J Korean Med Sci.
2023 Jan;38(4):e24. 10.3346/jkms.2023.38.e24.
Long-Term Risk of Cardiovascular Disease Among Type 2 Diabetes Patients According to Average and Visit-to-Visit Variations of HbA1c Levels During the First 3 Years of Diabetes Diagnosis
- Affiliations
-
- 1College of Pharmacy, Sookmyung Women’s University, Seoul, Korea
- 2Department of Biostatistics, Clinical Research Coordinating Center, Catholic Medical Center, The Catholic University of Korea, Seoul, Korea
- 3Division of Endocrinology and Metabolism, Department of Internal Medicine, Seoul St. Mary’s Hospital, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 4Department of Preventive Medicine, College of Medicine, The Catholic University of Korea, Seoul, Korea
- 5Department of Medical Informatics, College of Medicine, The Catholic University of Korea, Seoul, Korea
- KMID: 2539190
- DOI: http://doi.org/10.3346/jkms.2023.38.e24
Abstract
- Background
It remains unclear whether a combination of glycemic variability and glycated hemoglobin (HbA1c) status leads to a higher incidence of cardiovascular disease (CVD). Therefore, to investigate CVD risk according to the glucose control status during early diabetes, we examined visit-to-visit HbA1c variability among patients with type 2 diabetes (T2DM).
