J Stroke.
2022 Sep;24(3):404-416. 10.5853/jos.2022.01606.
Outcome Prediction in Cerebral Venous Thrombosis: The IN-REvASC Score
- Affiliations
-
- 1Department of Neurology, Boston Medical Center, Boston University School of Medicine, Boston, MA, USA
- 2Department of Neurology, Brown University, Providence, RI, USA
- 3Department of Neurology, Cooper Neurological Institute, Cooper University Hospital, Camden, NJ, USA
- 4Department of Neurology, University of Colorado School of Medicine, Aurora, CO, USA
- 5Department of Neurology, University of Florida, Gainesville, FL, USA
- 6Department of Neurology, Inselspital, University Hospital Bern, University of Bern, Bern, Switzerland
- 7Department of Neurology, Yale University, New Haven, CT, USA
- 8Department of Neuroradiology, Clinic of Radiology and Nuclear Medicine, University Hospital Basel, Basel, Switzerland
- 9Department of Medicine and Surgery, University of Perugia, Perugia, Italy
- 10Neurology–Stroke Unit, IRCCS MultiMedica, Milano, Italy
- 11Department of Neurology, University of California at Los Angeles, Los Angeles, CA, USA
- 12Department of Neurosciences and Mental Health, Neurology Service, Hospital de Santa Maria/CHULN, University of Lisbon, Lisbon, Portugal
- 13Department of Neurology, Amsterdam University Medical Center, location AMC, Amsterdam, The Netherlands
- KMID: 2534270
- DOI: http://doi.org/10.5853/jos.2022.01606
Abstract
- Background
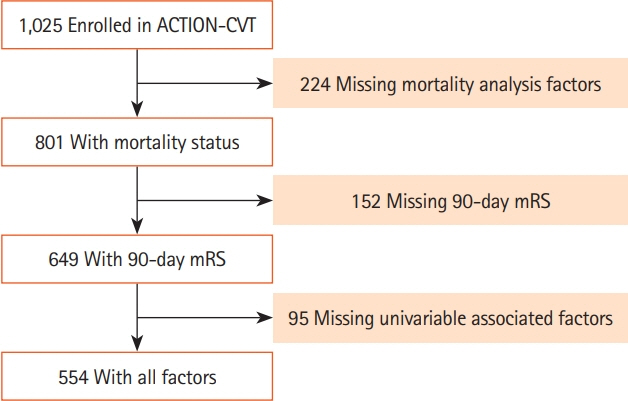
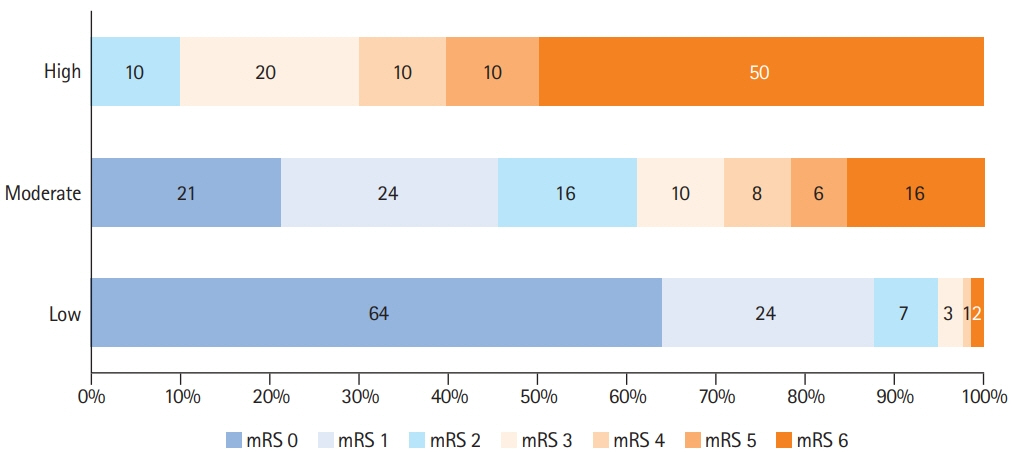
We identified risk factors, derived and validated a prognostic score for poor neurological outcome and death for use in cerebral venous thrombosis (CVT). Methods We performed an international multicenter retrospective study including consecutive patients with CVT from January 2015 to December 2020. Demographic, clinical, and radiographic characteristics were collected. Univariable and multivariable logistic regressions were conducted to determine risk factors for poor outcome, mRS 3-6. A prognostic score was derived and validated. Results A total of 1,025 patients were analyzed with median 375 days (interquartile range [IQR], 180 to 747) of follow-up. The median age was 44 (IQR, 32 to 58) and 62.7% were female. Multivariable analysis revealed the following factors were associated with poor outcome at 90- day follow-up: active cancer (odds ratio [OR], 11.20; 95% confidence interval [CI], 4.62 to 27.14; P<0.001), age (OR, 1.02 per year; 95% CI, 1.00 to 1.04; P=0.039), Black race (OR, 2.17; 95% CI, 1.10 to 4.27; P=0.025), encephalopathy or coma on presentation (OR, 2.71; 95% CI, 1.39 to 5.30; P=0.004), decreased hemoglobin (OR, 1.16 per g/dL; 95% CI, 1.03 to 1.31; P=0.014), higher NIHSS on presentation (OR, 1.07 per point; 95% CI, 1.02 to 1.11; P=0.002), and substance use (OR, 2.34; 95% CI, 1.16 to 4.71; P=0.017). The derived IN-REvASC score outperformed ISCVT-RS for the prediction of poor outcome at 90-day follow-up (area under the curve [AUC], 0.84 [95% CI, 0.79 to 0.87] vs. AUC, 0.71 [95% CI, 0.66 to 0.76], χ2 P<0.001) and mortality (AUC, 0.84 [95% CI, 0.78 to 0.90] vs. AUC, 0.72 [95% CI, 0.66 to 0.79], χ2 P=0.03). Conclusions Seven factors were associated with poor neurological outcome following CVT. The INREvASC score increased prognostic accuracy compared to ISCVT-RS. Determining patients at highest risk of poor outcome in CVT could help in clinical decision making and identify patients for targeted therapy in future clinical trials.
