J Cerebrovasc Endovasc Neurosurg.
2022 Jun;24(2):129-136. 10.7461/jcen.2022.E2021.07.012.
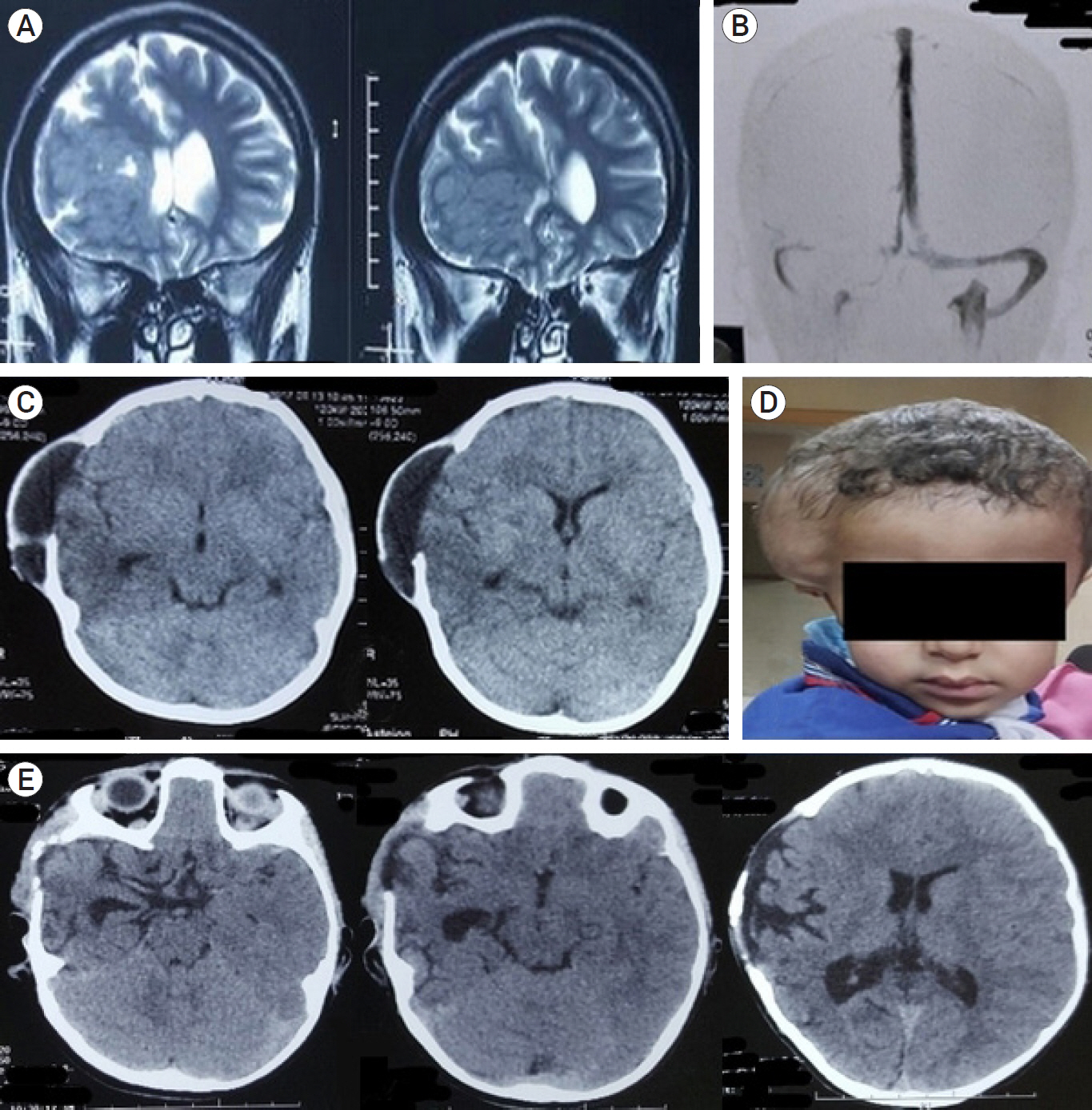
Efficiency of decompressive craniectomy as a line of management of severe cerebral venous thrombosis
- Affiliations
-
- 1Department of Neurosurgery, Mansoura University Hospital, Mansoura University, Mansoura, Egypt
- KMID: 2531655
- DOI: http://doi.org/10.7461/jcen.2022.E2021.07.012
Abstract
Objective
Cerebral venous thrombosis (CVT) is a rare pathology with life threatening consequences, most of these fatal complications are due to raised intracranial pressure due to venous infarction and cerebral swelling, the purpose of this study is to evaluate the efficiency of decompressive craniectomy for favorable outcome.
