Neurointervention.
2023 Nov;18(3):172-181. 10.5469/neuroint.2023.00269.
Low Levels of Low-Density Lipoprotein Cholesterol Increase the Risk of Post-Thrombectomy Delayed Parenchymal Hematoma
- Affiliations
-
- 1Vanderbilt University School of Medicine, Nashville, TN, USA
- 2Cerebrovascular Program, Vanderbilt University Medical Center, Nashville, TN, USA
- 3Department of Biostatistics, Vanderbilt University Medical Center, Nashville, TN, USA
- KMID: 2547279
- DOI: http://doi.org/10.5469/neuroint.2023.00269
Abstract
- Purpose
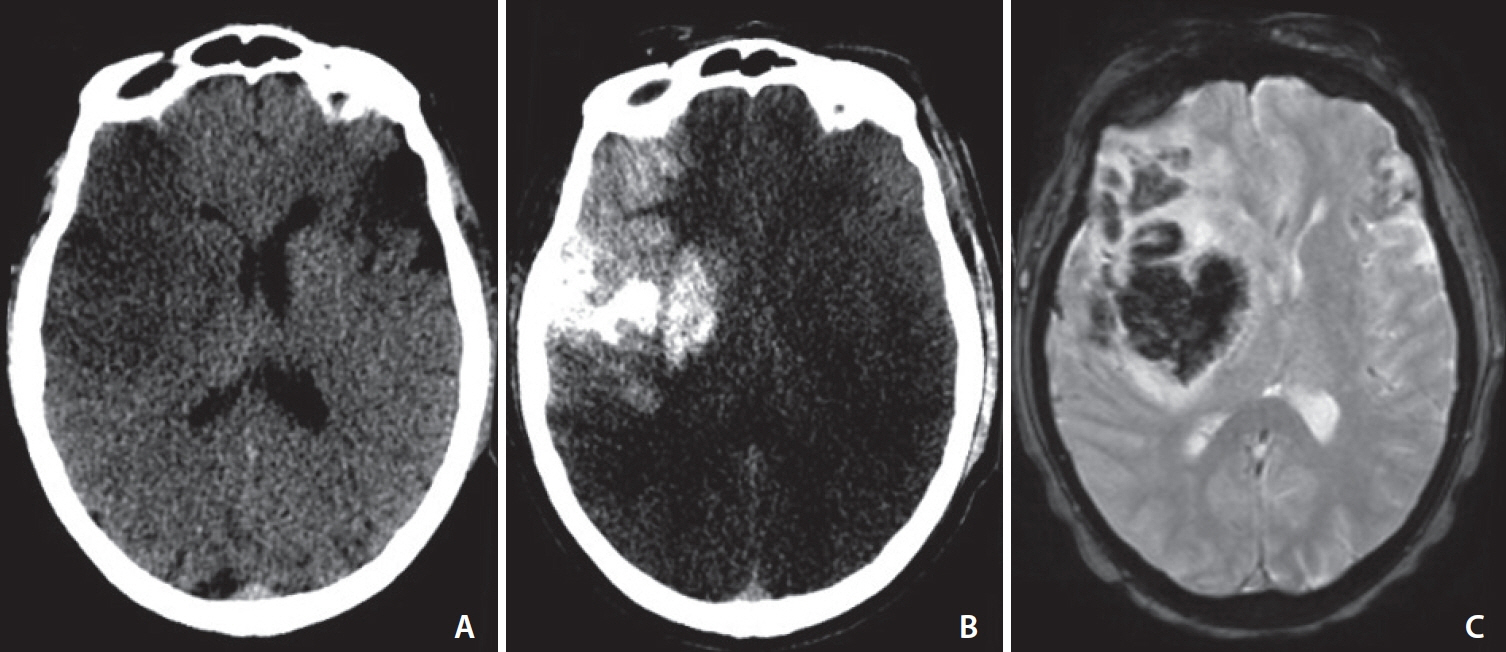
Low levels of low-density lipoprotein cholesterol (LDL-C) have been suggested to increase the risk of hemorrhagic transformation (HT) following acute ischemic stroke. However, the literature on the relationship between LDL-C levels and post-thrombectomy HT is sparse. The aim of our study is to investigate the association between LDL-C and delayed parenchymal hematoma (PH) that was not seen on immediate post-thrombectomy dual-energy computed tomography (DECT).
