Brain Tumor Res Treat.
2023 Oct;11(4):254-265. 10.14791/btrt.2023.0033.
Survival and Malignant Transformation of Pineal Parenchymal Tumors: A 30-Year Retrospective Analysis in a Single-Institution
- Affiliations
-
- 1Department of Neurosurgery, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 2Division of Pediatric Neurosurgery, Seoul National University Children’s Hospital, Seoul, Korea
- 3Neuroscience Research Institute, Seoul National University Medical Research Center, Seoul National University College of Medicine, Seoul, Korea
- 4Department of Pathology, Seoul National University Hospital, Seoul National University College of Medicine, Seoul, Korea
- 5Center of Hospital Medicine, Seoul National University Hospital, Seoul, Korea
- KMID: 2547414
- DOI: http://doi.org/10.14791/btrt.2023.0033
Abstract
- Background
This study aims to elucidate clinical features, therapeutic strategies, and prognosis of pineal parenchymal tumors (PPT) by analyzing a 30-year dataset of a single institution.
Methods
We reviewed data from 43 patients diagnosed with PPT at Seoul National University Hospital between 1990 and 2020. We performed survival analyses and assessed prognostic factors.
Results
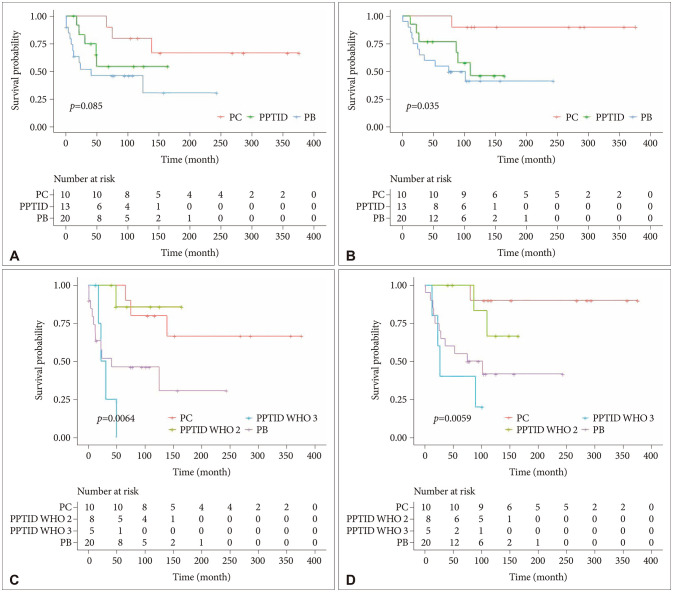
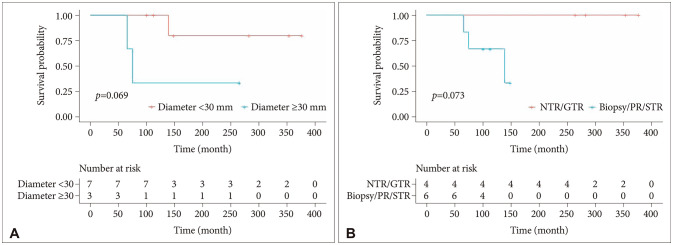
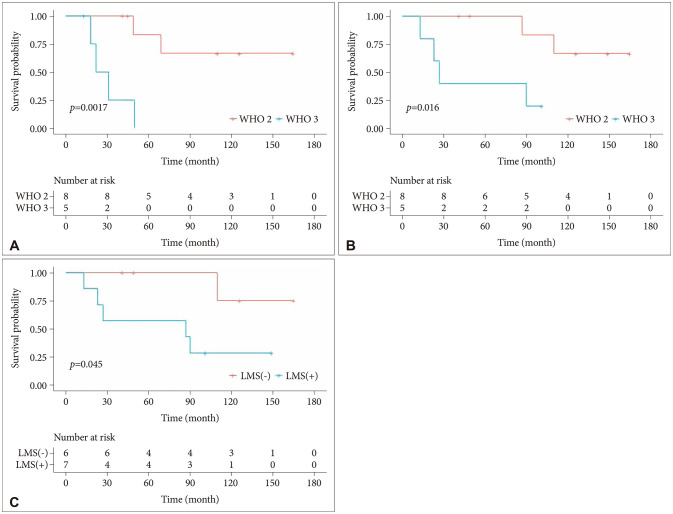
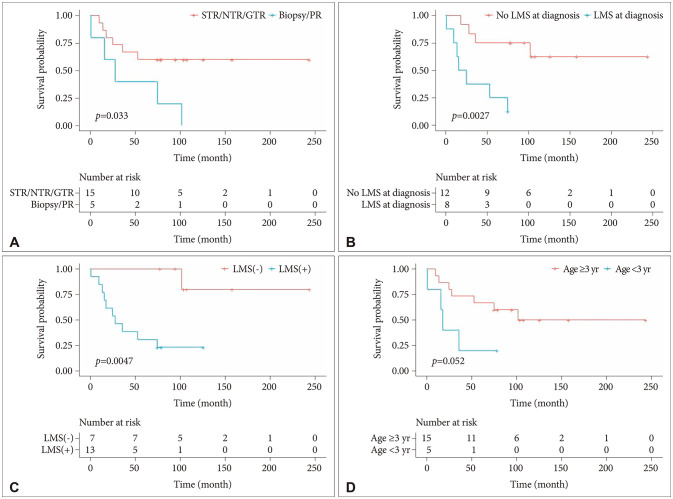
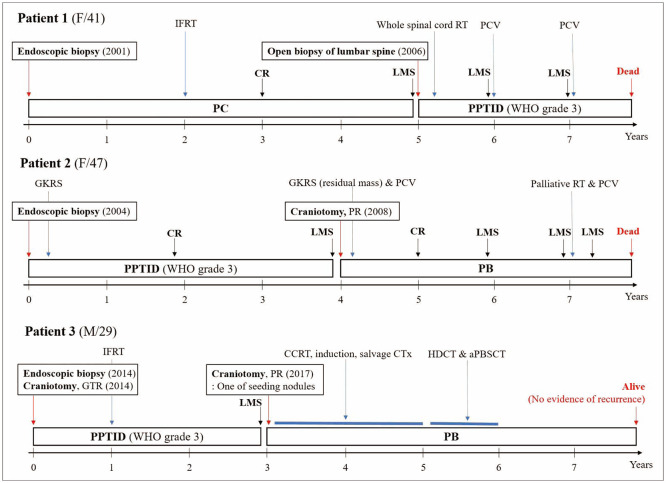
The cohort included 10 patients with pineocytoma (PC), 13 with pineal parenchymal tumor of intermediate differentiation (PPTID), and 20 with pineoblastoma (PB). Most patients presented with hydrocephalus at diagnosis. Most patients underwent an endoscopic third ventriculostomy and biopsy, with some undergoing additional resection after diagnosis