Korean J Radiol.
2006 Jun;7(2):106-117. 10.3348/kjr.2006.7.2.106.
Hepatic Radiofrequency Ablation Using Multiple Probes: Ex Vivo and In Vivo Comparative Studies of Monopolar versus Multipolar Modes
- Affiliations
-
- 1Department of Radiology, and Institute of Radiation Medicine, Seoul National University College of Medicine, Clinical Research Institute, Seoul National University Hospital, Seoul, Korea. HANJK@RADCOM.SNU.AC.KR
- KMID: 1782183
- DOI: http://doi.org/10.3348/kjr.2006.7.2.106
Abstract
OBJECTIVE
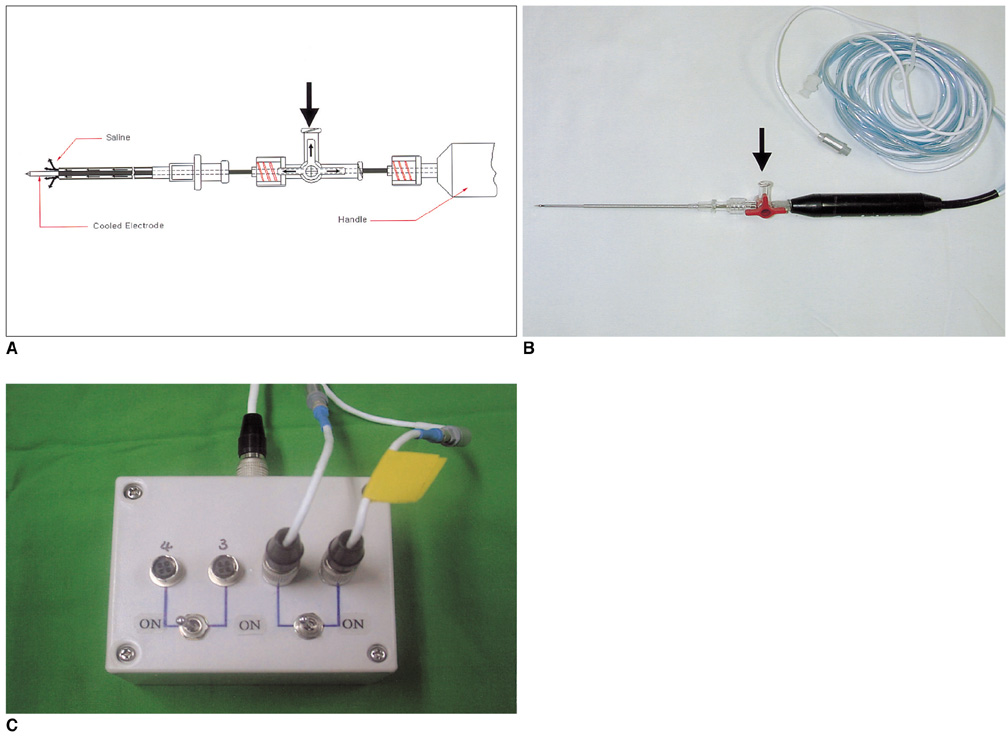
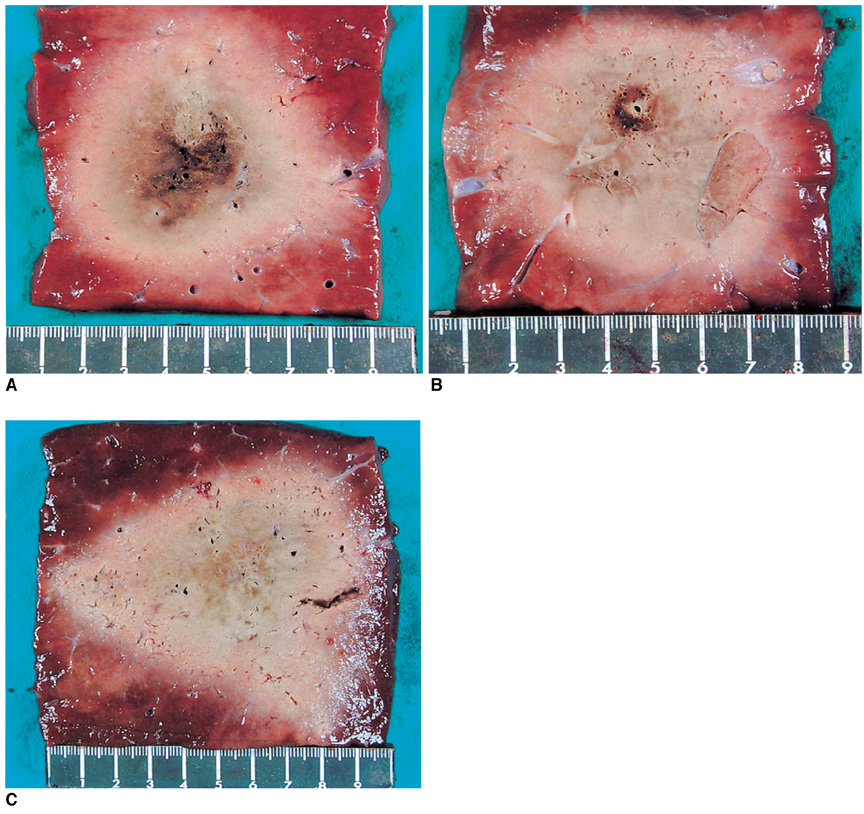
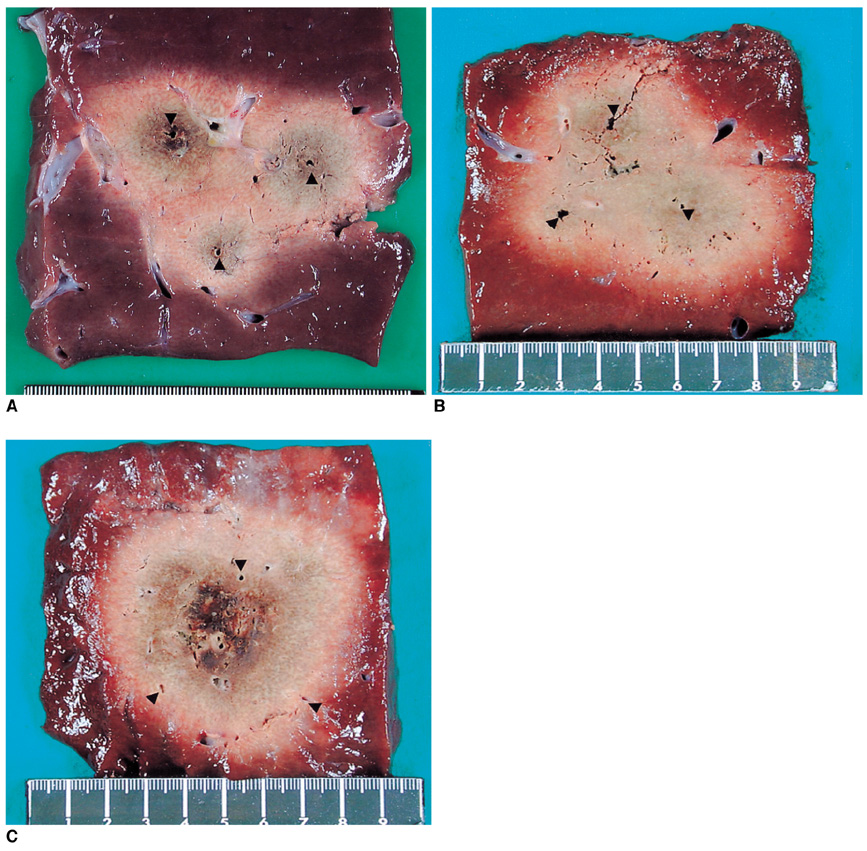
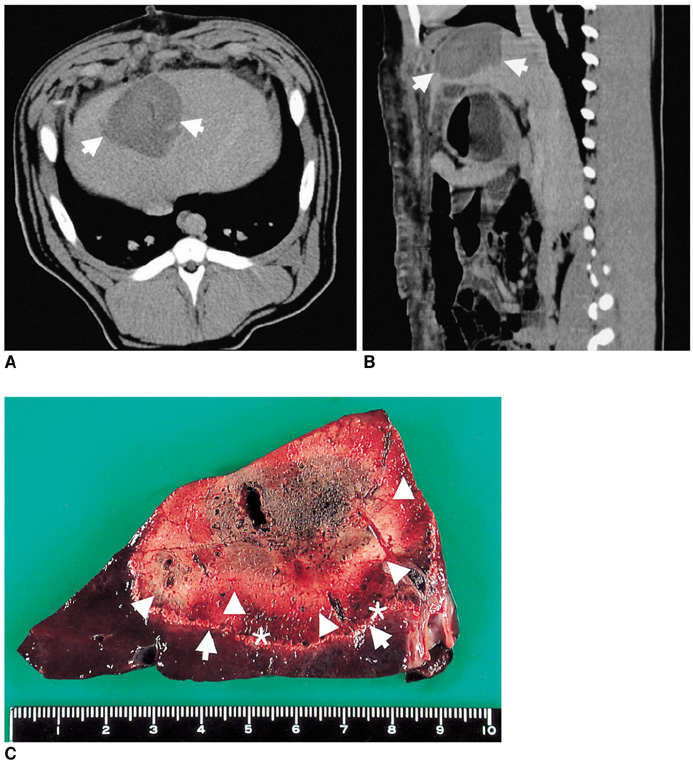
We wanted to compare the efficiency of multipolar radiofrequency ablation (RFA) using three perfused-cooled electrodes with multiple overlapping- and simultaneous monopolar techniques for creating an ablation zone in ex vivo bovine livers and in in vivo porcine livers. MATERIALS AND METHODS: In the ex vivo experiments, we used a 200 W generator (Valleylab, CC-3 model) and three perfused-cooled electrodes or internally cooled electrodes to create 30 coagulation zones by performing consecutive monopolar RFA (group A, n = 10), simultaneous monopolar RFA (group B, n = 