Korean J Radiol.
2004 Jun;5(2):121-127. 10.3348/kjr.2004.5.2.121.
Saline-Enhanced Hepatic Radiofrequency Ablation Using a Perfused-Cooled Electrode: Comparison of Dual Probe Bipolar Mode with Monopolar and Single Probe Bipolar Modes
- Affiliations
-
- 1Department of Radiology, and Institute of Radiation Medicine, Seoul National University College of Medicine. hanjk@radcom.snu.ac.kr
- 2Clinical Research Institute, Seoul National University Hospital.
- KMID: 753992
- DOI: http://doi.org/10.3348/kjr.2004.5.2.121
Abstract
OBJECTIVE
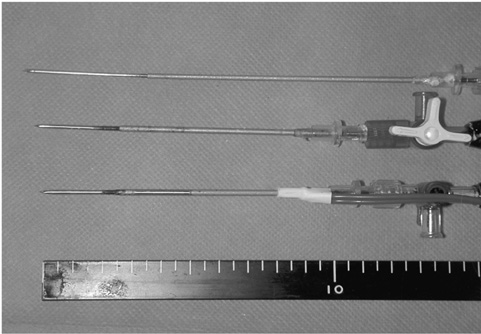
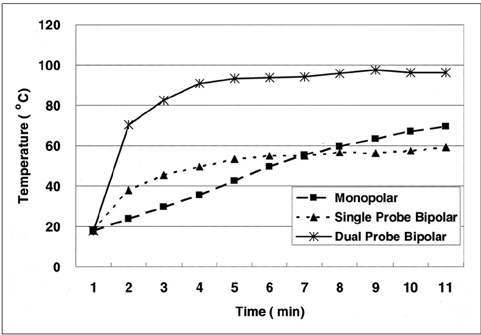
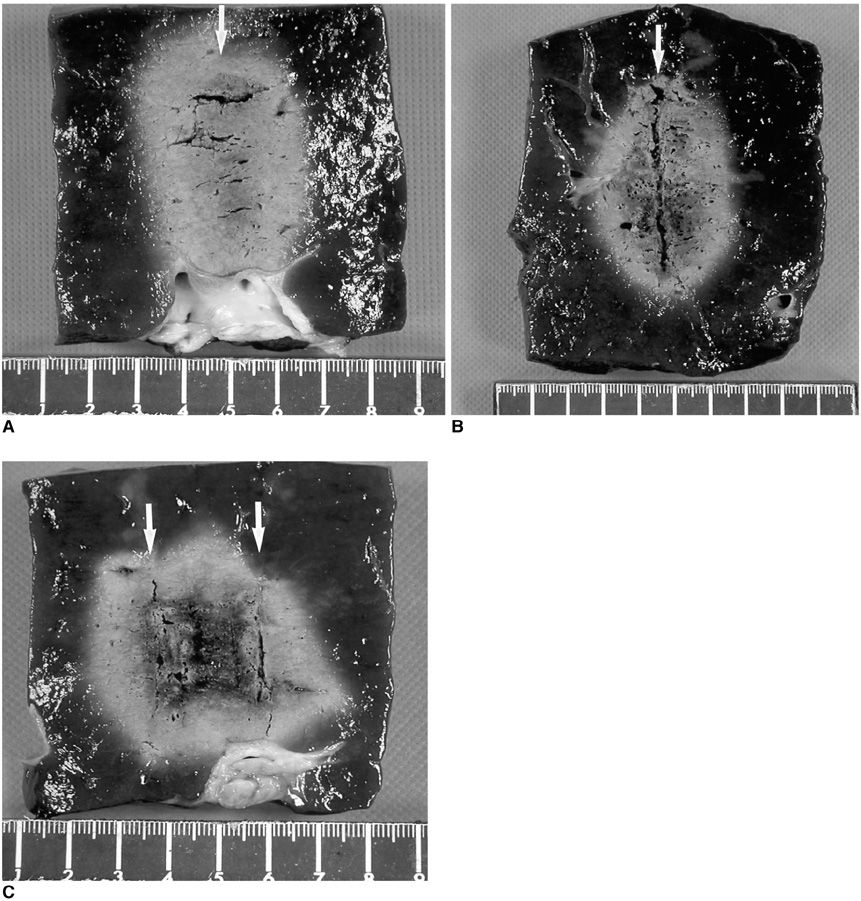
To determine whether saline-enhanced dual probe bipolar radiofrequency ablation (RFA) using perfused-cooled electrodes shows better in-vitro efficiency than monopolar or single probe bipolar RFA in creating larger coagulation necrosis. MATERIALS AND METHODS: RF was applied to excised bovine livers in both bipolar and monopolar modes using a 200W generator (CC-3; Radionics) and the perfused-cooled electrodes for 10 mins. After placing single or double perfused-cooled electrodes in the explanted liver, 30 ablation zones were created at three different regimens: group A; saline-enhanced monopolar RFA, group B; saline-enhanced single probe bipolar RFA, and group C; saline-enhanced dual probe bipolar RFA. During RFA, we measured the tissue temperature at 15 mm from the electrode. The dimensions of the ablation zones and changes in the impedance currents and liver temperature during RFA were then compared between the groups. RESULTS: The mean current values were higher for monopolar mode (group A) than for the bipolar modes (groups B and C) : 1550+/-25 mA in group A, 764+/-189 mA in group B and 819+/-98 mA in group C (p < 0.05). The volume of RF-induced coagulation necrosis was greater in group C than in the other groups: 27.6+/-2.9 cm3 in group A, 23.7+/-3.8 cm3 in group B, and 34.2+/-5.1 cm3 in group C (p < 0.05). However, there was no significant difference between the short-axis diameter of the coagulation necrosis in the three groups: 3.1+/-0.8 cm, 2.9+/-1.2 cm and 4.0+/-1.3 cm in groups A, B and C, respectively (p > 0.05). The temperature at 15 mm from the electrode was higher in group C than in the other groups: 70+/-18 degrees C in group A, 59+/-23 degrees C in group B and 96+/-16 degrees C in group C (p < 0.05). CONCLUSION: Saline-enhanced bipolar RFA using dual perfused-cooled electrodes increases the dimension of the ablation zone more efficiently than monopolar RFA or single probe bipolar RFA.
MeSH Terms
Figure
Cited by 1 articles
-
Recent Advances in the Image-Guided Tumor Ablation of Liver Malignancies: Radiofrequency Ablation with Multiple Electrodes, Real-Time Multimodality Fusion Imaging, and New Energy Sources
Dong Ho Lee, Jeong Min Lee