Methods
A retrospective analysis of clinical, radiological and surgical data of patients who underwent decompressive craniectomy for CVT in a tertiary referral hospital between the years 2016 through 2020.
Results
The study included 7 patients, female predominance was noted (5/7), mean age was 18.14 years. Mean Glasgow coma score (GCS) at surgery was 8.26, good clinical outcome was achieved for the majority of cases 71.4%, and one case of mortality 14.28%.
Conclusions
Decompressive craniectomy is a life saving procedure for patients with severe brain swelling as a sequela of CVT, majority of patients (71.4%) showed favorable functional outcome by 6 months postoperatively.
Figure
Reference
-
1. Aaron S, Alexander M, Maya T, Mathew V, Goel M, Nair SC, et al. Underlying prothrombotic states in pregnancy associated cerebral venous thrombosis. Neurol India. 2010; 58(4):555–9.
Article2. Aaron S, Alexander M, Moorthy RK, Mani S, Mathew V, Patil AKB, et al. Decompressive craniectomy in cerebral venous thrombosis: A single centre experience. J Neurol Neurosurg Psychiatry. 2013; Sep. 84(9):995–1000.
Article3. Breteau G, Mounier-Vehier F, Godefroy O, Gauvrit JY, Mackowiak-Cordoliani MA, Girot M, et al. Cerebral venous thrombosis: 3-year clinical outcome in 55 consecutive patients. J Neurol. 2003; Jan. 250(1):29–35.4. Canhão P, Falcão F, Ferro JM. Thrombolytics for cerebral sinus thrombosis: A systematic review. Cerebrovascular Diseases. 2003; 15(3):159–66.5. Coutinho JM, Majoie CBLM, Coert BA, Stam J. Decompressive hemicraniectomy in cerebral sinus thrombosis: Consecutive case series and review of the literature. Stroke. 2009; Jun. 40(6):2233–5.
Article6. Einhäupl K, Stam J, Bousser MG, De Bruijn SFTM, Ferro JM, Martinelli I, et al. EFNS guideline on the treatment of cerebral venous and sinus thrombosis in adult patients. Eur J Neurol. 2010; Oct. 17(10):1229–35.
Article7. Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F. Prognosis of cerebral vein and dural sinus thrombosis: Results of the international study on cerebral vein and dural sinus thrombosis (ISCVT). Stroke. 2004; Mar. 35(3):664–70.
Article8. Ferro JM, Crassard I, Coutinho JM, Canhão P, Barinagarrementeria F, Cucchiara B, et al. Decompressive surgery in cerebrovenous thrombosis: A multicenter registry and a systematic review of individual patient data. Stroke. 2011; Oct. 42(10):2825–31.9. Girot M, Ferro JM, Canhão P, Stam J, Bousser MG, Barinagarrementeria F, et al. Predictors of outcome in patients with cerebral venous thrombosis and intracerebral hemorrhage. Stroke. 2007; Feb. 38(2):337–42.
Article10. Hiltunen S, Putaala J, Haapaniemi E, Tatlisumak T. Long-term outcome after cerebral venous thrombosis: Analysis of functional and vocational outcome, residual symptoms, and adverse events in 161 patients. J Neurol. 2016; Mar. 263(3):477–84.