confirmation. Radiotherapy was administered with a high prevalence of gamma knife radiosurgery for PC and PPTID, and craniospinal irradiation for PB. Chemotherapy was essential in the treatment of grade 3 PPTID and PB. The 5-year progression-free survival rates for PC, grade 2 PPTID, grade 3 PPTID, and PB were 100%, 83.3%, 0%, and 40%, respectively, and the 5-year overall survival rates were 100%, 100%, 40%, and 55%, respectively. High-grade tumor histology was associated with lower survival rates. Significant prognostic factors varied among tumor types, with World Health Organization (WHO) grade and leptomeningeal seeding (LMS) for PPTID, and the extent of resection and LMS for PB. Three patients experienced malignant transformations.
Conclusion
This study underscores the prognostic significance of WHO grades in PPT. It is nec-essary to provide specific treatment according to tumor grade. Grade 3 PPTID showed a poor prognosis. Potential LMS and malignant transformations necessitate aggressive multimodal treatment and close-interval screening.
Figure
Reference
-
1. Raleigh DR, Solomon DA, Lloyd SA, Lazar A, Garcia MA, Sneed PK, et al. Histopathologic review of pineal parenchymal tumors identifies novel morphologic subtypes and prognostic factors for outcome. Neuro Oncol. 2017; 19:78–88. PMID: 27282397.
Article2. Figarella-Branger D. Pineal tumours. WHO Classification of Tumours Editorial Board. WHO classification of tumours: central nervous system tumours. 5th ed. Lyon: International Agency for Research on Cancer;2021. p. 241–252.3. Jouvet A, Saint-Pierre G, Fauchon F, Privat K, Bouffet E, Ruchoux MM, et al. Pineal parenchymal tumors: a correlation of histological features with prognosis in 66 cases. Brain Pathol. 2000; 10:49–60. PMID: 10668895.