Keyword
Figure
Reference
-
References
1. Devasagayam S, Wyatt B, Leyden J, Kleinig T. Cerebral venous sinus thrombosis incidence is higher than previously thought: a retrospective population-based study. Stroke. 2016; 47:2180–2182.2. Coutinho JM, Zuurbier SM, Aramideh M, Stam J. The incidence of cerebral venous thrombosis: a cross-sectional study. Stroke. 2012; 43:3375–3377.3. Salottolo K, Wagner J, Frei DF, Loy D, Bellon RJ, McCarthy K, et al. Epidemiology, endovascular treatment, and prognosis of cerebral venous thrombosis: US center study of 152 patients. J Am Heart Assoc. 2017; 6:e005480.4. Ropper AH, Klein JP. Cerebral venous thrombosis. N Engl J Med. 2021; 385:59–64.5. Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F; ISCVT Investigators. Prognosis of cerebral vein and dural sinus thrombosis: results of the International Study on Cerebral Vein and Dural Sinus Thrombosis (ISCVT). Stroke. 2004; 35:664–670.6. Borhani Haghighi A, Edgell RC, Cruz-Flores S, Feen E, Piriyawat P, Vora N, et al. Mortality of cerebral venous-sinus thrombosis in a large national sample. Stroke. 2012; 43:262–264.7. Korathanakhun P, Sathirapanya P, Geater SL, Petpichetchian W. Predictors of hospital outcome in patients with cerebral venous thrombosis. J Stroke Cerebrovasc Dis. 2014; 23:2725–2729.8. Duman T, Uluduz D, Midi I, Bektas H, Kablan Y, Goksel BK, et al. A multicenter study of 1144 patients with cerebral venous thrombosis: the VENOST Study. J Stroke Cerebrovasc Dis. 2017; 26:1848–1857.9. Wasay M, Kaul S, Menon B, Dai AI, Saadatnia M, Malik A, et al. Asian study of cerebral venous thrombosis. J Stroke Cerebrovasc Dis. 2019; 28:104247.10. Ferro JM, Bacelar-Nicolau H, Rodrigues T, Bacelar-Nicolau L, Canhão P, Crassard I, et al. Risk score to predict the outcome of patients with cerebral vein and dural sinus thrombosis. Cerebrovasc Dis. 2009; 28:39–44.11. Barboza MA, Chiquete E, Arauz A, Merlos-Benitez M, Quiroz-Compeán A, Barinagarrementería F, et al. A practical score for prediction of outcome after cerebral venous thrombosis. Front Neurol. 2018; 9:882.12. Poungvarin N, Prayoonwiwat N, Ratanakorn D, Towanabut S, Tantirittisak T, Suwanwela N, et al. Thai venous stroke prognostic score: TV-SPSS. J Med Assoc Thai. 2009; 92:1413–1422.13. Koopman K, Uyttenboogaart M, Vroomen PC, van der Meer J, De Keyser J, Luijckx GJ. Development and validation of a predictive outcome score of cerebral venous thrombosis. J Neurol Sci. 2009; 276:66–68.14. Barinagarrementeria F, Cantu C, Arredondo H. Aseptic cerebral venous thrombosis: proposed prognostic scale. J Stroke Cerebrovasc Dis. 1992; 2:34–39.15. Eskey CJ, Meyers PM, Nguyen TN, Ansari SA, Jayaraman M, McDougall CG, et al. Indications for the performance of intracranial endovascular neurointerventional procedures: a scientific statement from the American Heart Association. Circulation. 