Article11. Ilyas A, Chen CJ, Raper DM, Ding D, Buell T, Mastorakos P, et al. Endovascular mechanical thrombectomy for cerebral venous sinus thrombosis: A systematic review. J Neurointerv Surg. 2017; Nov. 9(11):1086–92.
Article12. Keller E, Pangalu A, Fandino J, Könü D, Yonekawa Y. Decompressive craniectomy in severe cerebral venous and dural sinus thrombosis. Acta Neurochir Suppl. 2005; 94:177–83.
Article13. Lee SS, Baek SH, Shin DI. A case of cerebral venous thrombosis as the presenting sign of occult prostate cancer. J Clin Neurol. 2009; Dec. 5(4):195–7.
Article14. Mohamed MWF, Aung SS, Mereddy N, Ramanan SP, Hamid P. Role, effectiveness, and outcome of decompressive craniectomy for cerebral venous and dural sinus thrombosis (CVST): Is surgery really an option? Cureus. 2020; Dec. 17. 12(12):e12135.
Article15. Raza E, Shamim MS, Wadiwala MF, Ahmed B, Kamal AK. Decompressive surgery for malignant cerebral venous sinus thrombosis: A retrospective case series from pakistan and comparative literature review. J Stroke Cerebrovasc Dis. 2014; Jan. 23(1):e13–22.
Article16. Saposnik G, Barinagarrementeria F, Brown RD, Bushnell CD, Cucchiara B, Cushman M, et al. Diagnosis and management of cerebral venous thrombosis: A statement for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2011; Apr. 42(4):1158–92.
Article17. Shariff EM, Alhameed M. Multiple cranial neuropathies in cerebral venous sinus thrombosis. Oxf Med Case Reports. 2014; May. 2014(2):21–3.
Article18. Théaudin M, Crassard I, Bresson D, Saliou G, Favrole P, Vahedi K, et al. Should decompressive surgery be performed in malignant cerebral venous thrombosis?: A series of 12 patients. Stroke. 2010; Apr. 41(4):727–31.19. Vahedi K, Hofmeijer J, Juettler E, Vicaut E, George B, Algra A, et al. Early decompressive surgery in malignant infarction of the middle cerebral artery: A pooled analysis of three randomised controlled trials. Lancet Neurol. 2007; 6(3):215–22.
Article20. Weber J, Spring A. Unilateral decompressive craniectomy in left transverse and sigmoid sinus thrombosis. Zentralbl Neurochir. 2004; 65(3):135–40.
Article21. Zhang S, Zhao H, Li H, You C, Hui X. Decompressive craniectomy in hemorrhagic cerebral venous thrombosis: Clinicoradiological features and risk factors. J Neurosurg. 2017; Oct. 127(4):709–15.
Article22. Zhao X, Rizzo A, Malek B, Fakhry S, Watson J. Basilar skull fracture: A risk factor for transverse/sigmoid venous sinus obstruction. J Neurotrauma. 2008; Feb. 25(2):104–11.
Article23. Zuurbier SM, Coutinho JM, Majoie CBLM, Coert BA, van den Munckhof P, Stam J. Decompressive hemicraniectomy in severe cerebral venous thrombosis: A prospective case series. J Neurol. 2012; Jun. 259(6):1099–105.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Unilateral Thrombosis of a Deep Cerebral Vein Associated with Transient Unilateral Thalamic Edema
- Paradoxical Herniation after Decompressive Craniectomy for Acute Subdural Hematoma
- Efficacy of the Decompressive Craniectomy for Acute Cerebral Infarction: Timing of Surgical Intervention and Clinical Prognostic Factors
- Clinical Comparison between Simple Craniectomy and Lesionectomy in the Patients with Acute Cerebral Infarction
- A Case of Hemorrhagic Cerebral Infarction in Ulcerative Colitis