10) or multipolar RFA (group C, n = 10) in explanted bovine livers. In the consecutive mode, three ablation spheres were created by sequentially applying 150 watts radiofrequency (RF) energy to the internally cooled electrodes for 12 minutes each for a total of 36 minutes. In the simultaneous monopolar and multipolar modes, RF energy was concurrently applied to the three perfused-cooled electrodes for 20 minutes at 150 watt with instillation of 6% hypertonic saline at 2 mL/min. During RFA, we measured the temperatures of the treated area at its center. The changes in impedance, the current and liver temperature during RFA, as well as the dimensions of the thermal ablation zones, were compared among the three groups. In the in vivo experiments, three coagulations were created by performing multipolar RFA in a pig via laparotomy with using same parameter as the ex vivo study. RESULTS: In the ex vivo experiments, the impedance was gradually decreased during the RFA in groups B and C, but in group A, the impedance was increased during RFA and this induced activation by the pulsed RF technique. In groups A, B and C, the mean final-temperature values were 80 +/- 10 degrees C, 69+/-18 degrees C and 79 +/- 12 degrees C, respectively (p < 0.05). The multipolar mode created a larger volume of ablation than did the other modes: 37.6 +/-4.0 cm3 (group A); 44.9 +/- 12.7 cm3 (group B); and 78.9 +/- 6.9 cm3 (group C) (p < 0.05). In the in vivo experiment, the pig well tolerated the RFA procedure and no major complications occurred during the 4 days of the follow-up period. The mean volume of coagulations produced by multipolar RFA in the pig liver was 60.5+/-17.9 cm3. CONCLUSION: For the multiple probe RFA, the multipolar mode with hypertonic saline instillation was more efficient in generating larger areas of thermal ablation than either the consecutive or simultaneous monopolar modes.
MeSH Terms
Figure
Cited by 2 articles
-
Percutaneous Radiofrequency Ablation with Multiple Electrodes for Medium-Sized Hepatocellular Carcinomas
Jung Lee, Jeong Min Lee, Jung-Hwan Yoon, Jae Young Lee, Se Hyung Kim, Jeong Eun Lee, Joon Koo Han, Byung Ihn Choi
Korean J Radiol. 2012;13(1):34-43. doi: 10.3348/kjr.2012.13.1.34.Evaluation of the
In Vivo Efficiency and Safety of Hepatic Radiofrequency Ablation Using a 15-G Octopus® in Pig Liver
Eun Sun Lee, Jeong Min Lee, Kyung Won Kim, In Joon Lee, Joon Koo Han, Byung Ihn Choi
Korean J Radiol. 2013;14(2):194-201. doi: 10.3348/kjr.2013.14.2.194.
