Ann Pediatr Endocrinol Metab.
2022 Sep;27(3):183-191. 10.6065/apem.2244116.058.
Change of obesity prevalence and lifestyle patterns before and during COVID-19 among Korean adolescents
- Affiliations
-
- 1Department of Pediatrics, Gyeongsang National University Changwon Hospital, Changwon, Korea
- 2Department of Pediatrics, Korea Cancer Center Hospital, Seoul, Korea
- KMID: 2533337
- DOI: http://doi.org/10.6065/apem.2244116.058
Abstract
- Purpose
Lockdown measure for limiting coronavirus disease 2019 (COVID-19) spread cause an aggravation of the childhood obesity epidemic through lifestyle changes. The aim is to investigate how social restriction might have changed obesity prevalence and lifestyle patterns in Korean adolescents. We also evaluate the most fragile group and most influencing lifestyle parameters on obesity prevalence.
Methods
To assess the change in weight status and lifestyle, we compared the Korea Youth Risk Behavior Web-based Survey data 2019 (pre-COVID-19, n=57,303) and 2020 (post-COVID-19, n=54,948). Participants from middle schools and high schools, aged 12 to 18 years, voluntarily reported their weight status and lifestyles.
Results
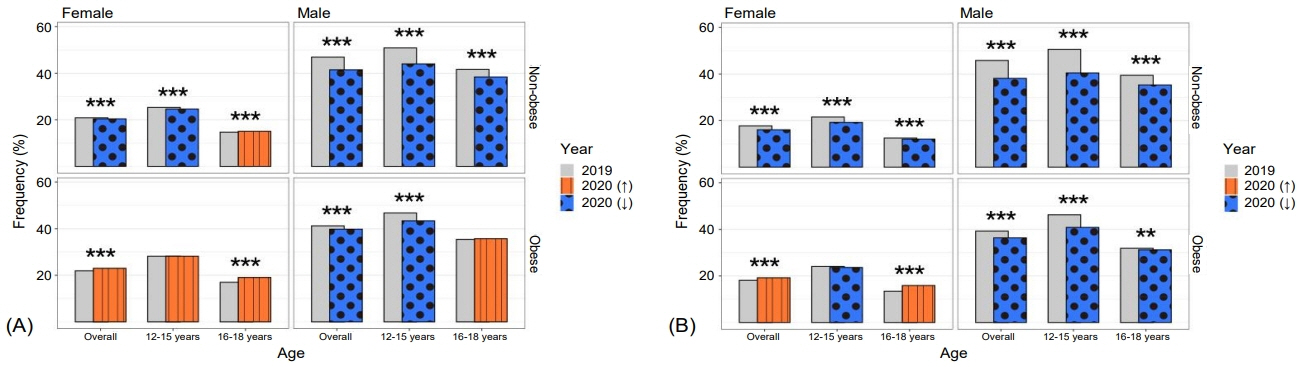
The prevalence of obesity of the total subjects was 11.0% in 2019 and 12.1% in 2020. This prevalence difference varied by sex (males 1.8%, females 0.3%, p<0.001), age group (12–15 year 1.6%, 16–18 year 0.4%, p<0.001), and socioeconomic status. Male aged 12–15 years showed highest increase from 12.5% to 15.2%. Physical activities, fruit intake, consumption of sugar-sweetened beverages, and stress showed all decrease. Only, nonstudy sedentary time marked increased from 3.3±2.3 hr/day to 4.3±2.8 hr/day. Both moderate-intensity and vigorous-intensity physical activity marked decreased especially in male aged 12–15 years, while increased in female aged 16–18 years.
Conclusion
Korean adolescents showed increasing obesity prevalence after COVID-19 lockdown, with males aged 12–15 years mainly affected, mainly due to a reduced physical activity and increased sedentary time.
Keyword
Figure
Cited by 3 articles
-
Correlation of tri-ponderal mass index with insulin-like growth factor-I and insulin-like growth factor binding protein-3 in children and adolescents
Iee Ho Choi, Sun-Young Kim, Minsun Kim
Ann Pediatr Endocrinol Metab. 2024;29(4):258-265. doi: 10.6065/apem.2346158.079.Impact of COVID-19 lockdown on blood glucose levels in pediatric patients with type 1 diabetes mellitus
Min Hyung Cho, Young Suk Shim, Hae Sang Lee
Ann Pediatr Endocrinol Metab. 2025;30(1):25-30. doi: 10.6065/apem.2448072.036.Clinical and epidemiological insights into early puberty in Thai girls: a 5-year study
Phattariya Yaisilp, Nattakarn Numsriskulrat, Taninee Sahakitrungruang
Ann Pediatr Endocrinol Metab. 2025;30(1):17-24. doi: 10.6065/apem.2448112.056.
