Improvement in Age at Mortality and Changes in Causes of Death in the Population with Diabetes: An Analysis of Data from the Korean National Health Insurance and Statistical Information Service, 2006 to 2018
- Affiliations
-
- 1Division of Endocrinology, Department of Internal Medicine, Keimyung University School of Medicine, Daegu, Korea
- 2Divison of Endocrinology, Department of Internal Medicine, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 3Research and Analysis Team, National Health Insurance Service Ilsan Hospital, Goyang, Korea
- 4Department of Public Health, Graduate School, Yonsei University, Seoul, Korea
- 5Division of Endocrinology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- KMID: 2531390
- DOI: http://doi.org/10.3803/EnM.2022.1440
Abstract
- Background
Diabetes is a leading cause of death that is responsible for 1.6 million annual deaths worldwide. However, the life expectancy and age at death of people with diabetes have been a matter of debate.
Methods
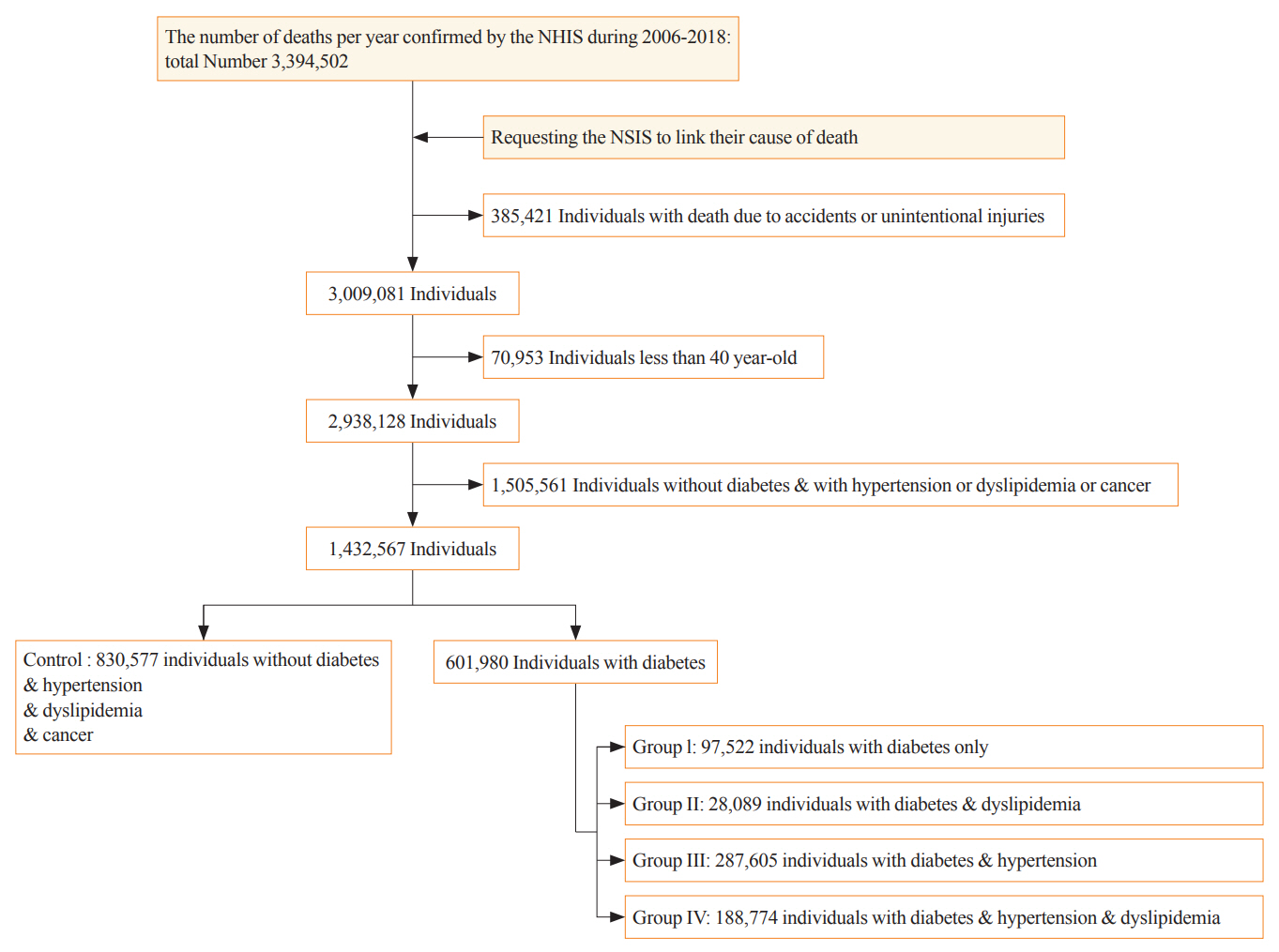
The National Health Insurance Service claims database, merged with death records from the National Statistical Information Service in Korea from 2006 to 2018, was analyzed.
