Korean Circ J.
2023 Sep;53(9):606-618. 10.4070/kcj.2023.0035.
Prognostic and Safety Implications of Renin-Angiotensin-Aldosterone System Inhibitors in Hypertrophic Cardiomyopathy: A Real-World Observation Over 2,000 Patients
- Affiliations
-
- 1Cardiovascular Center, Seoul National University Hospital, Seoul, Korea
- 2Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea
- 3Cardiovascular Center, Seoul National University Bundang Hospital, Seongnam, Korea
- KMID: 2545954
- DOI: http://doi.org/10.4070/kcj.2023.0035
Abstract
- Background and Objectives
The prognostic or safety implication of renin-angiotensinaldosterone system inhibitors (RASi) in hypertrophic cardiomyopathy (HCM) are not well established, mainly due to concerns regarding left ventricular outflow tract (LVOT) obstruction aggravation. We investigated the implications of RASi in a sizable number of HCM patients.
Methods
We enrolled 2,104 consecutive patients diagnosed with HCM in 2 tertiary university hospitals and followed up for five years. RASi use was defined as the administration of RASi after diagnostic confirmation of HCM. The primary and secondary outcomes were all-cause mortality and hospitalization for heart failure (HHF).
Results
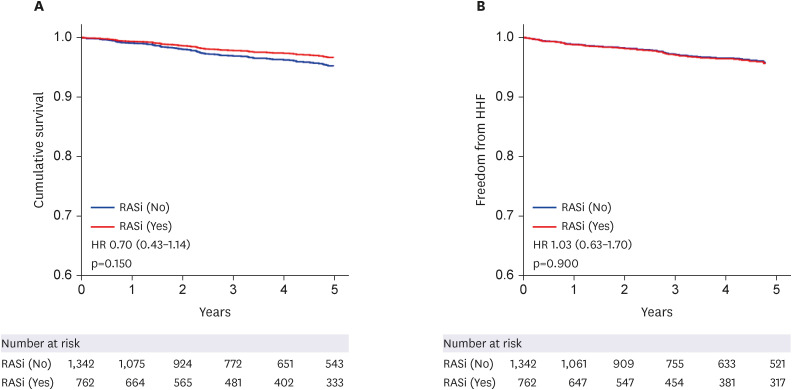
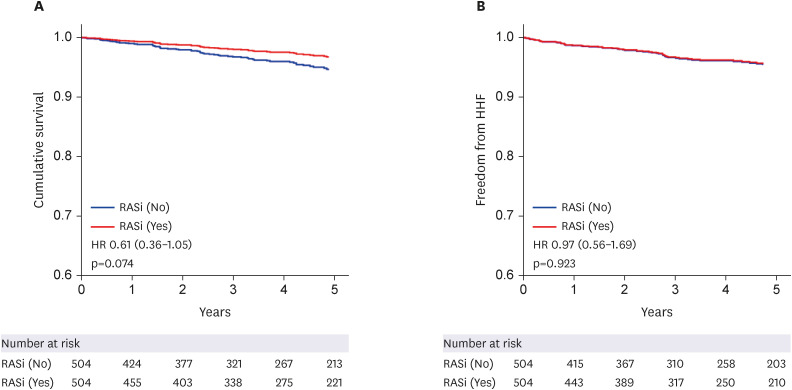
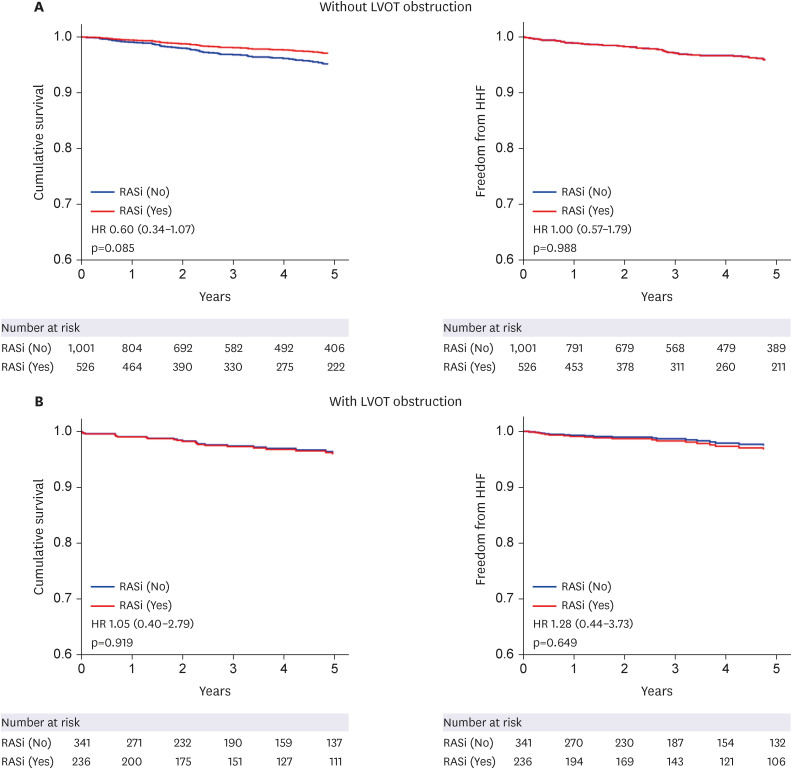