2018; 137:e661–e689.16. Ferro JM, Coutinho JM, Dentali F, Kobayashi A, Alasheev A, Canhão P, et al. Safety and efficacy of dabigatran etexilate vs dose-adjusted warfarin in patients with cerebral venous thrombosis: a randomized clinical trial. JAMA Neurol. 2019; 76:1457–1465.17. Yaghi S, Shu L, Bakradze E, Salehi Omran S, Giles JA, Amar JY, et al. Direct oral anticoagulants versus warfarin in the treatment of cerebral venous thrombosis (ACTION-CVT): a multicenter international study. Stroke. 2022; 53:728–738.18. Alimohammadi A, Kim DJ, Field TS. Updates in cerebral venous thrombosis. Curr Cardiol Rep. 2022; 24:43–50.19. Shu L, Bakradze E, Salehi Omran S, Giles JA, Amar JY, Henninger N, et al. Predictors of recurrent venous thrombosis after cerebral venous thrombosis: analysis of the ACTION-CVT Study. Neurology. 2022 Forthcoming.20. Siegler JE, Shu L, Yaghi S, Salehi Omran S, Elnazeir M, Bakradze E, et al. Endovascular therapy for cerebral vein thrombosis: a propensity-matched analysis of anticoagulation in the treatment of cerebral venous thrombosis. Neurosurgery. 2022; Aug. 23. [Epub]. https://doi.org/10.1227/neu.0000000000002098.21. Liberman AL, Kamel H, Mullen MT, Messé SR. International Classification of Diseases, ninth revision (ICD-9) diagnosis codes can identify cerebral venous thrombosis in hospitalized adults. Neurohospitalist. 2016; 6:147–150.22. Handley JD, Emsley HC. Validation of ICD-10 codes shows intracranial venous thrombosis incidence to be higher than previously reported. Health Inf Manag. 2020; 49:58–61.23. Burke JF, Freedman VA, Lisabeth LD, Brown DL, Haggins A, Skolarus LE. Racial differences in disability after stroke: results from a nationwide study. Neurology. 2014; 83:390–397.24. Clayton P. CUTPT: Stata module for empirical estimation of cutpoint for a diagnostic test. IDEAS;https://ideas.repec.org/c/boc/bocode/s457719.html. 2013. Accessed August 30, 2022.25. Canhão P, Ferro JM, Lindgren AG, Bousser MG, Stam J, Barinagarrementeria F, et al. Causes and predictors of death in cerebral venous thrombosis. Stroke. 2005; 36:1720–1725.26. Girot M, Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F, et al. Predictors of outcome in patients with cerebral venous thrombosis and intracerebral hemorrhage. Stroke. 2007; 38:337–342.27. Otite FO, Patel S, Sharma R, Khandwala P, Desai D, Latorre JG, et al. Trends in incidence and epidemiologic characteristics of cerebral venous thrombosis in the United States. Neurology. 2020; 95:e2200–e2213.28. Williams O, Ovbiagele B. Stroking out while Black: the complex role of racism. JAMA Neurol. 2020; 77:1343–1344.29. Levine DA, Duncan PW, Nguyen-Huynh MN, Ogedegbe OG. Interventions targeting racial/ethnic disparities in stroke prevention and treatment. Stroke. 2020; 51:3425–3432.30. Churchwell K, Elkind MS, Benjamin RM, Carson AP, Chang EK, Lawrence W, et al. Call to action: structural racism as a fundamental driver of health disparities: a presidential advisory from the American Heart Association. Circulation. 