Cancer Res Treat.
2023 Apr;55(2):684-692. 10.4143/crt.2022.1434.
Current Treatment Patterns and the Role of Upfront Autologous Stem Cell Transplantation in Patients with Peripheral T-Cell Lymphoma: A Korean Nationwide, Multicenter Prospective Registry Study (CISL 1404)
- Affiliations
-
- 1Department of Oncology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- 2Department of Internal Medicine, Seoul National University Hospital, Seoul, Korea
- 3Division of Hematology and Oncology, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Department of Medicine, Dongsan Medical Center, Keimyung University School of Medicine, Daegu, Korea
- 5Department of Internal Medicine, Gyeongsang National University Hospital, Gyeongsang National University College of Medicine, Jinju, Korea
- 6Department of Internal Medicine, Jeonbuk National University Hospital, Jeonju, Korea
- 7Department of Internal Medicine, Korea University Anam Hospital, Seoul, Korea
- 8Department of Internal Medicine, Yeungnam University College of Medicine, Daegu, Korea
- 9Department of Internal Medicine, Korea Cancer Center Hospital, Korea Institute of Radiological and Medical Sciences, Seoul, Korea
- 10Department of Internal Medicine, Chung-Ang University Hospital, Seoul, Korea
- 11Department of Internal Medicine, Gachon University of Gil Medical Center, Gachon University College of Medicine, Incheon, Korea
- 12Department of Internal Medicine, Inje University Busan Paik Hospital, Busan, Korea
- 13Department of Internal Medicine, Hanyang University College of Medicine, Seoul, Korea
- 14Department of Hematology and Oncology, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 15Center for Hematologic Malignancies, National Cancer Center, Goyang, Korea
- 16Department of Internal Medicine, Hallym University Sacred Heart Hospital, Anyang, Korea
- 17Department of Hematology-Oncology, Ajou University School of Medicine, Suwon, Korea
- 18Department of Internal Medicine, Hanyang University Guri Hospital, Hanyang University College of Medicine, Guri, Korea
- 19Department of Internal Medicine, Inje University Sanggye Paik Hospital, Seoul, Korea
- 20Department of Internal Medicine, Chungbuk National University Hospital, Cheongju, Korea
- KMID: 2541255
- DOI: http://doi.org/10.4143/crt.2022.1434
Abstract