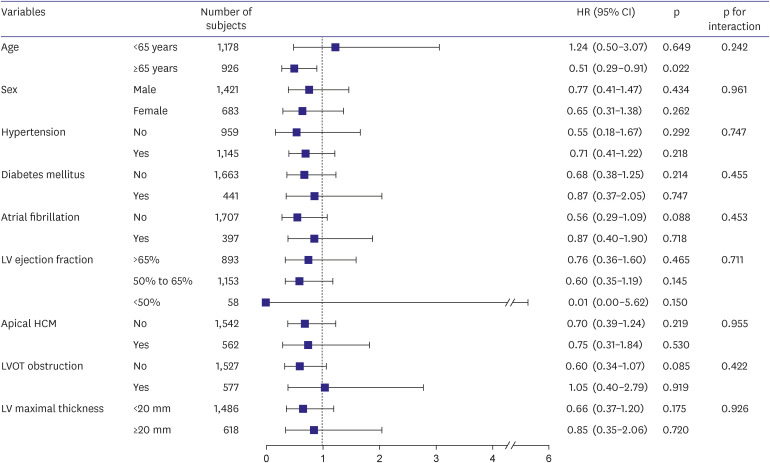
RASi were prescribed to 762 patients (36.2%). During a median follow-up of 48.1 months, 112 patients (5.3%) died, and 94 patients (4.5%) experienced HHF. Patients using RASi had less favorable baseline characteristics than those not using RASi, such as older age, more frequent history of comorbidities, and lower ejection fraction. Nonetheless, there was no difference in clinical outcomes between patients with and without RASi use (log-rank p=0.368 for all-cause mortality and log-rank p=0.443 for HHF). In multivariable analysis, patients taking RASi showed a comparable risk of all-cause mortality (hazard ratio [HR], 0.70, 95% confidence interval [CI], 0.43–1.14, p=0.150) and HHF (HR, 1.03, 95% CI, 0.63–1.70, p=0.900). In the subgroup analysis, there was no significant interaction of RASi use between subgroups stratified by LVOT obstruction, left ventricular (LV) ejection fraction, or maximal LV wall thickness.
Conclusions
RASi use was not associated with worse clinical outcomes. It might be safely administered in patients with HCM if clinically indicated.
Figure
Cited by 1 articles
-
Should We Use Renin-Angiotensin-Aldosterone System Inhibitors Routinely in Patients With Hypertrophic Cardiomyopathy?
Jae-Hyeong Park
Korean Circ J. 2023;53(9):619-620. doi: 10.4070/kcj.2023.0161.
