mm (group A) ; 28.8+/-8.2 mm (group B) ; 31.2+/-7.6 mm (group C) (p < 0.05) CONCLUSION: Using an open perfusion system, HS-enhanced bipolar RFA more efficiently created larger areas of thermal ablation and higher tissue temperatures than monopolar RFA.
Figure
Reference
-
1. Goldberg SN, Gazelle GS, Solbiati L, Livraghi T. State of the art: tumor ablation with radio-frequency energy. Radiology. 2000. 217:633–646.2. McGahan JP, Dodd GD. Radiofrequency ablation of the liver: current status. AJR Am J Roentgenol. 2001. 176:3–16.3. Solbiati L, Livraghi T, Goldberg SN, et al. Percutaneous radiofrequency ablation of hepatic metastases from colorectal cancer: long-term results in 117 patients. Radiology. 2001. 221:159–166.4. Lim HK. Radiofrequency thermal ablation of hepatocellular carcinomas. Korean J Radiol. 2000. 1:175–184.5. Livraghi T, Goldberg SN, Lazzaroni S, et al. Hepatocellular carcinoma: radiofrequency ablation of medium and large lesions. Radiology. 2000. 214:761–768.6. de Baere T, Elias D, Dromain C, et al. Radiofrequency ablation of 100 hepatic metastases with a mean follow-up of more than one year. AJR Am J Roentgenol. 2000. 175:1619–1625.7. Dodd GD, Soulen MC, Kane RA, et al. Minimally invasive treatment of malignant hepatic tumors: at the threshold of a major breakthrough. RadioGraphics. 2000. 20:9–27.8. Goldberg SN, Stein M, Gazelle GS, Sheiman RG, et al. Percutaneous radiofrequency tissue ablation: optimization of pulsed-RF technique to increase coagulation necrosis. J Vasc Interv Radiol. 1999. 10:907–916.9. Goldberg SN, Gazelle GS, Mueller PR. Thermal ablation therapy for focal malignancy: a unified approach to underlying principles, techniques and diagnostic imaging guidance. AJR Am J Roentgenol. 2000. 174:323–331.10. Lee JM, Kim YK, Lee YH, Kim SW, Li CA, Kim CS. Percutaneous radiofrequency thermal ablation with hypertonic saline injection: in-vivo study in a rabbit liver model. Korean J Radiol. 2003. 4:27–34.11. Munver R, Threatt CB, Delvecchio FC, Preminger GM, Polascik TJ. Hypertonic saline-augmented radiofrequency ablation of VX2 tumor implanted in rabbit kidney: a short-term survival pilot study. Urology. 2002. 60:170–175.12. Goldberg SN, Ahmed M, Gazelle GS, et al. Radiofrequency thermal ablation with NaCl solution injection: effect of electrical conductivity on tissue heating, and coagulation-phantom and porcine liver study. Radiology. 2001. 219:157–165.13. McGahan JP, Gu WZ, Brock JM, Tesluk H, Jones CD. Hepatic ablation using bipolar radiofrequency electrocautery. Acad Radiol. 1996. 3:418–422.14. Curley SA, Davidson BS, Fleming RY, et al. Laparoscopically guided bipolar radiofrequency ablation of areas of porcine liver. Surg Endosc. 1997. 11:729–733.15. Goldberg SN, Hahn PF, Halpern E, et al. Radiofrequency tissue ablation: effect of pharmacologic modulation of blood flow on coagulation diameter. Radiology. 1998. 209:761–769.16. Patterson EJ, Scudamore CH, et al. Radiofrequency ablation of porcine liver in vivo: effects of blood flow and treatment time on lesion size. Ann Surg. 1998. 227:559–565.17. Lee JD, Lee JM, Kim SW, Kim CS, Mun WS. MR imaging-histopathologic correlation of radiofrequency thermal ablation lesion in a rabbit liver model: observation during acute and chronic stages. Korean J Radiol. 2001. 2:151–158.18. Motulsky H. Motulsky Harvey, editor. Comparing three or more means: analysis of variance. Intuitive Biostatistics. 1995. 1st ed. NY: Oxford University Press Inc.;155–261.19. Burdio F, Guemes A, Burdio JM, et al. Hepatic lesion ablation with bipolar saline-enhanced radiofrequency in the audible spectrum. Acad Radiol. 1999. 6:680–686.20. Haemmerich D, Tungjitkusolmun S, Staelin ST, Lee FT, Mahvi DM, Webster JG. Finite-element analysis of hepatic multiple probe radio-frequency ablation. IEEE Trans BioMed Eng. 2002. 49:836–842.21. Haemmerich D, Staelin ST, Tungjitkusolmun S, Lee FT, Mahvi DM, Webster JG. Hepatic bipolar radiofrequency ablation between separated multiprong electrodes. IEEE Trans BioMed Eng. 2001. 48:1145–1152.22. Jang IS, Rhim H, Koh BH, et al. An experimental study of simultaneous ablation with dual probes in radiofrequency thermal ablation. J Korean Radiol Soc. 2003. 48:163–169. (in Korean).
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Saline-Enhanced Hepatic Radiofrequency Ablation Using a Perfused-Cooled Electrode: Comparison of Dual Probe Bipolar Mode with Monopolar and Single Probe Bipolar Modes
- Hepatic Radiofrequency Ablation Using Multiple Probes: Ex Vivo and In Vivo Comparative Studies of Monopolar versus Multipolar Modes
- Radio Frequency Ablation in the Rabbit Lung Using Wet Electrodes: Comparison of Monopolar and Dual Bipolar Electrode Mode
- Comparison of Wet Radiofrequency Ablation with Dry Radiofrequency Ablation and Radiofrequency Ablation Using Hypertonic Saline Preinjection: Ex Vivo Bovine Liver
- Monopolar Radiofrequency Ablation Using a Dual-Switching System and a Separable Clustered Electrode: Evaluation of the In Vivo Efficiency