Ann Pediatr Endocrinol Metab.
2022 Dec;27(4):281-288. 10.6065/apem.2142228.114.
Changes in lifestyle and obesity during the COVID-19 pandemic in Korean adolescents: based on the Korea Youth Risk Behavior Survey 2019 and 2020
- Affiliations
-
- 1Department of Pediatrics, Inje University Sanggye Paik Hospital, Seoul, Korea
- 2Department of Pediatrics, Uijeongbu Eulji Medical Center, Eulji University School of Medicine, Uijeongbu, Korea
- KMID: 2537240
- DOI: http://doi.org/10.6065/apem.2142228.114
Abstract
- Purpose
The coronavirus disease 2019 (COVID-19) pandemic has affected people's daily lives and increased their time spent at home. This study aims to investigate the changes in lifestyle factors and obesity among Korean adolescents before and during the COVID-19 outbreak.
Methods
We used the data of 109,282 adolescents aged 12–18 years, from the Korea Youth Risk Behavior Survey conducted in 2019 and 2020 before and during the COVID-19 pandemic, respectively. The changes in the prevalence of obesity and lifestyle factors (diet, exercise, sitting time, and sleep duration) were assessed. The adjusted odds ratios (ORs) (95% confidence intervals [CIs]) of predictors for obesity were calculated.
Results
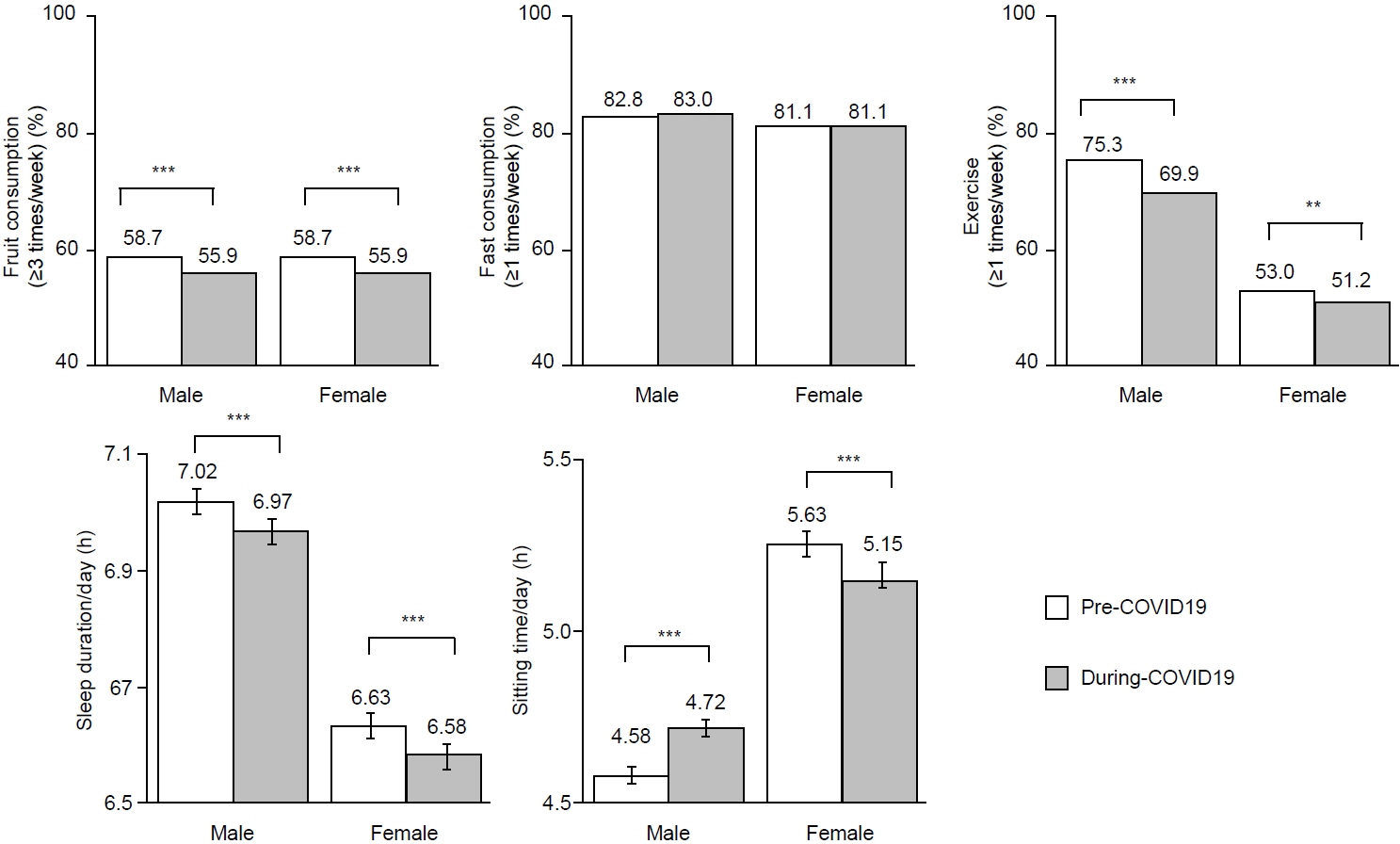
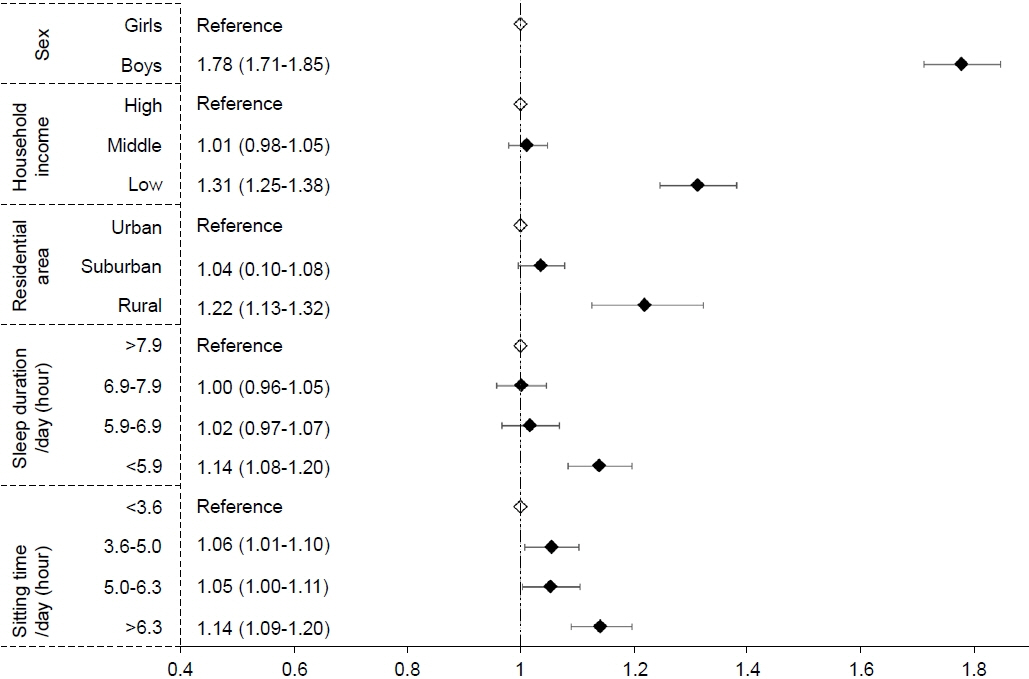
The prevalence of overweight (10% to 10.5%) and obesity (11.5% to 12.7%) increased significantly, especially among males younger than 15 years, whereas significant differences were absent among females. The mean body mass index z-score increased from 0.28 to 0.39 in males but decreased from 0.08 to 0.04 in females. Fruit consumption, regular exercise, and average sleep duration decreased, whereas sitting time increased. After controlling for covariates, a short sleep duration (OR, 1.14) and an increased sitting time (OR, 1.14) were significantly associated with an elevated risk for overweight/obesity.
