J Cerebrovasc Endovasc Neurosurg.
2023 Sep;25(3):253-259. 10.7461/jcen.2023.E2022.10.002.
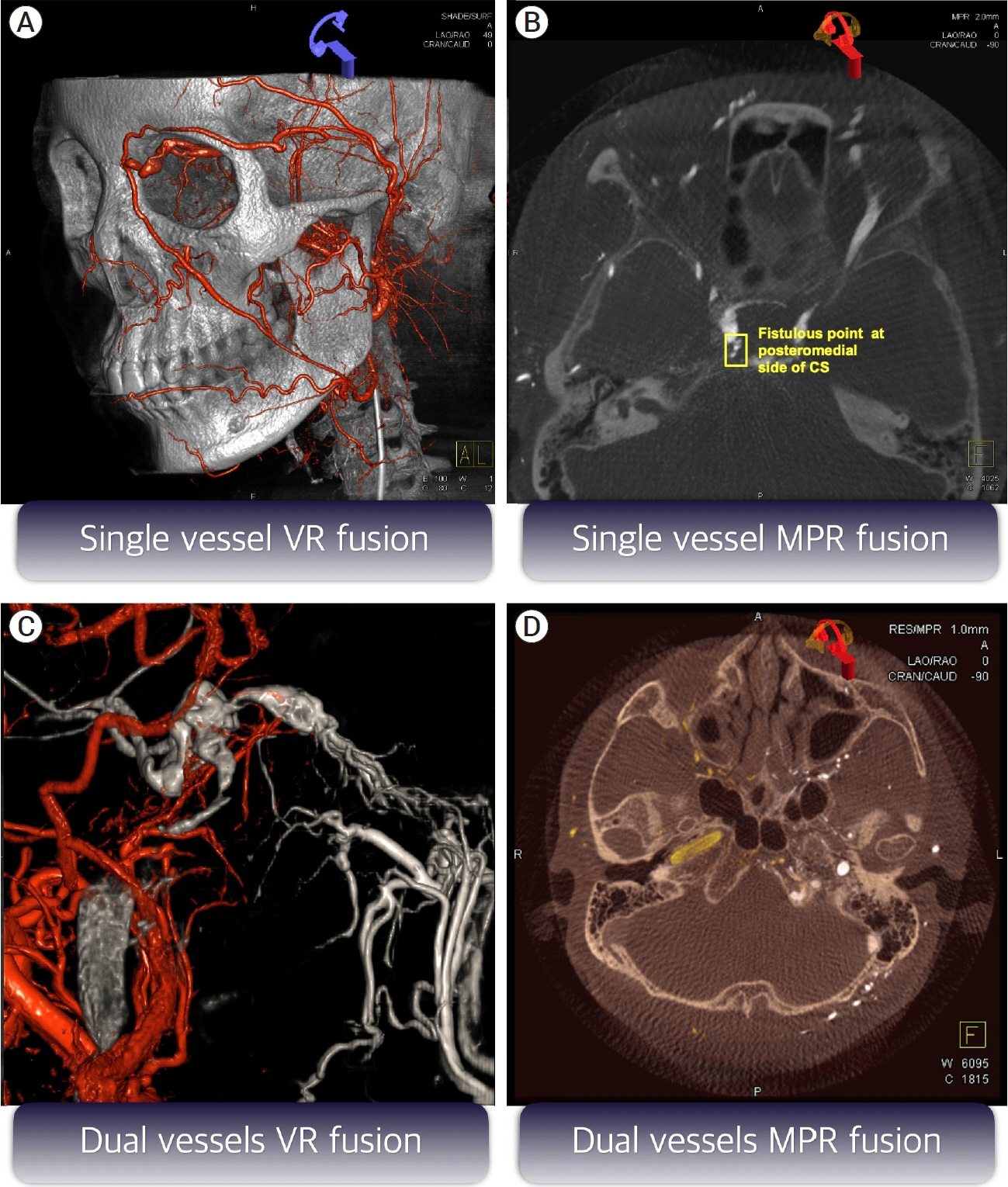
Image fusion technique using flat panel detector rotational angiography for transvenous embolization of intracranial dural arteriovenous fistula
- Affiliations
-
- 1Department of Neurosurgery, Seoul St Mary’s Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea
- 2Department of Radiology, Seoul St Mary’s Hospital, The Catholic University of Korea College of Medicine, Seoul, Korea
- KMID: 2546161
- DOI: http://doi.org/10.7461/jcen.2023.E2022.10.002
Abstract
- Precise evaluation of the feeders, fistulous points, and draining veins plays a key role for successful embolization of intracranial dural arteriovenous fistulas (DAVF). Digital subtraction angiography (DSA) is a gold standard diagnostic tool to assess the exact angioarchitecture of DAVFs. With the advent of new image postprocessing techniques, we lately have been able to apply image fusion techniques with two different image sets obtained with flat panel detector rotational angiography. This new technique can provide additional and better pretherapeutic information of DAVFs over the conventional 2D and 3D angiographies. In addition, it can be used during the endovascular treatment to help the accurate and precise navigation of the microcatheter and microguidwire inside the vessels and identify the proper location of microcatheter in the targeted shunting pouch. In this study, we briefly review the process of an image fusion technique and introduce our clinical application for treating DAVFs, especially focused on the transvenous embolization.