Korean J Radiol. 2018;19(4):545-559. doi: 10.3348/kjr.2018.19.4.545.
Reference
-
1. Goldberg SN. Radiofrequency tumor ablation: principles and techniques. Eur J Ultrasound. 2001. 13:129–147.2. Dodd GD, Frank MS, Aribandi M, Chopra S, Chintapalli KN. Radiofrequency thermal ablation: computer analysis created by overlapping ablations. AJR Am J Roentgenol. 2002. 177:777–782.3. Lee JM, Kim YK, Lee YH, Kim SW, Li CA, Kim CS. Percutaneous radiofrequency thermal ablation with hypertonic saline injection: in-vivo study in a rabbit liver model. Korean J Radiol. 2003. 4:27–34.4. Munver R, Threatt CB, Delvecchio FC, Preminger GM, Polascik TJ. Hypertonic saline-augmented radiofrequency ablation of VX2 tumor implanted in rabbit kidney: a short-term survival pilot study. Urology. 2002. 60:170–175.5. Goldberg SN, Solbiati L, Hahn PF, Cosman E, Conrad JE, Fogle R, et al. Large-volume tissue ablation with radio frequency by using a clustered, internally cooled electrode technique: laboratory and clinical experience in liver metastases. Radiology. 1998. 209:371–379.6. Lee JM, Rhim H, Han JK, Youn BJ, Kim SH, Choi BI. Dual-probe radiofrequency ablation: an in vitro experimental study in bovine liver. Invest Radiol. 2004. 39:89–96.7. Burdio F, Guemes A, Burdio JM, et al. Bipolar saline-enhanced electrode for radiofrequency ablation: results of experimental study of in vivo porcine liver. Radiology. 2003. 229:447–456.8. McGahan JP, Gu WZ, Brock JM, Tesluk H, Jones CD. Hepatic ablation using bipolar radiofrequency electrocautery. Acad Radiol. 1996. 3:418–422.9. Curley SA, Davidson BS, Fleming RY, et al. Laparoscopically guided bipolar radiofrequency ablation of areas of porcine liver. Surg Endosc. 1997. 11:729–733.10. Haemmerich D, Staelin ST, Tungjitkusolmun S, Lee FT, Mahvi DM, Webster JG. Hepatic bipolar radiofrequency ablation between separated multiprong electrodes. IEEE Trans BioMed Eng. 2001. 48:1145–1152.11. Lee JM, Han JK, Kim SH, et al. A comparative experimental study of the in-vitro efficiency of hypertonic saline-enhanced hepatic bipolar and monopolar radiofrequency ablation. Korean J Radiol. 2003. 4:163–169.12. Burdio F, Guemes A, Burdio JM, et al. Hepatic lesion ablation with bipolar saline-enhanced radiofrequency in the audible spectrum. Acad Radiol. 1999. 6:680–686.13. Ni Y, Miao Y, Mulier S, Yu J, Baert AL, Marchal G. A novel "cooled-wet" electrode for radiofrequency ablation. Eur Radiol. 2000. 10:852–854.14. Miao Y, Ni Y, Yu J, Marchal G. A comparative study on validation of a novel cooled-wet electrode for radiofrequency liver ablation. Invest Radiol. 2000. 35:438–444.15. Lee JM, Han JK, Kim SH, et al. Wet radio-frequency ablation using dual electrodes: comparative study of bipolar mode versus monopolar simultaneous and alternating modes in the bovine liver. EJR. 2004. (in press).16. Goldberg SN, Stein MC, Gazelle GS, Sheiman RG, Kruskal JB, Clouse ME. Percutaneous radiofrequency tissue ablation: optimization of pulsed-radiofrequency technique to increase coagulation necrosis. J Vasc Interv Radiol. 