- Purpose
We conducted a nationwide, multicenter, prospective registry study for newly diagnosed patients with peripheral T-cell lymphoma (PTCL) to better define the clinical characteristics, treatment patterns, survival outcomes, and the role of upfront autologous stem cell transplantation (ASCT) in these patients.
Materials and Methods
Patients with PTCL receiving chemotherapy with curative intent were registered and prospectively monitored. All patients were pathologically diagnosed with PTCL.
Results
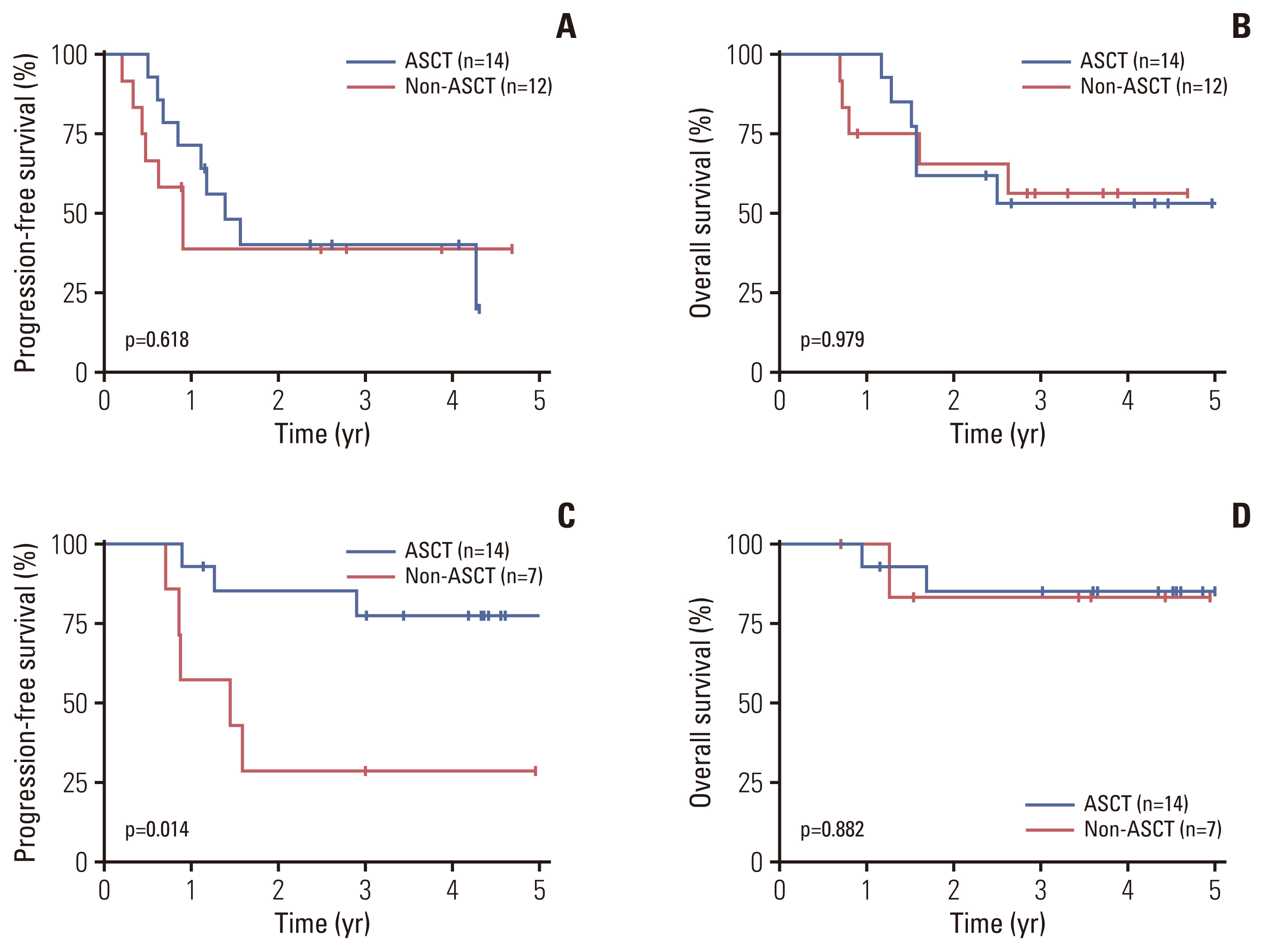
A total of 191 patients with PTCL were enrolled in this prospective registry study. PTCL, not otherwise specified (PTCL-NOS) was the most common pathologic subtype (n=80, 41.9%), followed by angioimmunoblastic T-cell lymphoma (AITL) (n=60, 31.4%). With a median follow-up duration of 3.9 years, the 3-year progression-free survival (PFS) and overall survival (OS) rates were 39.5% and 60.4%, respectively. The role of upfront ASCT was evaluated in patients who were considered transplant-eligible (n=59). ASCT was performed as an upfront consolidative treatment in 32 (54.2%) of these patients. There were no significant differences in PFS and OS between the ASCT and non-ASCT groups for all patients (n=59) and for patients with PTCL-NOS (n=26). However, in patients with AITL, the ASCT group was associated with significantly better PFS than the non-ASCT group, although there was no significant difference in OS.
Conclusion
The current study demonstrated that the survival outcomes with the current treatment options remain poor for patients with PTCL-NOS. Upfront ASCT may provide a survival benefit for patients with AITL, but not PTCL-NOS.
Figure
Reference
-
References
1. Zain JM, Hanona P. Aggressive T-cell lymphomas: 2021 updates on diagnosis, risk stratification and management. Am J Hematol. 2021; 96:1027–46.
Article2. Swerdlow SH, Campo E, Pileri SA, Harris NL, Stein H, Siebert R, et al. The 2016 revision of the World Health Organization classification of lymphoid neoplasms. Blood. 2016; 127:2375–90.
Article3. Vose J, Armitage J, Weisenburger D; International T-Cell Lymphoma Project. International peripheral T-cell and natural killer/T-cell lymphoma study: pathology findings and clinical outcomes. J Clin Oncol. 2008; 26:4124–30.