Article4. Deng X, Yang Z, Zhang X, Lin D, Xu X, Lu X, et al. Prognosis of pediatric patients with pineoblastoma: a SEER analysis 1990–2013. World Neurosurg. 2018; 118:e871–e879. PMID: 30031180.
Article5. Schild SE, Scheithauer BW, Schomberg PJ, Hook CC, Kelly PJ, Frick L, et al. Pineal parenchymal tumors. Clinical, pathologic, and therapeutic aspects. Cancer. 1993; 72:870–880. PMID: 8334641.
Article6. Kleihues P, Cavenee WK. Pathology and Genetics of Tumours of the Nervous System WHO Classification of Tumours. 3rd ed. Lyon: IARC Press;2000.7. Chatterjee D, Lath K, Singla N, Kumar N, Radotra BD. Pathologic prognostic factors of pineal parenchymal tumor of intermediate differentiation. Appl Immunohistochem Mol Morphol. 2019; 27:210–215. PMID: 28800009.
Article8. Roth J, Kozyrev DA, Richetta C, Dvir R, Constantini S. Pineal region tumors: an entity with crucial anatomical nuances. Childs Nerv Syst. 2021; 37:383–390. PMID: 32725465.
Article9. Wilson DA, Awad AW, Brachman D, Coons SW, McBride H, Youssef E, et al. Long-term radiosurgical control of subtotally resected adult pineocytomas. J Neurosurg. 2012; 117:212–217. PMID: 22702479.
Article10. Louis DN, Perry A, Wesseling P, Brat DJ, Cree IA, Figarella-Branger D, et al. The 2021 WHO classification of tumors of the central nervous system: a summary. Neuro Oncol. 2021; 23:1231–1251. PMID: 34185076.
Article11. Clark AJ, Sughrue ME, Aranda D, Parsa AT. Contemporary management of pineocytoma. Neurosurg Clin N Am. 2011; 22:403–407. PMID: 21801989.
Article12. Kim BS, Kim DK, Park SH. Pineal parenchymal tumor of intermediate differentiation showing malignant progression at relapse. Neuropathology. 2009; 29:602–608. PMID: 19170892.
Article13. Liu APY, Li BK, Pfaff E, Gudenas B, Vasiljevic A, Orr BA, et al. Clinical and molecular heterogeneity of pineal parenchymal tumors: a consensus study. Acta Neuropathol. 2021; 141:771–785. PMID: 33619588.
Article14. Lee JC, Mazor T, Lao R, Wan E, Diallo AB, Hill NS, et al. Recurrent KBTBD4 small in-frame insertions and absence of DROSHA deletion or DICER1 mutation differentiate pineal parenchymal tumor of intermediate differentiation (PPTID) from pineoblastoma. Acta Neuropathol. 2019; 137:851–854. PMID: 30877433.
Article15. Fang AS, Meyers SP. Magnetic resonance imaging of pineal region tumours. Insights Imaging. 2013; 4:369–382. PMID: 23640020.
Article16. Lombardi G, Poliani PL, Manara R, Berhouma M, Minniti G, Tabouret E, et al. Diagnosis and treatment of pineal region tumors in adults: a EURACAN overview. Cancers (Basel). 2022; 14:3646. PMID: 35954310.
Article17. Cao L, Jiang Y, Zhang X, Gu Z, Liu Z, Ding L. The prognosis of pineal parenchymal tumors: development and validation of a nomogram based on surveillance, epidemiology and end results. World Neurosurg. 2023; 173:e478–e486. PMID: 36841539.
Article18. Blakeley JO, Grossman SA. Management of pineal region tumors. Curr Treat Options Oncol. 2006; 7:505–516. PMID: 17032562.
Article19. Clark AJ, Ivan ME, Sughrue ME, Yang I, Aranda D, Han SJ, et al. Tumor control after surgery and radiotherapy for pineocytoma. J Neurosurg. 2010; 113:319–324. PMID: 20136388.
Article20. Clark AJ, Sughrue ME, Ivan ME, Aranda D, Rutkowski MJ, Kane AJ, et al. Factors influencing overall survival rates for patients with pineocytoma. J Neurooncol. 2010; 100:255–260. PMID: 20461445.