Reference
-
References
1. Ng M, Fleming T, Robinson M, Thomson B, Graetz N, Margono C, et al. Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet. 2014; 384:766–81.2. Must A, Jacques PF, Dallal GE, Bajema CJ, Dietz WH. Longterm morbidity and mortality of overweight adolescents: a follow-up of the Harvard Growth Study of 1922 to 1935. N Engl J Med. 1992; 327:1350–5.3. Videira-Silva A, Freira S, Fonseca H. Metabolically healthy overweight adolescents: definition and components. Ann Pediatr Endocrinol Metab. 2020; 25:256–64.4. National Center for Health Statistics (U.S.). Prevalence of overweight, obesity, and severe obesity among children and adolescents aged 2–19 years: United States, 1963–1965 through 2015–2016 [Internet]. Atlanta (GA): Centers for Disease Control and Prevention;2018. [updated 2019 Sept; cited 2022 May 7]. Available from: https://stacks.cdc.gov/view/cdc/58669/.5. Abarca-G’omez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 populationbased measurement studies in 128textperiodcentered 9 million children, adolescents, and adults. Lancet. 2017; 390:2627–42.6. Seo MY, Kim SH, Park MJ. Changes in anthropometric indices among Korean school students based on the 2010 and 2018 Korea School Health Examination Surveys. Ann Pediatr Endocrinol Metab. 2021; 26:38–45.7. Pietrobelli A, Pecoraro L, Ferruzzi A, Heo M, Faith M, Zoller T, et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity (Silver Spring). 2020; 28:1382–5.8. Dunton GF, Do B, Wang SD. Early effects of the COVID-19 pandemic on physical activity and sedentary behavior in children living in the US. BMC Public Health. 2020; 20:1351.9. Xiang M, Zhang Z, Kuwahara K. Impact of COVID-19 pandemic on children and adolescents’lifestyle behavior larger than expected. Prog Cardiovasc Dis. 2020; 63:531–2.10. Korea Disease Control and Prevention Agency. COVID-19 response [Internet]. Sejong (Korea): Ministry of Health and Welfare;2022. [cited 2022 May 7]. Available from: http://ncov.mohw.go.kr/en/baroView.do?brdId=11&brdGubun=111&dataGubun=&ncvContSeq=&contSeq=&board_id=&gubun=.11. Han JA, Chung YE, Chung IH, Hong YH, Chung S. Impact of the COVID-19 pandemic on seasonal variations in childhood and adolescent growth: experience of pediatric endocrine clinics. Children (Basel). 2021; 8:404.12. Gwag SH, Oh YR, Ha JW, Kang E, Nam HK, Lee Y, et al. Weight changes of children in 1 year during COVID-19 pandemic. J Pediatr Endocrinol Metab. 2022; 35:297–302.13. Vogel M, Geserick M, Gausche R, Beger C, Poulain T, Meigen C, et al. Age-and weight group-specific weight gain patterns in children and adolescents during the 15 years before and during the COVID-19 pandemic. Int J Obes (Lond). 2022; 46:144–52.14. Wen J, Zhu L, Ji C. Changes in weight and height among Chinese preschool children during COVID-19 school closures. Int J Obes (Lond). 2021; 45:2269–73.15. Brazendale K, Garcia J, Hunt ET, Blankenship M, Eisenstein D, Leon A. Preliminary evidence of children’s weight gain from 5 months of home quarantine during the COVID-19 pandemic. Am J Lifestyle Med. 2021; 16:197–202.16. Korea Disease Control and Prevention Agency. Korea youth risk behavior survey [Internet]. Cheongju (Korea): Korea Disease Control and Prevention Agency;2022. [cited 2021 Apr 15]. Available from: https://www.kdca.go.kr/yhs/.17. Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, et al. The 2017 Korean national growth charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 2018; 61:135–49.18. Bae JS, Joung HJ, Kim JY, Kwon KN, Kim YJ, Park SW. Validity of self-reported height, weight, and body mass index of the Korea Youth Risk Behavior Web-based Survey questionnaire. J Prev Med Public Health. 2010; 43:396–402.19. Wu AJ, Aris IM, Hivert MF, Rocchio C, Cocoros NM, Klompas M, et al. Association of changes in obesity prevalence with the COVID-19 pandemic in youth in Massachusetts. JAMA Pediatr. 