Reference
-
1. Seidman CE, Seidman JG. Identifying sarcomere gene mutations in hypertrophic cardiomyopathy: a personal history. Circ Res. 2011; 108:743–750. PMID: 21415408.2. Ommen SR, Mital S, Burke MA, et al. 2020 AHA/ACC guideline for the diagnosis and treatment of patients with hypertrophic cardiomyopathy: executive summary: a report of the American College of Cardiology/American Heart Association joint committee on clinical practice guidelines. J Am Coll Cardiol. 2020; 76:3022–3055. PMID: 33229115.3. Lee HJ, Kim J, Chang SA, Kim YJ, Kim HK, Lee SC. Major clinical issues in hypertrophic cardiomyopathy. Korean Circ J. 2022; 52:563–575. PMID: 35929051.
Article4. Maron BJ. Clinical course and management of hypertrophic cardiomyopathy. N Engl J Med. 2018; 379:655–668. PMID: 30110588.5. Lee HJ, Kim HK, Lee SC, et al. Supplementary role of left ventricular global longitudinal strain for predicting sudden cardiac death in hypertrophic cardiomyopathy. Eur Heart J Cardiovasc Imaging. 2022; 23:1108–1116. PMID: 34542591.6. Choi YJ, Kim HK, Hwang IC, et al. Prognosis of patients with hypertrophic cardiomyopathy and low-normal left ventricular ejection fraction. Heart. 2023; 109:771–778. PMID: 36581445.
Article7. Choi YJ, Kim B, Rhee TM, et al. Augmented risk of ischemic stroke in hypertrophic cardiomyopathy patients without documented atrial fibrillation. Sci Rep. 2022; 12:15785. PMID: 36138115.
Article8. Kim M, Kim B, Choi YJ, et al. Sex differences in the prognosis of patients with hypertrophic cardiomyopathy. Sci Rep. 2021; 11:4854. PMID: 33649405.
Article9. Lee HJ, Kim HK, Lee SC, et al. Age-related sex differences in the outcomes of patients with hypertrophic cardiomyopathy. PLoS One. 2022; 17:e0264580. PMID: 35213653.
Article10. Pfeffer MA, McMurray JJ, Velazquez EJ, et al. Valsartan, captopril, or both in myocardial infarction complicated by heart failure, left ventricular dysfunction, or both. N Engl J Med. 2003; 349:1893–1906. PMID: 14610160.
Article11. Julius S, Kjeldsen SE, Weber M, et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet. 2004; 363:2022–2031. PMID: 15207952.
Article12. Park CS, Kim B, Rhee TM, et al. Association between renin-angiotensin-aldosterone system blockade and clinical outcomes in patients with hypertension: real-world observation from a nationwide hypertension cohort. Clin Res Cardiol. 2023; [Epub ahead of print].
Article13. Devereux RB, Dahlöf B, Gerdts E, et al. Regression of hypertensive left ventricular hypertrophy by losartan compared with atenolol: the Losartan Intervention for Endpoint Reduction in Hypertension (LIFE) trial. Circulation. 2004; 110:1456–1462. PMID: 15326072.
Article14. Teekakirikul P, Eminaga S, Toka O, et al. Cardiac fibrosis in mice with hypertrophic cardiomyopathy is mediated by non-myocyte proliferation and requires Tgf-β. J Clin Invest. 2010; 120:3520–3529. PMID: 20811150.
Article15. Araujo AQ, Arteaga E, Ianni BM, Buck PC, Rabello R, Mady C. Effect of Losartan on left ventricular diastolic function in patients with nonobstructive hypertrophic cardiomyopathy. Am J Cardiol. 2005; 96:1563–1567. PMID: 16310441.
Article16. Authors/Task Force members. Elliott PM, Anastasakis A, et al. 2014 ESC guidelines on diagnosis and management of hypertrophic cardiomyopathy: the task force for the diagnosis and management of hypertrophic cardiomyopathy of the European Society of Cardiology (ESC). Eur Heart J. 2014; 35:2733–2779. PMID: 25173338.
Article17. Axelsson A, Iversen K, Vejlstrup N, et al. Efficacy and safety of the angiotensin II receptor blocker losartan for hypertrophic cardiomyopathy: the INHERIT randomised, double-blind, placebo-controlled trial. Lancet Diabetes Endocrinol. 2015; 3:123–131. PMID: 25533774.