Article21. Nam JY, Gilbert A, Cachia D, Mandel J, Fuller GN, Penas-Prado M, et al. Pineal parenchymal tumor of intermediate differentiation: a single-institution experience. Neurooncol Pract. 2020; 7:613–619. PMID: 33312675.
Article22. Takase H, Tanoshima R, Singla N, Nakamura Y, Yamamoto T. Pineal parenchymal tumor of intermediate differentiation: a systematic review and contemporary management of 389 cases reported during the last two decades. Neurosurg Rev. 2022; 45:1135–1155. PMID: 34668090.
Article23. Lu VM, Luther EM, Eichberg DG, Morell AA, Shah AH, Komotar RJ, et al. Prognosticating survival of pineal parenchymal tumors of intermediate differentiation (PPTID) by grade. J Neurooncol. 2021; 155:165–172. PMID: 34606044.
Article24. Ito T, Kanno H, Sato K, Oikawa M, Ozaki Y, Nakamura H, et al. Clinicopathologic study of pineal parenchymal tumors of intermediate differentiation. World Neurosurg. 2014; 81:783–789. PMID: 23396072.
Article25. Yu T, Sun X, Wang J, Ren X, Lin N, Lin S. Twenty-seven cases of pineal parenchymal tumours of intermediate differentiation: mitotic count, Ki-67 labelling index and extent of resection predict prognosis. J Neurol Neurosurg Psychiatry. 2016; 87:386–395. PMID: 25911570.
Article26. Yamashita S, Takeshima H, Hata N, Uchida H, Shinojima N, Yokogami K, et al. Clinicopathologic analysis of pineal parenchymal tumors of intermediate differentiation: a multi-institutional cohort study by the Kyushu Neuro-Oncology Study Group. J Neurooncol. 2023; 162:425–433. PMID: 37052748.
Article27. Kumar N, Srinivasa GY, Madan R, Salunke P. Role of radiotherapy in residual pineal parenchymal tumors. Clin Neurol Neurosurg. 2018; 166:91–98. PMID: 29408780.
Article28. Mallick S, Benson R, Rath GK. Patterns of care and survival outcomes in patients with pineal parenchymal tumor of intermediate differentiation: an individual patient data analysis. Radiother Oncol. 2016; 121:204–208. PMID: 27865543.
Article29. Bando T, Ueno Y, Shinoda N, Imai Y, Ichikawa K, Kuramoto Y, et al. Therapeutic strategy for pineal parenchymal tumor of intermediate differentiation (PPTID): case report of PPTID with malignant transformation to pineocytoma with leptomeningeal dissemination 6 years after surgery. J Neurosurg. 2019; 130:2009–2015.
Article30. Yi JW, Kim HJ, Choi YJ, Seol YM, Kahng DH, Choi YY, et al. Successful treatment by chemotherapy of pineal parenchymal tumor with intermediate differentiation: a case report. Cancer Res Treat. 2013; 45:244–249. PMID: 24155685.
Article31. Pfaff E, Aichmüller C, Sill M, Stichel D, Snuderl M, Karajannis MA, et al. Molecular subgrouping of primary pineal parenchymal tumors reveals distinct subtypes correlated with clinical parameters and genetic alterations. Acta Neuropathol. 2020; 139:243–257. PMID: 31768671.
Article32. Hansford JR, Huang J, Endersby R, Dodgshun AJ, Li BK, Hwang E, et al. Pediatric pineoblastoma: a pooled outcome study of North American and Australian therapeutic data. Neurooncol Adv. 2022; 4:vdac056. PMID: 35664557.
Article33. Tate M, Sughrue ME, Rutkowski MJ, Kane AJ, Aranda D, McClinton L, et al. The long-term postsurgical prognosis of patients with pineoblastoma. Cancer. 2012; 118:173–179. PMID: 21717450.
Article34. Abdelbaki MS, Abu-Arja MH, Davidson TB, Fangusaro JR, Stanek JR, Dunkel IJ, et al. Pineoblastoma in children less than six years of age: the head start I, II, and III experience. Pediatr Blood Cancer. 2020; 67:e28252. PMID: 32187454.