Results
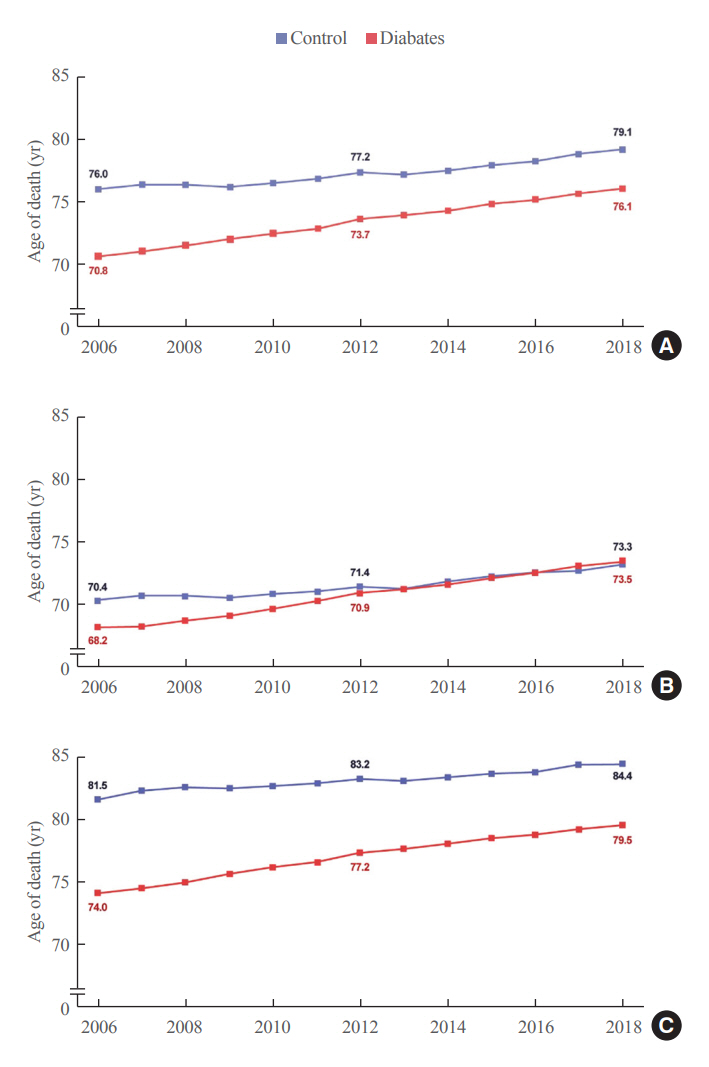
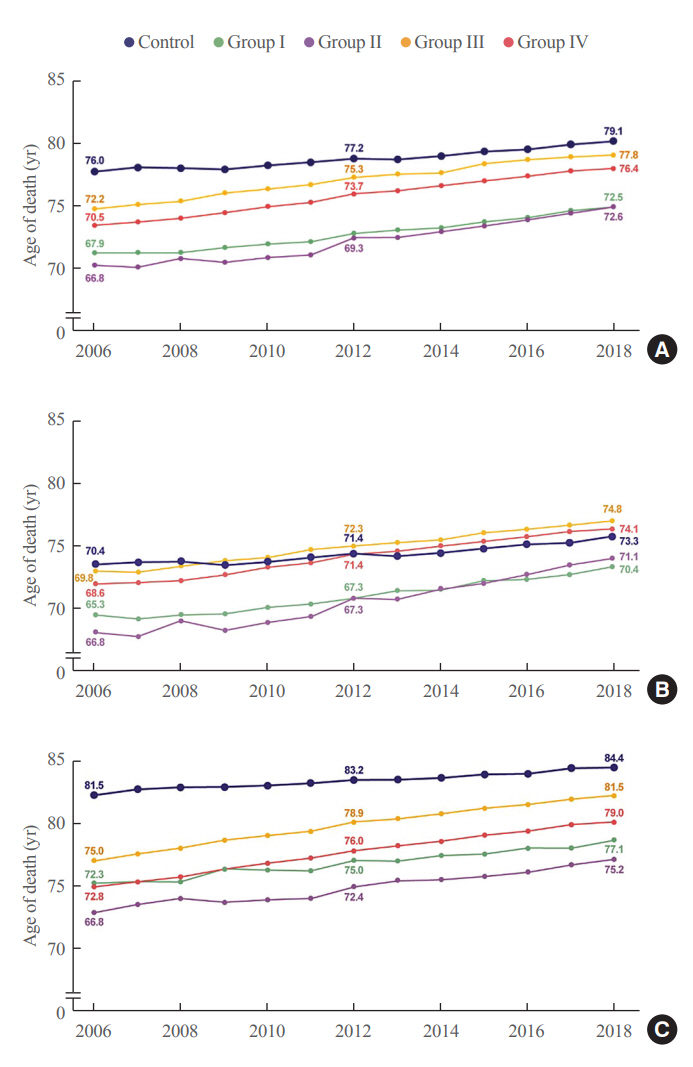
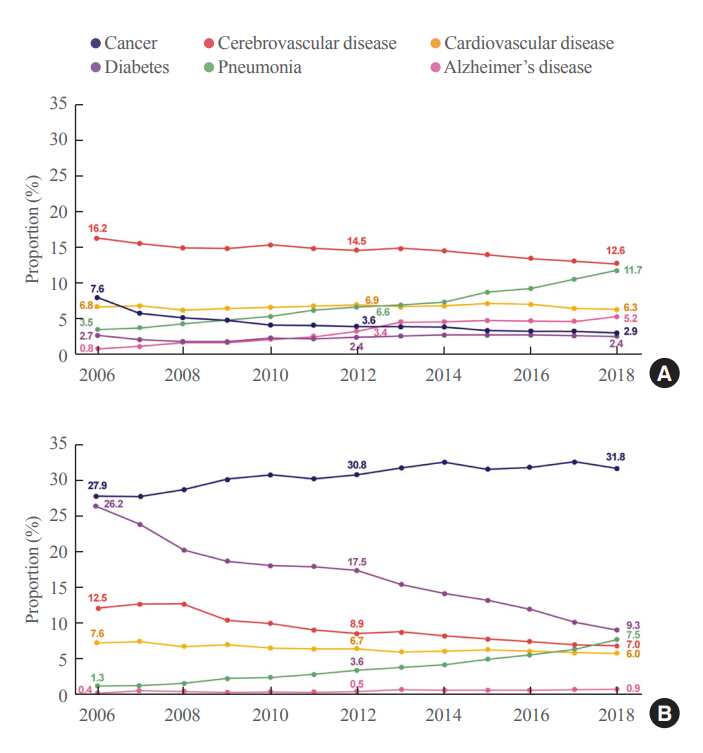
In total, 1,432,567 deaths were collected. The overall age at death increased by 0.44 and 0.26 year/year in the diabetes and control populations, respectively. The disparity in the mean age at death between the diabetes and control populations narrowed from 5.2 years in 2006 to 3.0 years in 2018 (p<0.001). In a subgroup analysis according to the presence of comorbid diseases, the number and proportion of deaths remained steady in the group with diabetes only, but steadily increased in the groups with diabetes combined with dyslipidemia and/or hypertension. Compared to the control population, the increase in the mean death age was higher in the population with diabetes. This trend was more prominent in the groups with dyslipidemia and/or hypertension than in the diabetes only group. Deaths from vascular disease and diabetes decreased, whereas deaths from cancer and pneumonia increased. The decline in the proportion of deaths from vascular disease was greater in the diabetes groups with hypertension and/or dyslipidemia than in the control population.
Conclusion
The age at death in the population with diabetes increased more steeply and reached a comparable level to those without diabetes.