Methods
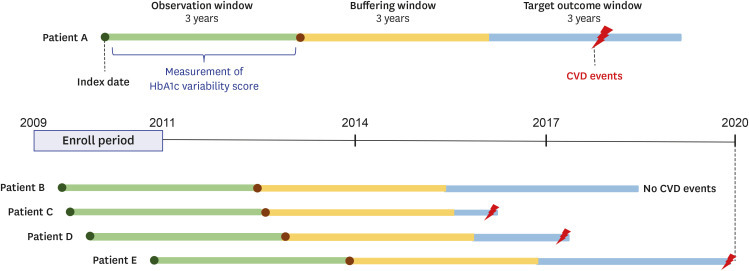
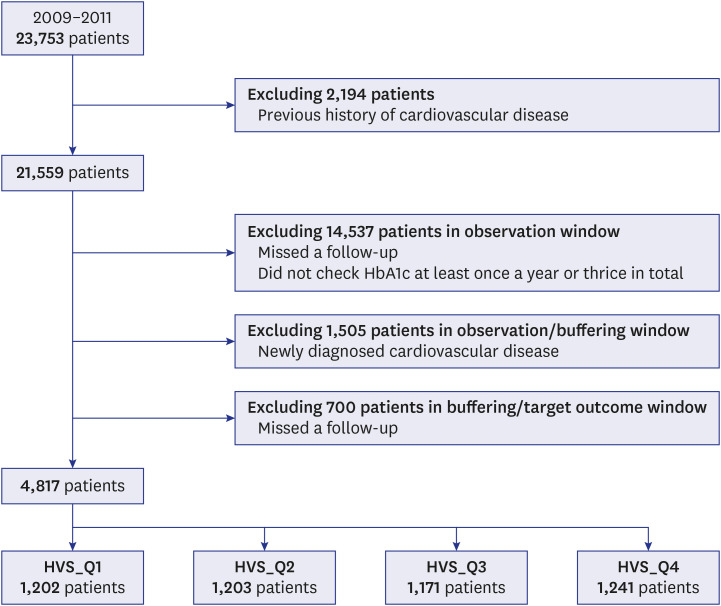
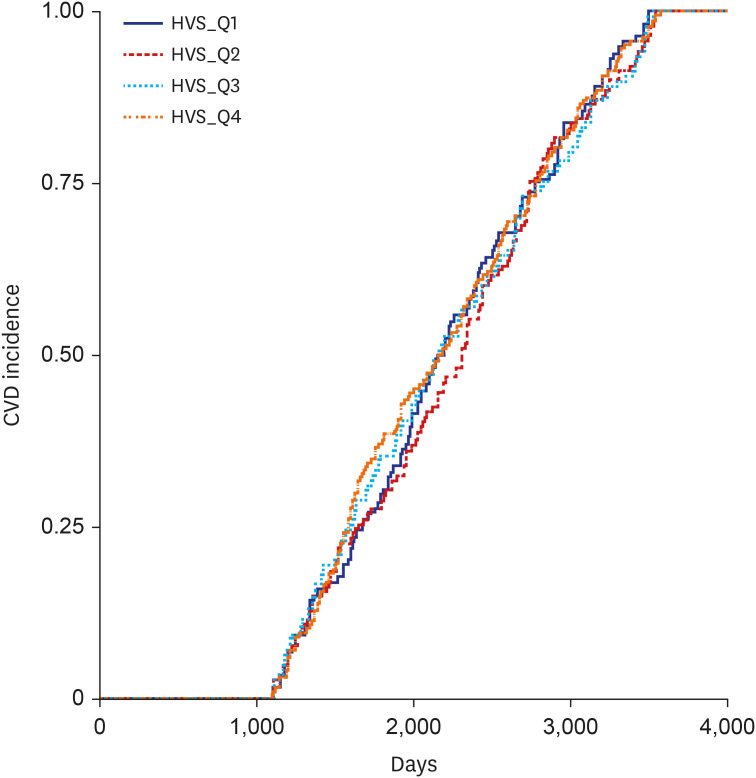
In this 9-year retrospective study, we measured HbA1c levels at each visit and tracked the change in HbA1c levels for 3 years after the first presentation (observation window) in newly diagnosed T2DM patients. We later assessed the occurrence of CVD in the last 3 years (target outcome window) of the study period after allowing a 3-year buffering window. The HbA1c variability score (HVS; divided into quartiles, HVS_Q1–4) was used to determine visit-to-visit HbA1c variability.
Results
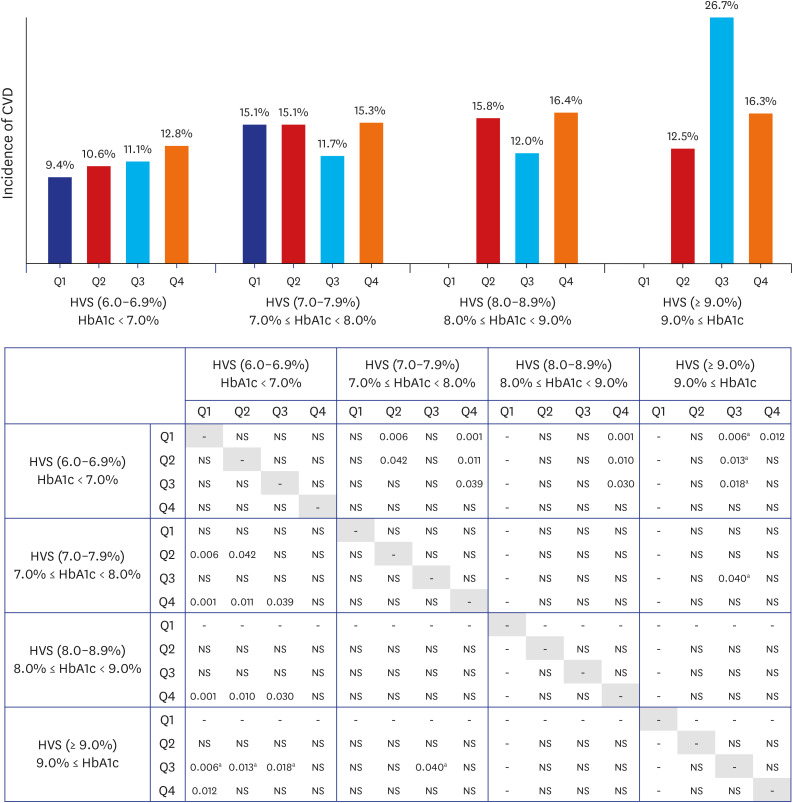
Among 4,817 enrolled T2DM patients, the mean HbA1c level was < 7% for the first 3 years. The group with the lowest HVS had the lowest rate of CVD (9.4%; 104/1,109 patients). The highest incidence of CVD of 26.7% (8/30 patients) was found in HVS [≥ 9.0%]_Q3, which was significantly higher than that in HVS [6.0–6.9%]_Q1 (P = 0.006), HVS [6.0–6.9%]_Q2 (P = 0.013), HVS [6.0–6.9%]_Q3 (P = 0.018), and HVS [7.0–7.9%]_Q3 (P = 0.040).