Materials and Methods
A retrospective analysis was conducted on all patients with anterior circulation large vessel occlusion who underwent thrombectomy at a comprehensive stroke center from 2018–2021. Per institutional protocol, all patients received DECT immediately post-thrombectomy and magnetic resonance imaging or CT at 24 hours. The presence of immediate hemorrhage was assessed by DECT, while delayed PH was assessed by 24-hour imaging. Multivariable analysis was performed to identify predictors of delayed PH. Patients with hemorrhage on immediate post-thrombectomy DECT were excluded to select only those with delayed PH.
Results
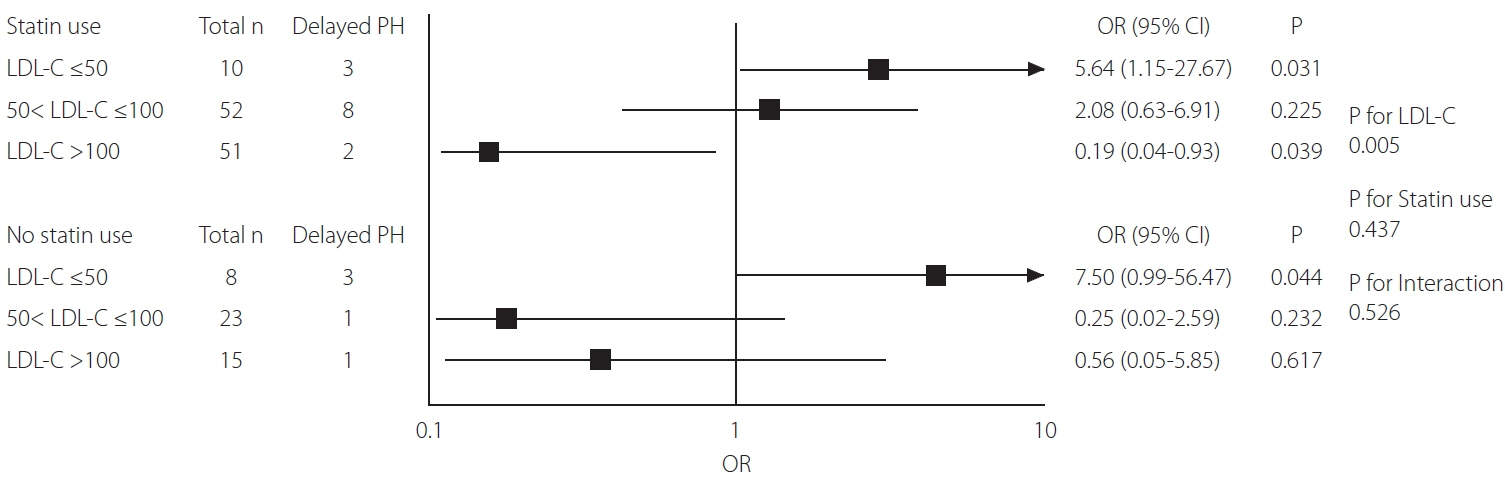
Of 159 patients without hemorrhage on immediate post-thrombectomy DECT, 18 (11%) developed delayed PH on 24-hour imaging. In multivariable analysis, LDL-C (odds ratio [OR], 0.76; P=0.038; 95% confidence interval [CI], 0.59–0.99; per 10 mg/dL increase) independently predicted delayed PH. High-density lipoprotein cholesterol, triglyceride, and statin use were not associated. After adjusting for potential confounders, LDL-C ≤50 mg/dL was associated with an increased risk of delayed PH (OR, 5.38; P=0.004; 95% CI, 1.70–17.04), while LDL-C >100 mg/dL was protective (OR, 0.26; P=0.041; 95% CI, 0.07–0.96).
Conclusion
LDL-C ≤50 mg/dL independently predicted delayed PH following thrombectomy and LDL-C >100 mg/dL was protective, irrespective of statin. Thus, patients with low LDL-C levels may warrant vigilant monitoring and necessary interventions, such as blood pressure control or anticoagulation management, following thrombectomy even in the absence of hemorrhage on immediate post-thrombectomy DECT.
Keyword
Figure
Reference
-
1. Tijssen MP, Hofman PA, Stadler AA, van Zwam W, de Graaf R, van Oostenbrugge RJ, et al. The role of dual energy CT in differentiating between brain haemorrhage and contrast medium after mechanical revascularisation in acute ischaemic stroke. Eur Radiol. 2014; 24:834–840.
Article2. DiNitto J, Feldman M, Grimaudo H, Mummareddy N, Ahn S, Bhamidipati A, et al. Flat-panel dual-energy head computed tomography in the angiography suite after thrombectomy for acute stroke: a clinical feasibility study. [published online ahead of print Feb 14, 2023]. Interv Neuroradiol. 2023.
