Int J Thyroidol.
2023 Nov;16(2):209-213. 10.11106/ijt.2023.16.2.209.
Primary Thyroid Lymphoma with Vocal Fold Paralysis
- Affiliations
-
- 1Department of Otolaryngology-Head and Neck Surgery, College of Medicine, Hanyang University, Seoul, Korea
- KMID: 2548751
- DOI: http://doi.org/10.11106/ijt.2023.16.2.209
Abstract
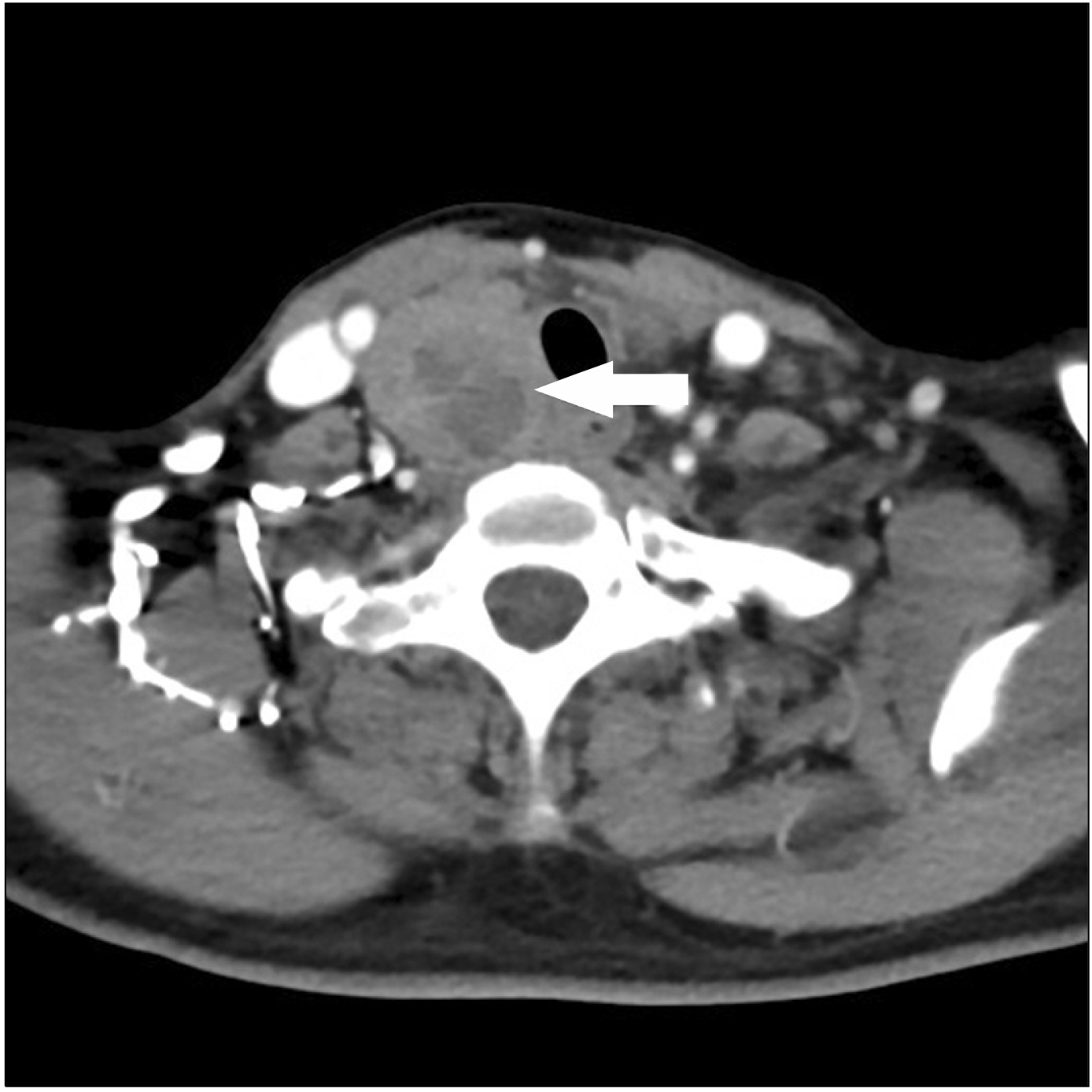
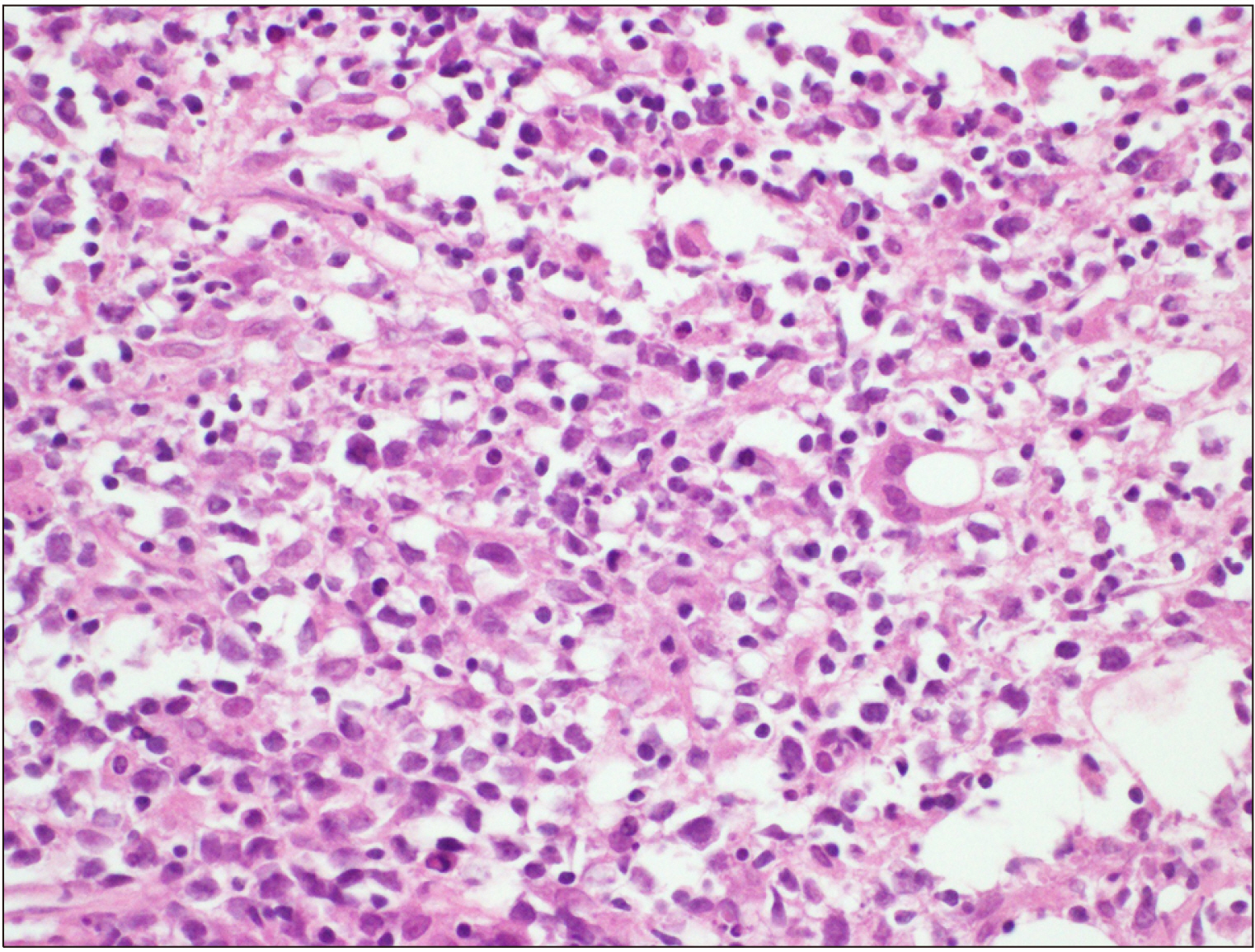
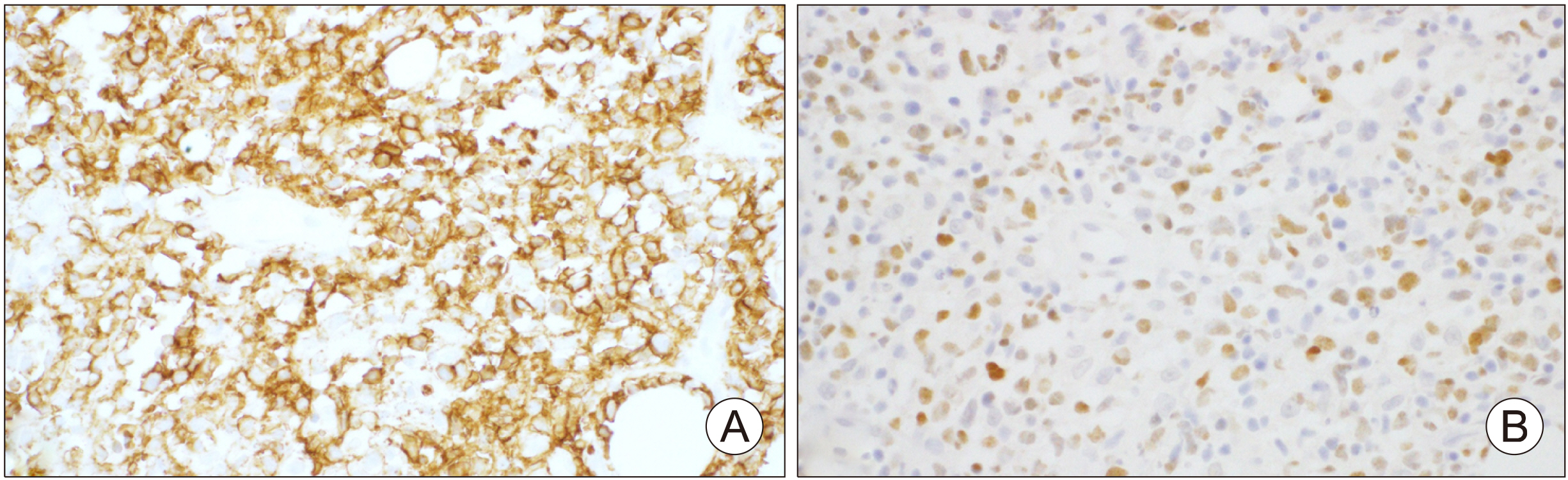
- Primary thyroid lymphoma is defined as a lymphoma involving either the thyroid gland alone or both the thyroid gland and neck lymph nodes, without contiguous spread or distant metastases from other areas of involvement at the time of diagnosis. Despite its rarity, prompt recognition of primary thyroid lymphoma is essential due to its distinct management, which differs significantly from the treatment approaches for other neoplasms of the thyroid gland. Herein, we report a 64 years old female patient who complained of hoarseness, and was diagnosed as thyroid lymphoma with unilateral vocal fold paralysis. After chemotherapy, vocal fold paralysis was relieved and the patient’s hoarseness improved.
Figure
Reference
-
References
1. Walsh S, Lowery AJ, Evoy D, McDermott EW, Prichard RS. 2013; Thyroid lymphoma: recent advances in diagnosis and optimal management strategies. Oncologist. 18(9):994–1003. DOI: 10.1634/theoncologist.2013-0036. PMID: 23881987. PMCID: PMC3780647.
Article2. Graff-Baker A, Sosa JA, Roman SA. 2010; Primary thyroid lymphoma: a review of recent developments in diagnosis and histology-driven treatment. Curr Opin Oncol. 22(1):17–22. DOI: 10.1097/CCO.0b013e3283330848. PMID: 19844180.