Reference
-
1. Cance WG, Stewart AK, Menck HR. The National Cancer Data Base Report on treatment patterns for hepatocellular carcinomas: improved survival of surgically resected patients, 1985-1996. Cancer. 2000. 88:912–920.2. Weber SM, Jarnagin WR, De Matteo RP, Blumgart LH, Fong Y. Survival after resection of multiple hepatic colorectal metastases. Ann Surg Oncol. 2000. 7:643–650.3. Vogl TJ, Muller PK, Mack MG, Straub R, Engelmann K, Neuhaus P. Liver metastases: interventional therapeutic techniques and results, stage of the art. Eur Radiol. 1999. 9:675–684.4. Marcos-Alvarez A, Jenkins RL, Washburn WK, Lewis WD, Stuart KE, Gordon FD, et al. Multimodality treatment of hepatocellular carcinoma in a hepatobiliary specialty center. Arch Surg. 1996. 131:292–298.5. McGhana JP, Dodd GD 3rd. Radiofrequency ablation of the liver: current status. AJR Am J Roentgenol. 2001. 176:3–16.6. Solbiati L, Livraghi T, Goldberg SN, Ierace T, Meloni F, Dellanoce M, et al. Percutaneous radiofrequency ablation of hepatic metastases from colorectal cancer: long-term results in 117 patients. Radiology. 2001. 221:159–166.7. Goldberg SN, Solbiati L, Hahn PF, Cosman E, Conrad JE, Fogle R, et al. Large-volume tissue ablation with radio frequency by using a clustered, internally cooled electrode technique: laboratory and clinical experience in liver metastases. Radiology. 1998. 209:371–379.8. Curley SA, Izzo F, Ellis LM, Vauthey JN, Vallone P. Radiofrequency ablation of hepatocellular cancer in 110 patients with cirrhosis. Ann Surg. 2000. 232:381–391.9. Rossi S, Di Stasi M, Buscarini E, Quaretti P, Garbagnati F, Squassante L, et al. Percutaneous RF interstitial thermal ablation in the treatment of hepatic cancer. AJR Am J Roentgenol. 1996. 167:759–768.10. Giorgio A, Tarantino L, de Stefano G, Scala V, Liorre G, Scarano F, et al. Percutaneous sonographically guided saline-enhanced radiofrequency ablation of hepatocellular carcinoma. AJR Am J Roentgenol. 2003. 181:479–484.11. Dupuy DE, Goldberg SN. Image-guided radiofrequency tumor ablation: challenges and opportunities - part II. J Vasc Interv Radiol. 2001. 12:1135–1148.12. de Baere T, Elias D, Dromain C, Din MG, Kuoch V, Ducreux M, et al. Radiofrequency ablation of 100 hepatic metastases with a mean follow-up of more than 1 year. AJR Am J Roentgenol. 2000. 175:1619–1625.13. Livraghi T, Goldberg SN, Lazzaroni S, Meloni F, Ierace T, Solbiati L, et al. Hepatocellular carcinoma: radio-frequency ablation of medium and large lesions. Radiology. 2000. 214:761–768.14. Dodd GD 3rd, Frank MS, Aribandi M, Chopra S, Chintapalli KN. Radiofrequency thermal ablation: computer analysis of the size of the thermal injury created by overlapping ablations. AJR Am J Roentgenol. 2002. 177:777–782.15. Goldberg SN. Radiofrequency tumor ablation: principles and techniques. Eur J Ultrasound. 2001. 13:129–147.16. Mulier S, Miao Y, Mulier P, Dupas B, Pereira P, de Baere T, et al. Electrodes and multiple electrode systems for radiofrequency ablation: a proposal for updated terminology. Eur Radiol. 2005. 15:798–808.17. Goldberg SN, Gazelle GS, Dawson SL, Rittman WJ, Mueller PR, Rosenthal DI. Tissue ablation with radiofrequency using multiple probe arrays. Acad Radiol. 1995. 2:670–674.18. Jang IS, Rhim H, Koh BH, Cho OK, Seo HS, Kim Y, et al. An experimental study of simultaneous ablation with dual probes in radiofrequency thermal ablation. J Korean Radiol Soc. 2003. 48:163–169.19. Lee FT Jr, Haemmerich D, Wright AS, Mahvi DM, Sampson LA, Webster JG. Multiple probe radiofrequency ablation: pilot study in an animal model. J Vasc Interv Radiol. 2003. 14:1437–1442.20. Haemmerich D, Lee FT Jr, Schutt DJ, Sampson LA, Webster JG, Fine JP, et al. Large-volume radiofrequency ablation of ex vivo bovine liver with multiple cooled cluster electrodes. Radiology. 2005. 234:563–568.21. Lee JM, Rhim H, Han JK, Youn BJ, Kim SH, Choi BI. Dual-probe radiofrequency ablation: an in vitro experimental study in bovine liver. Invest Radiol. 2004. 39:89–96.22. Lee JM, Han JK, Choi SH, Kim SH, Lee JY, Shin KS, et al. Comparison of renal ablation with monopolar radiofrequency and hypertonic-saline-augmented bipolar radiofrequency: in vitro and in vivo experimental studies. AJR Am J Roentgenol. 