Conclusion
During the COVID-19 pandemic, the prevalence of obesity and overweight increased, particularly in males, as did unfavorable trends in related lifestyle factors. Sex- and age-specific strategies to improve lifestyle factors associated with obesity are needed, especially during the COVID-19 pandemic.
Keyword
Figure
Reference
-
References
1. Moreno JP, Johnston CA, Woehler D. Changes in weight over the school year and summer vacation: results of a 5-year longitudinal study. J Sch Health. 2013; 83:473–7.2. von Hippel PT, Powell B, Downey DB, Rowland NJ. The effect of school on overweight in childhood: gain in body mass index during the school year and during summer vacation. Am J Public Health. 2007; 97:696–702.3. Androutsos O, Perperidi M, Georgiou C, Chouliaras G. Lifestyle changes and determinants of children's and adolescents' body weight increase during the first COVID-19 lockdown in Greece: The COV-EAT Study. Nutrients. 2021; 13:930.4. Bates LC, Zieff G, Stanford K, Moore JB, Kerr ZY, Hanson ED, et al. COVID-19 impact on behaviors across the 24-hour day in children and adolescents: physical activity, sedentary behavior, and sleep. Children (Basel). 2020; 7:138.5. Beck AL, Huang JC, Lendzion L, Fernandez A, Martinez S. Impact of the coronavirus disease 2019 pandemic on parents' perception of health behaviors in children with overweight and obesity. Acad Pediatr. 2021; 21:1434–40.6. Guo YF, Liao MQ, Cai WL, Yu XX, Li SN, Ke XY, et al. Physical activity, screen exposure and sleep among students during the pandemic of COVID-19. Sci Rep. 2021; 11:8529.7. Koletzko B, Holzapfel C, Schneider U, Hauner H. Lifestyle and body weight consequences of the COVID-19 pandemic in children: increasing disparity. Ann Nutr Metab. 2021; 77:1–3.8. Maltoni G, Zioutas M, Deiana G, Biserni GB, Pession A, Zucchini S. Gender differences in weight gain during lockdown due to COVID-19 pandemic in adolescents with obesity. Nutr Metab Cardiovasc Dis. 2021; 31:2181–5.9. Medrano M, Cadenas-Sanchez C, Oses M, Arenaza L, Amasene M, Labayen I. Changes in lifestyle behaviours during the COVID-19 confinement in Spanish children: a longitudinal analysis from the MUGI project. Pediatr Obes. 2021; 16:e12731.10. Pietrobelli A, Pecoraro L, Ferruzzi A, Heo M, Faith M, Zoller T, et al. Effects of COVID-19 lockdown on lifestyle behaviors in children with obesity living in Verona, Italy: a longitudinal study. Obesity (Silver Spring). 2020; 28:1382–5.11. Ruíz-Roso MB, de Carvalho Padilha P, Matilla-Escalante DC, Brun P, Ulloa N, Acevedo-Correa D, et al. Changes of physical activity and ultra-processed food consumption in adolescents from different countries during Covid-19 pandemic: an observational study. Nutrients. 2020; 12:2289.12. Ventura PS, Ortigoza AF, Castillo Y, Bosch Z, Casals S, Girbau C, et al. Children's health habits and COVID-19 lockdown in Catalonia: implications for obesity and noncommunicable diseases. Nutrients. 2021; 13:1657.13. Yang S, Guo B, Ao L, Yang C, Zhang L, Zhou J, et al. Obesity and activity patterns before and during COVID-19 lockdown among youths in China. Clin Obes. 2020; 10:e12416.14. Zhou J, Xie X, Guo B, Pei R, Pei X, Yang S, et al. Impact of COVID-19 lockdown on physical activity among the Chinese youths: the COVID-19 Impact on Lifestyle Change Survey (COINLICS). Front Public Health. 