1999. 10:907–916.17. Lee JD, Lee JM, Kim SW, Kim CS, Mun WS. MR imaging-histopathologic correlation of radiofrequency thermal ablation lesion in a rabbit liver model: observation during acute and chronic stages. Korean J Radiol. 2001. 2:151–158.18. Kettenbach J, Kostler W, Rucklinger E, et al. Percutaneous saline-enhanced radiofrequency ablation of unresectable hepatic tumors: initial experience in 26 patients. AJR Am J Roentgenol. 2003. 180:1537–1545.19. Miao Y, Ni Y, Yu J, Zhang H, Baert A, Marchal G. An ex vivo study on radiofrequency tissue ablation: increased lesion size by using an "expandable-wet" electrode. Eur Radiol. 2001. 11:1841–1847.20. Goldberg SN, Gazelle GS, Mueller PR. Thermal ablation therapy for focal malignancy: a unified approach to underlying principles, techniques and diagnostic imaging guidance. AJR Am J Roentgenol. 2000. 174:323–331.21. Goldberg SN, Ahmed M, Gazelle GS, et al. Radiofrequency thermal ablation with NaCl solution injection: effect of electrical conductivity on tissue heating, and coagulation-phantom and porcine liver study. Radiology. 2001. 219:157–165.22. Haemmerich D, Tungjitkusolmun S, Staelin ST, Lee FT Jr, Mahvi DM, Webster JG. Finite-element analysis of hepatic multiple probe radio-frequency ablation. IEEE Trans Biomed Eng. 2002. 49:836–842.23. Jang IS, Rhim H, Koh BH, et al. An experimental study of simultaneous ablation with dual probes in radiofrequency thermal ablation. J Korean Radiol Soc. 2003. 48:163–169. (in Korean).24. Goldberg SN, Hahn PF, Halpern EF, Fogle RM, Gazelle GS. Radiofrequency tissue ablation: effect of pharmacologic modulation of blood flow on coagulation diameter. Radiology. 1998. 209:761–769.25. Patterson EJ, Scudamore CH, Owen DA, Nagy AG, Buczkowski AK. Radiofrequency ablation of porcine liver in vivo: effects of blood flow and treatment time on lesion size. Ann Surg. 1998. 227:559–565.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparative Experimental Study of the, In-vitro Efficiency of Hypertonic, Saline-Enhanced Hepatic Bipolar and, Monopolar Radiofrequency Ablation
- Radio Frequency Ablation in the Rabbit Lung Using Wet Electrodes: Comparison of Monopolar and Dual Bipolar Electrode Mode
- Hepatic Radiofrequency Ablation Using Multiple Probes: Ex Vivo and In Vivo Comparative Studies of Monopolar versus Multipolar Modes
- Ablative Outcomes of Various Energy Modes for No-Touch and Peripheral Tumor-Puncturing Radiofrequency Ablation: An Ex Vivo Simulation Study
- Dual Switching Monopolar Radiofrequency Ablation Using a Separable Clustered Electrode: Comparison with Consecutive and Switching Monopolar Modes in Ex Vivo Bovine Livers