2005. 184:897–905.23. McGahan JP, Gu WZ, Brock JM, Tesluk H, Jones CD. Hepatic ablation using bipolar radiofrequency electrocautery. Acad Radiol. 1996. 3:418–422.24. Burdio F, Guemes A, Burdio JM, Navarro A, Sousa R, Castiella T, et al. Bipolar saline-enhanced electrode for radiofrequency ablation: results of experimental study of in vivo porcine liver. Radiology. 2003. 229:447–456.25. Lee JM, Han JK, Kim SH, Han CJ, An SK, Lee JY, et al. Wetradio-frequency ablation using multiple electrodes: comparative study of bipolar versus monopolar modes in the bovine liver. Eur J Radiol. 2005. 54:408–417.26. Lee JM, Han JK, Kim SH, Sohn KL, Choi SH, Choi BI. Bipolar radiofrequency ablation in ex vivo bovine liver with the open-perfused system versus the cooled-wet system. Eur Radiol. 2005. 15:759–764.27. Haemmerich D, Tungjitkusolmun S, Staelin ST, Lee FT Jr, Mahvi DM, Webster JG. Finite-element analysis of hepatic multiple probe radio-frequency ablation. IEEE Trans Biomed Eng. 2002. 49:836–842.28. Nakada SY, Jerde TJ, Warner TF, Wright AS, Haemmerich D, Mahvi DM. Bipolar radiofrequency ablation of the kidney: comparison with monopolar radiofrequency ablation. J Endourol. 2003. 17:927–933.29. Haemmerich D, Lee FT Jr. Multiple applicator approaches for radiofrequency and microwave ablation. Int J Hyperthermia. 2005. 21:93–106.30. Ritz JP, Lehmann KS, Reissfelder C, Albrecht T, Frericks B, Zurbuchen U, et al. Bipolar radiofrequency ablation of liver metastases during laparotomy: First clinical experiences with a new multipolar ablation concept. Int J Colorectal Dis. 2005. May. [Epub ahead of print].31. Tacke J, Mahnken A, Roggan A, Gunther RW. Multipolar radiofrequency ablation: first clinical results. Rofo. 2004. 176:324–329.32. Lee JD, Lee JM, Kim SW, Kim CS, Mun WS. MR imaging-histopathologic correlation of radiofrequency thermal ablation lesion in a rabbit liver model: observation during acute and chronic stages. Korean J Radiol. 2001. 2:151–158.33. Morimoto M, Sugimori K, Shirato K, Kokawa A, Tomita N, Saito T, et al. Treatment of hepatocellular carcinoma with radiofrequency ablation: radiologic-histologic correlation during follow-up periods. Hepatology. 2002. 35:1467–1475.34. 2004. accessed November 20th. http://rsb.info.nih.gov/ij/ .35. Goldlust EJ, Placzynski RP, He YY, Hsu CY, Coldberg MP. Automated measurement of infarct size with scanned images of triphenyltetrazolium chloride-stained rat brains. Stroke. 1996. 27:1657–1662.36. Mulier S, Miao Y, Mulier P, Dupas B, Pereira P, de Baere T, et al. Electrodes and multiple electrode systems for radiofrequency ablation: a proposal for updated terminology. Eur Radiol. 2005. 15:798–808.37. Goldberg SN, Grassi CJ, Cardella JF, Charboneau JW, Dodd GD 3rd, Dupuy DE, et al. Image-guided tumor ablation: standardization of terminology and reporting criteria. Radiology. 2005. 235:728–739.38. Lee JM, Kim YK, Lee YH, Kim SW, Li CA, Kim CS. Percutaneous radiofrequency thermal ablation with hypertonic saline injection: invivo study in a rabbit liver model. Korean J Radiol. 2003. 4:27–34.39. Goldberg SN, Ahmed M, Gazelle GS, Kruskal JB, Huertas JC, Halpern EF, et al. Radio-frequency thermal ablation with NaCl solution injection: effect of electrical conductivity on tissue heating and coagulation-phantom and porcine liver study. Radiology. 2001. 219:157–165.40. Patterson EJ, Scudamore CH, Owen DA, Nagy AG, Buczkowski AK. Radiofrequency ablation of porcine liver in vivo: effects of blood flow and treatment time on lesion size. Ann Surg. 1998. 227:559–565.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Ablative Outcomes of Various Energy Modes for No-Touch and Peripheral Tumor-Puncturing Radiofrequency Ablation: An Ex Vivo Simulation Study
- Monopolar Radiofrequency Ablation Using a Dual-Switching System and a Separable Clustered Electrode: Evaluation of the In Vivo Efficiency
- A Comparative Experimental Study of the, In-vitro Efficiency of Hypertonic, Saline-Enhanced Hepatic Bipolar and, Monopolar Radiofrequency Ablation
- Radiofrequency Ablation of Hepatic Cysts: Case Report
- No-Touch Radiofrequency Ablation: A Comparison of Switching Bipolar and Switching Monopolar Ablation in Ex Vivo Bovine Liver