Article3. Boisseau W, Fahed R, Lapergue B, Desilles JP, Zuber K, Khoury N, ETIS Investigators, et al. Predictors of parenchymal hematoma after mechanical thrombectomy: a multicenter study. Stroke. 2019; 50:2364–2370.
Article4. Koge J, Tanaka K, Yoshimoto T, Shiozawa M, Yamagami H, Satow T, et al. Early recurrent ischemic events after mechanical thrombectomy: effect of post-treatment intracranial hemorrhage. J Neurol. 2021; 268:2810–2820.
Article5. Larrue V, von Kummer R R, Müller A, Bluhmki E. Risk factors for severe hemorrhagic transformation in ischemic stroke patients treated with recombinant tissue plasminogen activator: a secondary analysis of the European-Australasian Acute Stroke Study (ECASS II). Stroke. 2001; 32:438–441.
Article6. Kim BJ, Lee SH, Ryu WS, Kang BS, Kim CK, Yoon BW. Low level of low-density lipoprotein cholesterol increases hemorrhagic transformation in large artery atherothrombosis but not in cardioembolism. Stroke. 2009; 40:1627–1632.
Article7. Yang N, Lin M, Wang BG, Zeng WY, He YF, Peng HY, et al. Low level of low-density lipoprotein cholesterol is related with increased hemorrhagic transformation after acute ischemic cerebral infarction. Eur Rev Med Pharmacol Sci. 2016; 20:673–678.8. Lin SF, Chao AC, Hu HH, Lin RT, Chen CH, Chan L, Taiwan Thrombolytic Therapy for Acute Ischemic Stroke (TTT-AIS) Study Group, et al. Low cholesterol levels increase symptomatic intracranial hemorrhage rates after intravenous thrombolysis: a multicenter cohort validation study. J Atheroscler Thromb. 2019; 26:513–527.
Article9. Bang OY, Saver JL, Liebeskind DS, Starkman S, Villablanca P, Salamon N, et al. Cholesterol level and symptomatic hemorrhagic transformation after ischemic stroke thrombolysis. Neurology. 2007; 68:737–742.
Article10. Uyttenboogaart M, Koch MW, Koopman K, Vroomen PC, Luijckx GJ, De Keyser J. Lipid profile, statin use, and outcome after intravenous thrombolysis for acute ischaemic stroke. J Neurol. 2008; 255:875–880.
Article11. Meier N, Nedeltchev K, Brekenfeld C, Galimanis A, Fischer U, Findling O, et al. Prior statin use, intracranial hemorrhage, and outcome after intra-arterial thrombolysis for acute ischemic stroke. Stroke. 2009; 40:1729–1737.
Article12. Rocco A, Sykora M, Ringleb P, Diedler J. Impact of statin use and lipid profile on symptomatic intracerebral haemorrhage, outcome and mortality after intravenous thrombolysis in acute stroke. Cerebrovasc Dis. 2012; 33:362–368.
Article13. Lin TC, Lin YK, Chen CI, Chan L, Chi NF, Yuan RY, et al. Serum lipid level is not associated with symptomatic intracerebral hemorrhage after intravenous thrombolysis for acute ischemic stroke. PeerJ. 2018; 6:e6021.
Article14. Higashida RT, Furlan AJ, Roberts H, Tomsick T, Connors B, Barr J, et al. Trial design and reporting standards for intra-arterial cerebral thrombolysis for acute ischemic stroke. Stroke. 2003; 34:e109–e137.
Article15. Kleine JF, Wunderlich S, Zimmer C, Kaesmacher J. Time to redefine success? TICI 3 versus TICI 2b recanalization in middle cerebral artery occlusion treated with thrombectomy. J Neurointerv Surg. 2017; 9:117–121.
Article16. Hacke W, Kaste M, Bluhmki E, Brozman M, Dávalos A, Guidetti D, ECASS Investigators, et al. Thrombolysis with alteplase 3 to 4.5 hours after acute ischemic stroke. N Engl J Med. 2008; 359:1317–1329.
Article17. Yuan T, Chen N, Jin H, Yin H. Increased microvascular permeability and low level of low-density lipoprotein cholesterol predict symptomatic intracerebral hemorrhage in acute ischemic stroke. Sci Prog. 2020; 103:36850420924153.