Article18. Ho CY, Day SM, Axelsson A, et al. Valsartan in early-stage hypertrophic cardiomyopathy: a randomized phase 2 trial. Nat Med. 2021; 27:1818–1824. PMID: 34556856.
Article19. Lang RM, Badano LP, Mor-Avi V, et al. Recommendations for cardiac chamber quantification by echocardiography in adults: an update from the American Society of Echocardiography and the European Association of Cardiovascular Imaging. Eur Heart J Cardiovasc Imaging. 2015; 16:233–270. PMID: 25712077.
Article20. Senni M, McMurray JJ, Wachter R, et al. Initiating sacubitril/valsartan (LCZ696) in heart failure: results of TITRATION, a double-blind, randomized comparison of two uptitration regimens. Eur J Heart Fail. 2016; 18:1193–1202. PMID: 27170530.
Article21. Olivotto I, Cecchi F, Poggesi C, Yacoub MH. Patterns of disease progression in hypertrophic cardiomyopathy: an individualized approach to clinical staging. Circ Heart Fail. 2012; 5:535–546. PMID: 22811549.22. Bois JP, Geske JB, Foley TA, Ommen SR, Pellikka PA. Comparison of maximal wall thickness in hypertrophic cardiomyopathy differs between magnetic resonance imaging and transthoracic echocardiography. Am J Cardiol. 2017; 119:643–650. PMID: 27956002.
Article23. Lee HJ, Kim HK, Rhee TM, et al. Left atrial reservoir strain-based left ventricular diastolic function grading and incident heart failure in hypertrophic cardiomyopathy. Circ Cardiovasc Imaging. 2022; 15:e013556. PMID: 35439039.
Article24. Goel SS, Kleiman NS, Zoghbi WA, Reardon MJ, Kapadia SR. Renin-angiotensin system blockade in aortic stenosis: implications before and after aortic valve replacement. J Am Heart Assoc. 2020; 9:e016911. PMID: 32893727.
Article25. Goh SS, Sia CH, Ngiam NJ, et al. Effect of renin-angiotensin blockers on left ventricular remodeling in severe aortic stenosis. Am J Cardiol. 2017; 119:1839–1845. PMID: 28390678.
Article26. Park JB, Kim DH, Lee H, et al. Obesity and metabolic health status are determinants for the clinical expression of hypertrophic cardiomyopathy. Eur J Prev Cardiol. 2020; 27:1849–1857. PMID: 31787021.
Article27. Yoshibayashi M, Kamiya T, Saito Y, Matsuo H. Increased plasma levels of brain natriuretic peptide in hypertrophic cardiomyopathy. N Engl J Med. 1993; 329:433–434. PMID: 8326985.
Article28. Shimada YJ, Raita Y, Liang LW, et al. Comprehensive proteomics profiling reveals circulating biomarkers of hypertrophic cardiomyopathy. Circ Heart Fail. 2021; 14:e007849. PMID: 34192899.
Article29. Ashrafian H, McKenna WJ, Watkins H. Disease pathways and novel therapeutic targets in hypertrophic cardiomyopathy. Circ Res. 2011; 109:86–96. PMID: 21700950.
Article30. Maron BJ, Desai MY, Nishimura RA, et al. Diagnosis and evaluation of hypertrophic cardiomyopathy: JACC state-of-the-art review. J Am Coll Cardiol. 2022; 79:372–389. PMID: 35086660.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Use of Angiotensin Converting Enzyme Inhibitors and Angiotensin Receptor Blockers: A Closer Look at Hyperkalemia
- New drugs for treatment of hypertension
- Upregulation of Renin-angiotensin, Endothelin and C-type Natriuretic Peptide in Rat Glomerulus with Bilateral Ureteral Obstruction
- Renin Angiotensin System in Rabbit Corpus Cavernosum: Functional Characterization of Angiotensin II Receptors
- Renin-Angiotensin-Aldosterone System Blockade and Renal Protection in Diabetic Nephropathy