Conclusion
To our knowledge, this is the first long-term study to analyze the importance of both HbA1c change and visit-to-visit HbA1c variability during outpatient visits within the first 3 years. Lowering glucose levels during early diabetes may be more critical than reducing visit-to-visit HbA1c variability.
Keyword
Figure
Reference
-
1. Weykamp C. HbA1c: a review of analytical and clinical aspects. Ann Lab Med. 2013; 33(6):393–400. PMID: 24205486.2. Stratton IM, Adler AI, Neil HA, Matthews DR, Manley SE, Cull CA, et al. Association of glycaemia with macrovascular and microvascular complications of type 2 diabetes (UKPDS 35): prospective observational study. BMJ. 2000; 321(7258):405–412. PMID: 10938048.3. UK Prospective Diabetes Study (UKPDS) Group. Intensive blood-glucose control with sulphonylureas or insulin compared with conventional treatment and risk of complications in patients with type 2 diabetes (UKPDS 33). Lancet. 1998; 352(9131):837–853. PMID: 9742976.4. Ohkubo Y, Kishikawa H, Araki E, Miyata T, Isami S, Motoyoshi S, et al. Intensive insulin therapy prevents the progression of diabetic microvascular complications in Japanese patients with non-insulin-dependent diabetes mellitus: a randomized prospective 6-year study. Diabetes Res Clin Pract. 1995; 28(2):103–117. PMID: 7587918.5. ACCORD Study Group. Cushman WC, Evans GW, Byington RP, Goff DC Jr, Grimm RH Jr, et al. Effects of intensive blood-pressure control in type 2 diabetes mellitus. N Engl J Med. 2010; 362(17):1575–1585. PMID: 20228401.6. Yang Y, Lee EY, Cho JH, Park YM, Ko SH, Yoon KH, et al. Cardiovascular autonomic neuropathy predicts higher HbA1c variability in subjects with type 2 diabetes mellitus. Diabetes Metab J. 2018; 42(6):496–512. PMID: 30302965.7. Li S, Nemeth I, Donnelly L, Hapca S, Zhou K, Pearson ER. Visit-to-visit HbA1c variability is associated with cardiovascular diseases and microvascular complications in patients with newly diagnosed type 2 diabetes. Diabetes Care. 2020; 43(2):426–432. PMID: 31727686.8. Yang CY, Su PF, Hung JY, Ou HT, Kuo S. Comparative predictive ability of visit-to-visit HbA1c variability measures for microvascular disease risk in type 2 diabetes. Cardiovasc Diabetol. 2020; 19(1):105. PMID: 32631323.9. Wadén J, Forsblom C, Thorn LM, Gordin D, Saraheimo M, Groop PH, et al. A1C variability predicts incident cardiovascular events, microalbuminuria, and overt diabetic nephropathy in patients with type 1 diabetes. Diabetes. 2009; 58(11):2649–2655. PMID: 19651819.10. Forbes A, Murrells T, Mulnier H, Sinclair AJ. Mean HbA1c, HbA1c variability, and mortality in people with diabetes aged 70 years and older: a retrospective cohort study. Lancet Diabetes Endocrinol. 2018; 6(6):476–486. PMID: 29674135.11. Marcovecchio ML, Dalton RN, Chiarelli F, Dunger DB. A1C variability as an independent risk factor for microalbuminuria in young people with type 1 diabetes. Diabetes Care. 2011; 34(4):1011–1013. PMID: 21335371.12. Takao T, Matsuyama Y, Yanagisawa H, Kikuchi M, Kawazu S. Association between HbA1c variability and mortality in patients with type 2 diabetes. J Diabetes Complications. 2014; 28(4):494–499. PMID: 24703414.13. Kim HS, Kim DJ, Yoon KH. Medical big data is not yet available: why we need realism rather than exaggeration. Endocrinol Metab. 