Article18. Pikija S, Sztriha LK, Killer-Oberpfalzer M, Weymayr F, Hecker C, Ramesmayer C, et al. Contribution of serum lipid profiles to outcome after endovascular thrombectomy for anterior circulation ischemic stroke. Mol Neurobiol. 2019; 56:4582–4588.
Article19. Ha SH, Ryu JC, Bae JH, Koo S, Kwon B, Song Y, et al. High serum total cholesterol associated with good outcome in endovascular thrombectomy for acute large artery occlusion. Neurol Sci. 2022; 43:5985–5991.
Article20. Konishi M, Iso H, Komachi Y, Iida M, Shimamoto T, Jacobs DR Jr, et al. Associations of serum total cholesterol, different types of stroke, and stenosis distribution of cerebral arteries. The Akita Pathology Study. Stroke. 1993; 24:954–964.
Article21. Zhou X, Yang Q. From hemorrhagic stroke to lipid paradox: a double-hit hypothesis underlying low low-density lipoprotein cholesterol related cardiovascular risk—a narrative review. J Bio-X Res. 2020; 3:97–103.
Article22. Nardi K, Leys D, Eusebi P, Cordonnier C, Gautier S, Hénon H, et al. Influence of lipid profiles on the risk of hemorrhagic transformation after ischemic stroke: systematic review. Cerebrovasc Dis Extra. 2011; 1:130–141.
Article23. Zhang W, Li W, Tian R, Cao L. High-density lipoprotein level is associated with hemorrhage transformation after ischemic stroke treatment with intravenous thrombolysis: a systematic review and meta-analysis. J Clin Neurosci. 2022; 106:122–127.
Article24. Amarenco P, Bogousslavsky J, Callahan A 3rd, Goldstein LB, Hennerici M, Rudolph AE, Stroke Prevention by Aggressive Reduction in Cholesterol Levels (SPARCL) Investigators, et al. High-dose atorvastatin after stroke or transient ischemic attack. N Engl J Med. 2006; 355:549–559.
Article25. Ribe AR, Vestergaard CH, Vestergaard M, Pedersen HS, Prior A, Lietzen LW, et al. Statins and risk of intracerebral hemorrhage in individuals with a history of stroke. Stroke. 2020; 51:1111–1119.
Article26. Scheitz JF, MacIsaac RL, Abdul-Rahim AH, Siegerink B, Bath PM, Endres M, VISTA Collaboration, et al. Statins and risk of poststroke hemorrhagic complications. Neurology. 2016; 86:1590–1596.
Article27. Iancu A, Buleu F, Chita DS, Tutelca A, Tudor R, Brad S. Early hemorrhagic transformation after reperfusion therapy in patients with acute ischemic stroke: analysis of risk factors and predictors. Brain Sci. 2023; 13:840.
Article28. Ahn S, Roth SG, Mummareddy N, Ko Y, Bhamidipati A, Jo J, et al. The clinical utility of dual-energy CT in post-thrombectomy care: part 2, the predictive value of contrast density and volume for delayed hemorrhagic transformation. J Stroke Cerebrovasc Dis. 2023; 32:107216.
Article29. Ahn S, Mummareddy N, Roth SG, Jo J, Bhamidipati A, Ko Y, et al. The clinical utility of dual-energy CT in post-thrombectomy care: part 1, predictors and outcomes of subarachnoid and intraparenchymal hemorrhage. J Stroke Cerebrovasc Dis. 2023; 32:107217.
Article30. Lee H, Qureshi AM, Mueller-Kronast NH, Zaidat OO, Froehler MT, Liebeskind DS, et al. Subarachnoid hemorrhage in mechanical thrombectomy for acute ischemic stroke: analysis of the STRATIS registry, systematic review, and meta-analysis. Front Neurol. 2021; 12:663058.
Article31. Kaesmacher J, Kaesmacher M, Maegerlein C, Zimmer C, Gersing AS, Wunderlich S, et al. Hemorrhagic transformations after thrombectomy: risk factors and clinical relevance. Cerebrovasc Dis. 2017; 43:294–304.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Predictors of Serum Low-Density Lipoprotein Cholesterol Level in Postmenopausal Women
- Changes in the Serum Level of High Density Lipoprotein-cholesterol after Smoking Cessation among Adult Men
- Association between Dietary Carbohydrate Intake and Cardiovascular Risk Factors According to Low-Density Lipoprotein Cholesterol Levels in Korean Adults
- Low-Carbohydrate Diets in Korea: Why Does It Matter, and What Is Next?
- Serum Lipid Levels in Psoriasis