2020; 142:e454–e468.31. Skolarus LE, Sharrief A, Gardener H, Jenkins C, Boden-Albala B. Considerations in addressing social determinants of health to reduce racial/ethnic disparities in stroke outcomes in the United States. Stroke. 2020; 51:3433–3439.32. Magwood GS, Ellis C, Nichols M, Burns SP, Jenkins C, Woodbury M, et al. Barriers and facilitators of stroke recovery: perspectives from African Americans with stroke, caregivers and healthcare professionals. J Stroke Cerebrovasc Dis. 2019; 28:2506–2516.33. Barlas RS, Honney K, Loke YK, McCall SJ, Bettencourt-Silva JH, Clark AB, et al. Impact of hemoglobin levels and anemia on mortality in acute stroke: analysis of UK regional registry data, systematic review, and meta-analysis. J Am Heart Assoc. 2016; 5:e003019.34. Silvis SM, Reinstra E, Hiltunen S, Lindgren E, Heldner MR, Mansour M, et al. Anaemia at admission is associated with poor clinical outcome in cerebral venous thrombosis. Eur J Neurol. 2020; 27:716–722.35. Liu K, Pei L, Gao Y, Zhao L, Fang H, Bunda B, et al. Dehydration status predicts short-term and long-term outcomes in patients with cerebral venous thrombosis. Neurocrit Care. 2019; 30:478–483.36. Coutinho JM, Ferro JM, Canhão P, Barinagarrementeria F, Cantú C, Bousser MG, et al. Cerebral venous and sinus thrombosis in women. Stroke. 2009; 40:2356–2361.37. Ruiz-Sandoval JL, Chiquete E, Bañuelos-Becerra LJ, Torres-Anguiano C, González-Padilla C, Arauz A, et al. Cerebral venous thrombosis in a Mexican multicenter registry of acute cerebrovascular disease: the RENAMEVASC study. J Stroke Cerebrovasc Dis. 2012; 21:395–400.38. Coutinho JM, Zuurbier SM, Bousser MG, Ji X, Canhão P, Roos YB, et al. Effect of endovascular treatment with medical management vs standard care on severe cerebral venous thrombosis: the TO-ACT Randomized Clinical Trial. JAMA Neurol. 2020; 77:966–973.39. Quinn TJ, Dawson J, Walters MR, Lees KR. Reliability of the modified Rankin Scale: a systematic review. Stroke. 2009; 40:3393–3395.40. Dentali F, Poli D, Scoditti U, Di Minno MN, De Stefano V, Siragusa S, et al. Long-term outcomes of patients with cerebral vein thrombosis: a multicenter study. J Thromb Haemost. 2012; 10:1297–1302.41. Nguyen TN, Qureshi MM, Klein P, Yamagami H, Abdalkader M, Mikulik R, et al. Global impact of the COVID-19 pandemic on cerebral venous thrombosis and mortality. J Stroke. 2022; 24:256–265.42. Siegler JE, Abdalkader M, Michel P, Nguyen TN. Therapeutic trends of cerebrovascular disease during the COVID-19 pandemic and future perspectives. J Stroke. 2022; 24:179–188.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Case of Cerebral Venous Thromobosis Associated with Postsplenectomy Thrombocytosis
- A Case of Leptomeningeal Metastasis Associated with Cerebral Venous Thrombosis
- Deep Cerebral Venous Thrombosis Showing Parkinsonism such as Micrographia, Hypophonia and Bradykinesia
- A Case of Deep Cerebral Venous Thrombosis Associated with Iron Deficiency Anemia
- Efficiency of decompressive craniectomy as a line of management of severe cerebral venous thrombosis