J Cerebrovasc Endovasc Neurosurg.
2022 Dec;24(4):398-403. 10.7461/jcen.2022.E2021.11.003.
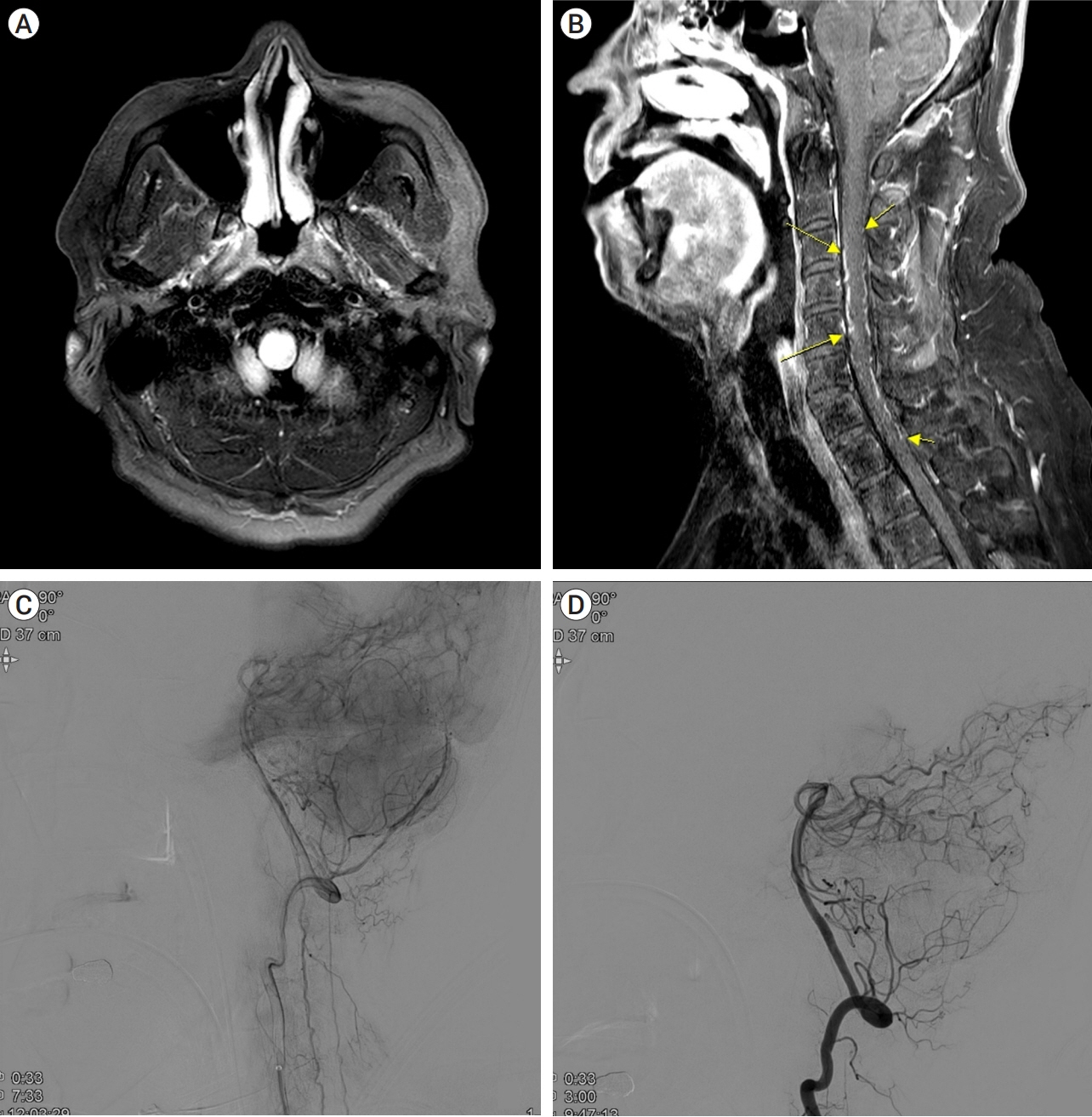
Congestive myelopathy due to spinal dural arteriovenous fistula mimicking CNS demyelinating disease
- Affiliations
-
- 1Department of Neurology, College of Medicine, Hanyang University, Seoul, Korea
- KMID: 2537326
- DOI: http://doi.org/10.7461/jcen.2022.E2021.11.003
Abstract
- Spinal dural arteriovenous fistula (SDAVF) is known for its ambiguous and various clinical presentations. Among these presentations, congestive myelopathy is one of the most common, yet it is challenging to correctly diagnose SDAVF at initial presentation. Several diseases present as myelopathy, including demyelinating diseases. Herein, we present two cases of congestive myelopathy due to SDAVF presenting to the emergency room (ER) with progressive quadriparesis. Even though the patients had a proper magnetic resonance imaging (MRI) examination from the initial presentation, there was a delay in making a final diagnosis. Both patients’ clinical presentation and MRI mimicked central nervous system (CNS) demyelinating disease initially, and a more thorough examination revealed SDAVF. Such a delay in diagnosis can result in more neurological deterioration and may result in more sequelae. Hence, SDAVF should always be considered as a differential diagnosis when examining patients with myelopathy.
Keyword
Figure
Reference
-
1. Fox S, Hnenny L, Ahmed U, Meguro K, Kelly ME. Spinal dural arteriovenous fistula: a case series and review of imaging findings. Spinal Cord Ser Cases. 2017; Jul. 3:17024.
Article2. Howard RS. Spinal vascular disease: a neglected cause of myelopathy. Pract Neurol. 2019; Jun. 19(3):184–6.
Article3. Koch C, Zeumer H, Westphal M. Spinal vascular malformations: therapeutic options. In : Lanzer P, Topol EJ, editors. Pan Vascular Medicine. Berlin, Heidelberg: Springer;2002. p. 1253–64.4. Li C, Yu J, Li K, Hou K, Yu J. Dural arteriovenous fistula of the lateral foramen magnum region: a review. Interv Neuroradiol. 2018; Aug. 24(4):425–34.
Article5. Maimon S, Luckman Y, Strauss I. Spinal dural arteriovenous fistula: a review. Adv Tech Stand Neurosurg. 2016; (43):111–37.
Article6. Rain S, Udding J, Broere D. Acute clinical worsening after steroid administration in cervical myelitis may reveal a subdural arteriovenous fistula. Case Rep Neurol. 2016; Nov. 8(3):234–42.
Article7. Ronald AA, Yao B, Winkelman RD, Piraino D, Masaryk TJ, Krishnaney AA. Spinal dural arteriovenous fistula: diagnosis, outcomes, and prognostic factors. World Neurosurg. 2020; Dec. 144:e306–15.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Myelopathy due to Spinal Dural Arteriovenous Fistula: A Case Report
- Myelopathy Caused by Spinal Dural Arterio-Venous Fistula after First Lumbar Vertebral Body Fracture: A Case Report
- Syringomyelia Associated with Spinal Dural Arteriovenous Fistula: Clinical and Radiological Improvement after Embolization
- Intracranial Dural Arteriovenous Fistula Draining into Spinal Perimedullary Veins: A Rare Cause of Myelopathy
- A Case of Myelopathy due to Spinal Dural Arteriovenous Fistula Supplied by Branches of the Internal Iliac Arteries