Keyword
Figure
Reference
-
1. Alexandre AM, Visconti E, Lozupone E, D’Argento F, Pedicelli A. Embolization of dural arteriovenous fistula of the cavernous sinus through percutaneous ultrasound-guided puncture of the facial vein. World Neurosurg. 2017; Mar. 99:812.2. Benndorf G, Bender A, Lehmann R, Lanksch W. Transvenous occlusion of dural cavernous sinus fistulas through the thrombosed inferior petrosal sinus: Report of four cases and review of the literature. Surg Neurol. 2000; Jul. 54(1):42–54.3. Biondi A, Milea D, Cognard C, Ricciardi GK, Bonneville F, van Effenterre R. Cavernous sinus dural fistulae treated by transvenous approach through the facial vein: Report of seven cases and review of the literature. AJNR Am J Neuroradiol. 2003; Jun-Jul. 24(6):1240–6.4. Borden JA, Wu JK, Shucart WA. A proposed classification for spinal and cranial dural arteriovenous fistulous malformations and implications for treatment. J Neurosurg. 1995; Feb. 82(2):166–79.5. Caton MT, Narsinh KH, Baker A, Dowd CF, Higashida RT, Cooke DL, et al. Dural arteriovenous fistulas of the foramen magnum region: Clinical features and angioarchitectural phenotypes. AJNR Am J Neuroradiol. 2021; Aug. 42(8):1486–91.6. Cho YD, Rhim JK, Yoo DH, Kang HS, Kim JE, Cho WS, et al. Transvenous microguidewire looping technique for breach of ipsilateral inferior petrosal sinus occlusions en route to cavernous sinus dural arteriovenous fistulas. Interv Neuroradiol. 2016; Oct. 22(5):590–5.7. Choi JH, Cho DY, Shin YS, Kim BS. Intraprocedural flat panel detector rotational angiography and an image fusion technique for delivery of a microcatheter into the targeted shunt pouch of a dural arteriovenous fistula. AJNR Am J Neuroradiol. 2020; Oct. 41(10):1876–8.8. Choi JH, Jo KI, Kim KH, Jeon P, Yeon JY, Kim JS, et al. Early rebleeding of intracranial dural arteriovenous fistulas after an intracranial hemorrhage. Acta Neurochir (Wien). 2017; Aug. 159(8):1479–87.9. Choi JH, Shin YS, Kim BS. Making microguidewire loop facilitates navigation through tortuous or abruptly angulated head and neck veins to access cavernous sinus dural arteriovenous fistulas. World Neurosurg. 2019; Sep. 129:e561–5.10. Cognard C, Gobin YP, Pierot L, Bailly AL, Houdart E, Casasco A, et al. Cerebral dural arteriovenous fistulas: Clinical and angiographic correlation with a revised classification of venous drainage. Radiology. 1995; Mar. 194(3):671–80.11. Fukuda K, Higashi T, Okawa M, Iwaasa M, Abe H, Inoue T. Fusion technique using three-dimensional digital subtraction angiography in the evaluation of complex cerebral and spinal vascular malformations. World Neurosurg. 2016; Jan. 85:353–8.12. Karygiannis MN, Szatmary Z, Claudino PA, Houdart E. Facial vein catheterization for transvenous embolization of the cavernous sinus. Technique and advantages of the direct jugular vein approach - Report of three cases. Interv Neuroradiol. 2006; Mar. 12(1):25–30.13. Kuwayama N, Akioka N. Complications of endovascular treatment of intracranial dural arteriovenous fistulas. Acta Neurochir Suppl. 2021; 132:123–7.14. Li H, Wan F, Li J, Sheng L, Li G, Chen G, et al. Flat detector computed tomography-based “dual vessel fusion” technique for diagnosis and surgical planning in the management of dural arteriovenous fistula. World Neurosurg. 2015; Aug. 84(2):520–7.15. Oh SH, Choi JH, Kim BS, Lee KS, Shin YS. Treatment outcomes according to various treatment modalities for intracranial dural arteriovenous fistulas in the Onyx era: A 10- year single-center experience. World Neurosurg. 2019; Jun. 126:e825–34.16. Söderman M, Pavic L, Edner G, Holmin S, Andersson T. Natural history of dural arteriovenous shunts. Stroke. 2008; Jun. 39(6):1735–9.17. Spittau B, Millán DS, El-Sherifi S, Hader C, Singh TP, Motschall E, et al. Dural arteriovenous fistulas of the hypoglossal canal: Systematic review on imaging anatomy, clinical findings, and endovascular management. J Neurosurg. 2015; Apr. 122(4):883–903.18. Tanoue S, Kiyosue H, Mori H, Hongo N, Okahara M, Kubo T. Fusion imaging using subtracted and unsubtracted rotational angiography for pretherapeutic evaluation of dural arteriovenous fistulas. Jpn J Radiol. 2014; Oct. 32(10):600–7.19. van Dijk JM, terBrugge KG, Willinsky RA, Wallace MC. Clinical course of cranial dural arteriovenous fistulas with long-term persistent cortical venous reflux. Stroke. 2002; May. 33(5):1233–6.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Occurrence of De Novo Dural Arteriovenous Fistula after Transvenous Embolization of Dural Arteriovenous Fistula : Case Reports of Two Patients
- Transvenous coil embolization of hypoglossal canal dural arteriovenous fistula using detachable coils: A case report
- Transvenous injection of n-butyl 2-cyanoacrylate to obliterate the pathologic cavernous sinus as a salvage technique for incompletely obliterated complex cavernous sinus dural arteriovenous fistula after transvenous coil embolization
- Occurrence of Metachronous Intracranial Dural Arteriovenous Fistula after Embolization of Intracranial Dural Arteriovenous Fistula: A Case Report
- Dural Arteriovenous Fistula Involving Transverse Sinus: Successful Embolization Using Onyx(R)