Article3. Li WH, Zheng WH, Zhao JQ, Wang KJ, Han C. 2022; A large-scale study of patients with preoperative vocal cord paralysis associated with thyroid disease and related clinicopathological features. Ear Nose Throat J. 1455613221115137. DOI: 10.1177/01455613221115137. PMID: 35856809.
Article4. Rowe-Jones JM, Rosswick RP, Leighton SE. 1993; Benign thyroid disease and vocal cord palsy. Ann R Coll Surg Engl. 75(4):241–4. PMID: 8379624. PMCID: PMC2497920.5. Pedersen RK, Pedersen NT. 1996; Primary non-Hodgkin's lymphoma of the thyroid gland: a population based study. Histopathology. 28(1):25–32. DOI: 10.1046/j.1365-2559.1996.268311.x. PMID: 8838117.
Article6. Pasieka JL. 2000; Hashimoto's disease and thyroid lymphoma: role of the surgeon. World J Surg. 24(8):966–70. DOI: 10.1007/s002680010159. PMID: 10865042.
Article7. Holm LE, Blomgren H, Lowhagen T. 1985; Cancer risks in patients with chronic lymphocytic thyroiditis. N Engl J Med. 312(10):601–4. DOI: 10.1056/NEJM198503073121001. PMID: 3838363.
Article8. Harrington KJ, Michalaki VJ, Vini L, Nutting CM, Syrigos KN, A'Hern R, et al. 2005; Management of non-Hodgkin's lymphoma of the thyroid: the Royal Marsden Hospital experience. Br J Radiol. 78(929):405–10. DOI: 10.1259/bjr/31803121. PMID: 15845932.
Article9. Derringer GA, Thompson LD, Frommelt RA, Bijwaard KE, Heffess CS, Abbondanzo SL. 2000; Malignant lymphoma of the thyroid gland: a clinicopathologic study of 108 cases. Am J Surg Pathol. 24(5):623–39. DOI: 10.1097/00000478-200005000-00001. PMID: 10800981.10. Demharter J, Muller P, Wagner T, Schlimok G, Haude K, Bohndorf K. 2001; Percutaneous core-needle biopsy of enlarged lymph nodes in the diagnosis and subclassification of malignant lymphomas. Eur Radiol. 11(2):276–83. DOI: 10.1007/s003300000540. PMID: 11218028.
Article11. Pavlidis ET, Pavlidis TE. 2019; A review of primary thyroid lymphoma: molecular factors, diagnosis and management. J Invest Surg. 32(2):137–42. DOI: 10.1080/08941939.2017.1383536. PMID: 29058491.
Article12. Rovira A, Carroll P, Simo R. 2023; Thyroid lymphoma. Curr Opin Otolaryngol Head Neck Surg. 31(2):83–8. DOI: 10.1097/MOO.0000000000000875. PMID: 36912220.
Article13. Chai YJ, Hong JH, Koo do H, Yu HW, Lee JH, Kwon H, et al. 2015; Clinicopathological characteristics and treatment outcomes of 38 cases of primary thyroid lymphoma: a multicenter study. Ann Surg Treat Res. 89(6):295–9. DOI: 10.4174/astr.2015.89.6.295. PMID: 26665123. PMCID: PMC4672092.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Vocal Fold Injection: Review of Indications, Techniques, and Materials for Augmentation
- A Case of Unilateral Vocal Fold Paralysis Caused by Ortner's Syndrome
- The Vertical Level of the Paralyzed Vocal Fold in Unilateral Vocal Fold Paralysis
- A Case of Head and Neck Mucosa-Associated Lymphoid Tissue Lymphoma Presenting as Progressive Multiple Cranial Nerve Palsy
- Efficiency of Intraoperative Recurrent Laryngeal Nerve Monitoring Using Electromyography Tube in Reoperative Thyroid Surgery