2022; 176:198–201.20. Jia P, Zhang L, Yu W, Yu B, Liu M, Zhang D, et al. Impact of COVID-19 lockdown on activity patterns and weight status among youths in China: the COVID-19 Impact on Lifestyle Change Survey (COINLICS). Int J Obes (Lond). 2021; 45:695–9.21. Maltoni G, Zioutas M, Deiana G, Biserni GB, Pession A, Zucchini S. Gender differences in weight gain during lockdown due to COVID-19 pandemic in adolescents with obesity. Nutr Metab Cardiovasc Dis. 2021; 31:2181–5.22. Qiu N, He H, Qiao L, Ding Y, Ji S, Guo X, et al. Sex differences in changes in BMI and blood pressure in Chinese school-aged children during the COVID-19 quarantine. Int J Obes (Lond). 2021; 45:2132–6.23. Lim JS, Hwang JS, Cheon GJ, Lee JA, Kim DH, Park KD, et al. Gender differences in total and regional body composition changes as measured by dual-energy x-ray absorptiometry in Korean children and adolescents. J Clin Densitom. 2009; 12:229–37.24. Ahn JH, Lim SW, Song BS, Seo J, Lee JA, Kim DH, et al. Age at menarche in the Korean female: secular trends and relationship to adulthood body mass index. Ann Pediatr Endocrinol Metab. 2013; 18:60–4.25. Amaro-Gahete FJ, Jurado-Fasoli L, De-la-O A, Gutierrez A, Castillo MJ, Ruiz JR. Accuracy and validity of resting energy expenditure predictive equations in middle-aged adults. Nutrients. 2018; 10:1635.26. Rocha J, Paxman J, Dalton C, Winter E, Broom DR. Effects of a 12-week aerobic exercise intervention on eating behaviour, food cravings, and 7-day energy intake and energy expenditure in inactive men. Appl Physiol Nutr Metab. 2016; 41:1129–36.27. Kim J, Lee J. Role of obesity-induced inflammation in the development of insulin resistance and type 2 diabetes: History of the research and remaining questions. Ann Pediatr Endocrinol Metab. 2021; 26:1–13.28. Steinbeck KS. The importance of physical activity in the prevention of overweight and obesity in childhood: a review and an opinion. Obes Rev. 2001; 2:117–30.29. Adams EL, Caccavale LJ, Smith D, Bean MK. Food insecurity, the home food environment, and parent feeding practices in the era of COVID-19. Obesity. 2020; 28:2056–63.30. L'opez-Bueno R, L’opez-S’anchez GF, Casaj’us JA, Calatayud J, Gil-Salmer’on A, Grabovac I, et al. Health-related behaviors among school-aged children and adolescents during the Spanish Covid-19 confinement. Front Pediatr. 2020; 8:573.31. Moore SA, Faulkner G, Rhodes RE, Brussoni M, Chulak-Bozzer T, Ferguson LJ, et al. Impact of the COVID-19 virus outbreak on movement and play behaviours of Canadian children and youth: a national survey. Int J Behav Nutr Phys Act. 2020; 17:85.32. Ruiz-Roso MB, de Carvalho Padilha P, Mantilla-Escalante DC, Ulloa N, Brun P, Acevedo-Correa D, et al. Covid-19 confinement and changes of adolescent’s dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients. 2020; 12:1807.33. Sobal J, Stunkard A. Socioeconomic status and obesity: a review of the literature. Psychol Bull. 1989; 105:260–75.34. Grant-Guimaraes J, Feinstein R, Laber E, Kosoy J. Childhood overweight and obesity. Gastroenterol Clin N Am. 2016; 45:715–28.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Changes in lifestyle and obesity during the COVID-19 pandemic in Korean adolescents: based on the Korea Youth Risk Behavior Survey 2019 and 2020
- A Comparison of Changes in Health Behavior, Obesity, and Mental Health of Korean Adolescents Before and During the COVID-19 Pandemic: Online Cross-Sectional Study
- The impacts of COVID-19 on childhood obesity: prevalence, contributing factors, and implications for management
- Changes in the Prevalences of Obesity, Abdominal Obesity, and Non-Alcoholic Fatty Liver Disease among Korean Children during the COVID-19 Outbreak
- Diabetes, Obesity, and COVID-19