2019; 34(4):349–354.14. Shin SY, Kim HS. Data pseudonymization in a range that does not affect data quality: correlation with the degree of participation of clinicians. J Korean Med Sci. 2021; 36(44):e299. PMID: 34783216.15. Nathan DM. DCCT/EDIC Research Group. The diabetes control and complications trial/epidemiology of diabetes interventions and complications study at 30 years: overview. Diabetes Care. 2014; 37(1):9–16. PMID: 24356592.16. Lind M, Svensson AM, Kosiborod M, Gudbjörnsdottir S, Pivodic A, Wedel H, et al. Glycemic control and excess mortality in type 1 diabetes. N Engl J Med. 2014; 371(21):1972–1982. PMID: 25409370.17. Risso A, Mercuri F, Quagliaro L, Damante G, Ceriello A. Intermittent high glucose enhances apoptosis in human umbilical vein endothelial cells in culture. Am J Physiol Endocrinol Metab. 2001; 281(5):E924–E930. PMID: 11595647.18. Downie E, Craig ME, Hing S, Cusumano J, Chan AK, Donaghue KC. Continued reduction in the prevalence of retinopathy in adolescents with type 1 diabetes: role of insulin therapy and glycemic control. Diabetes Care. 2011; 34(11):2368–2373. PMID: 22025782.19. Su G, Mi SH, Li Z, Tao H, Yang HX, Zheng H. Prognostic value of early in-hospital glycemic excursion in elderly patients with acute myocardial infarction. Cardiovasc Diabetol. 2013; 12(1):33. PMID: 23399749.20. Kim CS, Park SY, Yu SH, Kang JG, Ryu OH, Lee SJ, et al. Is A1C variability an independent predictor for the progression of atherosclerosis in type 2 diabetic patients? Korean Diabetes J. 2010; 34(3):174–181. PMID: 20617078.21. Penno G, Solini A, Zoppini G, Orsi E, Fondelli C, Zerbini G, et al. Hemoglobin A1c variability as an independent correlate of cardiovascular disease in patients with type 2 diabetes: a cross-sectional analysis of the renal insufficiency and cardiovascular events (RIACE) Italian multicenter study. Cardiovasc Diabetol. 2013; 12(1):98. PMID: 23829205.22. Kim HS, Kim JH. Proceed with caution when using real world data and real world evidence. J Korean Med Sci. 2019; 34(4):e28. PMID: 30686950.23. Mita T, Katakami N, Okada Y, Yoshii H, Osonoi T, Nishida K, et al. Protocol of a prospective observational study on the relationship between glucose fluctuation and cardiovascular events in patients with type 2 diabetes. Diabetes Ther. 2019; 10(5):1565–1575. PMID: 31338757.24. Wang MT, Tsai CL, Lo YW, Liou JT, Lee WJ, Lai IC. Risk of stroke associated with inhaled ipratropium bromide in chronic obstructive pulmonary disease: a population-based nested case-control study. Int J Cardiol. 2012; 158(2):279–284. PMID: 22386700.25. Xu Y, Fu EL, Trevisan M, Jernberg T, Sjölander A, Clase CM, et al. Stopping renin-angiotensin system inhibitors after hyperkalemia and risk of adverse outcomes. Am Heart J. 2022; 243:177–186. PMID: 34610282.26. Ravaut M, Sadeghi H, Leung KK, Volkovs M, Kornas K, Harish V, et al. Predicting adverse outcomes due to diabetes complications with machine learning using administrative health data. NPJ Digit Med. 2021; 4(1):24. PMID: 33580109.27. Lei J, Ploner A, Elfström KM, Wang J, Roth A, Fang F, et al. HPV vaccination and the risk of invasive cervical cancer. N Engl J Med. 2020; 383(14):1340–1348. PMID: 32997908.28. Dehlendorff C, Baandrup L, Kjaer SK. Real-world effectiveness of human papillomavirus vaccination against vulvovaginal high-grade precancerous lesions and cancers. J Natl Cancer Inst. 2021; 113(7):869–874. PMID: 33377930.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Blood Pressure Variability and Cardiovascular Risk
- Do Type 1 and Type 2 Diabetes Have the Same Vascular Complications?
- Increased Visit-to-Visit Liver Enzyme Variability Is Associated with Incident Diabetes: A Community-Based 12-Year Prospective Cohort Study
- Impact of COVID-19 lockdown on blood glucose levels in pediatric patients with type 1 diabetes mellitus
- Lipid Variability and Diabetes Mellitus