Article4. Yoon SE, Song Y, Kim SJ, Yoon DH, Chen TY, Koh Y, et al. Comprehensive analysis of peripheral T-cell and natural killer/T-cell lymphoma in Asian patients: a multinational, multicenter, prospective registry study in Asia. Lancet Reg Health West Pac. 2021; 10:100126.
Article5. Ellin F, Landstrom J, Jerkeman M, Relander T. Real-world data on prognostic factors and treatment in peripheral T-cell lymphomas: a study from the Swedish Lymphoma Registry. Blood. 2014; 124:1570–7.
Article6. Savage KJ, Chhanabhai M, Gascoyne RD, Connors JM. Characterization of peripheral T-cell lymphomas in a single North American institution by the WHO classification. Ann Oncol. 2004; 15:1467–75.
Article7. Park SI, Horwitz SM, Foss FM, Pinter-Brown LC, Carson KR, Rosen ST, et al. The role of autologous stem cell transplantation in patients with nodal peripheral T-cell lymphomas in first complete remission: report from COMPLETE, a prospective, multicenter cohort study. Cancer. 2019; 125:1507–17.
Article8. d’Amore F, Relander T, Lauritzsen GF, Jantunen E, Hagberg H, Anderson H, et al. Up-front autologous stem-cell transplantation in peripheral T-cell lymphoma: NLG-T-01. J Clin Oncol. 2012; 30:3093–9.9. Reimer P, Rudiger T, Geissinger E, Weissinger F, Nerl C, Schmitz N, et al. Autologous stem-cell transplantation as first-line therapy in peripheral T-cell lymphomas: results of a prospective multicenter study. J Clin Oncol. 2009; 27:106–13.
Article10. Fossard G, Broussais F, Coelho I, Bailly S, Nicolas-Virelizier E, Toussaint E, et al. Role of up-front autologous stem-cell transplantation in peripheral T-cell lymphoma for patients in response after induction: an analysis of patients from LYSA centers. Ann Oncol. 2018; 29:715–23.
Article11. Cheson BD, Fisher RI, Barrington SF, Cavalli F, Schwartz LH, Zucca E, et al. Recommendations for initial evaluation, staging, and response assessment of Hodgkin and non-Hodgkin lymphoma: the Lugano classification. J Clin Oncol. 2014; 32:3059–68.
Article12. Adams SV, Newcomb PA, Shustov AR. Racial patterns of peripheral T-cell lymphoma incidence and survival in the United States. J Clin Oncol. 2016; 34:963–71.
Article13. Shi Y. Current status and progress of lymphoma management in China. Int J Hematol. 2018; 107:405–12.
Article14. Fuji S, Kida S, Nakata K, Morishima T, Miyashiro I, Ishikawa J. Increased incidence of adult T cell leukemia-lymphoma and peripheral T cell lymphoma-not otherwise specified with limited improvement in overall survival: a retrospective analysis using data from the population-based Osaka Cancer Registry. Ann Hematol. 2021; 100:157–65.
Article15. Advani RH, Skrypets T, Civallero M, Spinner MA, Manni M, Kim WS, et al. Outcomes and prognostic factors in angioimmunoblastic T-cell lymphoma: final report from the international T-cell Project. Blood. 2021; 138:213–20.16. Tang T, Khoo LP, Lim C, Ham JS, Kim SJ, Hong H, et al. Outcomes of patients with peripheral T-cell lymphoma in first complete remission: data from three tertiary Asian cancer centers. Blood Cancer J. 2017; 7:653.
Article17. Maurer MJ, Ghesquieres H, Jais JP, Witzig TE, Haioun C, Thompson CA, et al. Event-free survival at 24 months is a robust end point for disease-related outcome in diffuse large B-cell lymphoma treated with immunochemotherapy. J Clin Oncol. 2014; 32:1066–73.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Scleroderma following Autologous Peripheral Stem Cell Transplantation
- Thrombotic Thrombocytopenic Purpura after Autologous Peripheral Blood Stem Cell Transplantation
- Autoimmune Diseases after Autologous Hematopoietic Stem Cell Transplantation in Patients with Non-Hodgkin's Lymphoma
- The Evolving Role of Myeloablative Chemotherapy with Stem Cell Transplantation for the Treatment of Autoimmune Disease
- A Case of Mantle Cell Lymphoma Treated with Autologous Stem Cell Transplantation and Rituximab