2021; 9:592795.15. Hoffman JA, Miller EA. Addressing the consequences of school closure due to COVID-19 on children's physical and mental well-being. World Med Health Policy. 2020; 12:300–10.16. Adams EL, Caccavale LJ, Smith D, Bean MK. Food insecurity, the home food environment, and parent feeding practices in the era of COVID-19. Obesity (Silver Spring). 2020; 28:2056–63.17. An R. Projecting the impact of the coronavirus disease-2019 pandemic on childhood obesity in the United States: a microsimulation model. J Sport Health Sci. 2020; 9:302–12.18. Jenssen BP, Kelly MK, Powell M, Bouchelle Z, Mayne SL, Fiks AG. COVID-19 and changes in child obesity. Pediatrics. 2021; 147:e2021050123.19. Kang HM, Jeong DC, Suh BK, Ahn MB. The impact of the coronavirus disease-2019 pandemic on childhood obesity and vitamin D status. J Korean Med Sci. 2021; 36:e21.20. Kim ES, Kwon Y, Choe YH, Kim MJ. COVID-19-related school closing aggravate obesity and glucose intolerance in pediatric patients with obesity. Sci Rep. 2021; 11:5494.21. Ruiz-Roso MB, de Carvalho Padilha P, Mantilla-Escalante DC, Ulloa N, Brun P, Acevedo-Correa D, et al. Covid-19 confinement and changes of adolescent's dietary trends in Italy, Spain, Chile, Colombia and Brazil. Nutrients. 2020; 12:1807.22. UNESCO. COVID-19 educational disruption and response [Internet]. Paris: UNESCO;2021. [cited 2021 Sep 8]. Available from: https://www.unesco.org/en/articles/covid-19-educational-disruption-and-response.23. Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, et al. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 2018; 61:135–49.24. Pietiläinen KH, Kaprio J, Borg P, Plasqui G, Yki-Järvinen H, Kujala UM, et al. Physical inactivity and obesity: a vicious circle. Obesity (Silver Spring). 2008; 16:409–14.25. Kaditis AG, Ohler A, Gileles-Hillel A, Choshen-Hillel S, Gozal D, Bruni O, et al. Effects of the COVID-19 lockdown on sleep duration in children and adolescents: a survey across different continents. Pediatr Pulmonol. 2021; 56:2265–73.26. Patel SR, Hu FB. Short sleep duration and weight gain: a systematic review. Obesity (Silver Spring). 2008; 16:643–53.27. Felső R, Lohner S, Hollódy K, Erhardt É, Molnár D. Relationship between sleep duration and childhood obesity: Systematic review including the potential underlying mechanisms. Nutr Metab Cardiovasc Dis. 2017; 27:751–61.28. Yu B, Zhang D, Yu W, Luo M, Yang S, Jia P. Impacts of lockdown on dietary patterns among youths in China: the COVID-19 impact on lifestyle change survey. Public Health Nutr. 2021; 24:3221–32.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A Comparison of Changes in Health Behavior, Obesity, and Mental Health of Korean Adolescents Before and During the COVID-19 Pandemic: Online Cross-Sectional Study
- Impact of the COVID-19 Pandemic on Tooth Brushing and Handwashing of Adolescents: A Secondary Analayis of the Korea Youth Risk Behavior Web-Based Survey (2019∼2020)
- Changes in health behaviors and obesity of Korean adolescents before and during the COVID-19 pandemic: a special report using the Korea Youth Risk Behavior Survey
- Changes in mental health of Korean adolescents before and during the COVID-19 pandemic: a special report using the Korea Youth Risk Behavior Survey
- Mental Health Changes in Korean Adolescents After the COVID-19 Pandemic: Using the Korea Youth Risk Behavior Survey (KYRBS) From 2020, 2021