Article35. Mynarek M, Pizer B, Dufour C, van Vuurden D, Garami M, Massimino M, et al. Evaluation of age-dependent treatment strategies for children and young adults with pineoblastoma: analysis of pooled European Society for Paediatric Oncology (SIOP-E) and US head start data. Neuro Oncol. 2017; 19:576–585. PMID: 28011926.
Article36. Parikh KA, Venable GT, Orr BA, Choudhri AF, Boop FA, Gajjar AJ, et al. Pineoblastoma—The experience at St. Jude Children’s Research Hospital. Neurosurgery. 2017; 81:120–128. PMID: 28327927.
Article37. Farnia B, Allen PK, Brown PD, Khatua S, Levine NB, Li J, et al. Clinical outcomes and patterns of failure in pineoblastoma: a 30-year, single-institution retrospective review. World Neurosurg. 2014; 82:1232–1241. PMID: 25045788.
Article38. Tian Y, Liu R, Qin J, Wang J, Ma Z, Gong J, et al. Retrospective analysis of the clinical characteristics, therapeutic aspects, and prognostic factors of 18 cases of childhood pineoblastoma. World Neurosurg. 2018; 116:e162–e168. PMID: 29709740.
Article39. Jin MC, Prolo LM, Wu A, Azad TD, Shi S, Rodrigues AJ, et al. Patterns of care and age-specific impact of extent of resection and adjuvant radiotherapy in pediatric pineoblastoma. Neurosurgery. 2020; 86:E426–E435. PMID: 32110805.
Article40. Park M, Han JW, Hahn SM, Lee JA, Kim JY, Shin SH, et al. Atypical teratoid/rhabdoid tumor of the central nervous system in children under the age of 3 years. Cancer Res Treat. 2021; 53:378–388. PMID: 33138347.
Article41. Gururangan S, McLaughlin C, Quinn J, Rich J, Reardon D, Halperin EC, et al. High-dose chemotherapy with autologous stem-cell rescue in children and adults with newly diagnosed pineoblastomas. J Clin Oncol. 2003; 21:2187–2191. PMID: 12775745.
Article42. Chalif EJ, Murray RD, Mozaffari K, Chillakuru YR, Shim T, Monfared A, et al. Malignant pineal parenchymal tumors in adults: a national cancer database analysis. Neurosurgery. 2022; 90:807–815. PMID: 35311743.
Article43. Morgenstern PF, Souweidane MM. Pineal region tumors: simultaneous endoscopic third ventriculostomy and tumor biopsy. World Neurosurg. 2013; 79(2 Suppl):S18.e9–S18.e13.
Article44. Yamini B, Refai D, Rubin CM, Frim DM. Initial endoscopic management of pineal region tumors and associated hydrocephalus: clinical series and literature review. J Neurosurg. 2004; 100:437–441. PMID: 15287451.
Article45. Chernov MF, Kamikawa S, Yamane F, Ishihara S, Kubo O, Hori T. Neurofiberscopic biopsy of tumors of the pineal region and posterior third ventricle: indications, technique, complications, and results. Neurosurgery. 2006; 59:267–277. PMID: 16883167.
Article46. Lieu AS, Wu CC, Chai CY, Ma YC, Su HY. Pineocytoma with malignant transformation to pineal parenchymal tumor with intermediate differentiation and leptomeningeal dissemination after subtotal tumor resection and adjuvant radiotherapy. Indian J Pathol Microbiol. 2023; 66:141–144. PMID: 36656225.
Article47. Gomez C, Wu J, Pope W, Vinters H, Desalles A, Selch M. Pineocytoma with diffuse dissemination to the leptomeninges. Rare Tumors. 2011; 3:e53. PMID: 22355508.
Article48. Kerezoudis P, Yolcu YU, Laack NN, Ruff MW, Khatua S, Daniels DJ, et al. Survival and associated predictors for patients with pineoblastoma or pineal parenchymal tumors of intermediate differentiation older than 3 years: insights from the national cancer database. Neurooncol Adv. 2022; 4:vdac057. PMID: 35611271.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Radiotherapy Results of pineal Tumors
- Surgical Treatment of Cavernous Malformation of Pineal Region
- A Role of Trial Radiation Therapy in the Pineal Region Tumors
- A Malignant Transformation of a Spinal Epidural Mass from Ganglioneuroblastoma to Neuroblastoma
- Pineal Region Tumors : Clinical Analysis of 13 Cases