Figure
Cited by 3 articles
-
Risk of Cause-Specific Mortality across Glucose Spectrum in Elderly People: A Nationwide Population-Based Cohort Study
Joonyub Lee, Hun-Sung Kim, Kee-Ho Song, Soon Jib Yoo, Kyungdo Han, Seung-Hwan Lee
Endocrinol Metab. 2023;38(5):525-537. doi: 10.3803/EnM.2023.1765.Long-Term Cumulative Exposure to High γ-Glutamyl Transferase Levels and the Risk of Cardiovascular Disease: A Nationwide Population-Based Cohort Study
Han-Sang Baek, Bongseong Kim, Seung-Hwan Lee, Dong-Jun Lim, Hyuk-Sang Kwon, Sang-Ah Chang, Kyungdo Han, Jae-Seung Yun
Endocrinol Metab. 2023;38(6):770-781. doi: 10.3803/EnM.2023.1726.Effects of Pancreatitis and Type 2 Diabetes Mellitus on the Development of Pancreatic Cancer: A Nationwide Nested Case-Control Study
Young-eun Kim, Min Heui Yu, Chung Mo Nam, Eun Seok Kang
Diabetes Metab J. 2025;49(2):252-263. doi: 10.4093/dmj.2024.0277.
Reference
-
1. NCD Risk Factor Collaboration (NCD-RisC). Worldwide trends in diabetes since 1980: a pooled analysis of 751 population-based studies with 4.4 million participants. Lancet. 2016; 387:1513–30.2. Kim BY, Won JC, Lee JH, Kim HS, Park JH, Ha KH, et al. Diabetes fact sheets in Korea, 2018: an appraisal of current status. Diabetes Metab J. 2019; 43:487–94.
Article3. World Health Organization. Global report on diabetes. Geneva: WHO;2016. [cited 2022 Jun 9]. Available from: https://www.who.int/publications/i/item/9789241565257.4. Kochanek KD, Murphy SL, Xu J, Arias E. Deaths: final data for 2017. Natl Vital Stat Rep. 2019; 68:1–77.5. Tamayo T, Rosenbauer J, Wild SH, Spijkerman AM, Baan C, Forouhi NG, et al. Diabetes in Europe: an update. Diabetes Res Clin Pract. 2014; 103:206–17.
Article6. Vital Statistics Division-Statistics Korea, Shin HY, Kim J, Lee S, Park MS, Park S, et al. Cause-of-death statistics in 2018 in the Republic of Korea. J Korean Med Assoc. 2020; 63:286–97.
Article7. Gregg EW, Li Y, Wang J, Burrows NR, Ali MK, Rolka D, et al. Changes in diabetes-related complications in the United States, 1990-2010. N Engl J Med. 2014; 370:1514–23.
Article8. Wiviott SD, Raz I, Bonaca MP, Mosenzon O, Kato ET, Cahn A, et al. Dapagliflozin and cardiovascular outcomes in type 2 diabetes. N Engl J Med. 2019; 380:347–57.
Article9. Kristensen SL, Rorth R, Jhund PS, Docherty KF, Sattar N, Preiss D, et al. Cardiovascular, mortality, and kidney outcomes with GLP-1 receptor agonists in patients with type 2 diabetes: a systematic review and meta-analysis of cardiovascular outcome trials. Lancet Diabetes Endocrinol. 2019; 7:776–85.
Article10. Zinman B, Wanner C, Lachin JM, Fitchett D, Bluhmki E, Hantel S, et al. Empagliflozin, cardiovascular outcomes, and mortality in type 2 diabetes. N Engl J Med. 2015; 373:2117–28.
Article11. Kim HK, Song SO, Noh J, Jeong IK, Lee BW. Data configuration and publication trends for the Korean National Health Insurance and Health Insurance Review & Assessment Database. Diabetes Metab J. 2020; 44:671–8.
Article12. Kim SM, Jang WM, Ahn HA, Park HJ, Ahn HS. Korean National Health Insurance value incentive program: achievements and future directions. J Prev Med Public Health. 2012; 45:148–55.
Article13. Li S, Wang J, Zhang B, Li X, Liu Y. Diabetes mellitus and cause-specific mortality: a population-based study. Diabetes Metab J. 2019; 43:319–41.
Article14. Kim NH. Diabetes mellitus, still major threat to mortality from various causes. Diabetes Metab J. 2019; 43:273–5.
Article15. Preis SR, Hwang SJ, Coady S, Pencina MJ, D’Agostino RB Sr, Savage PJ, et al. Trends in all-cause and cardiovascular disease mortality among women and men with and without diabetes mellitus in the Framingham Heart Study, 1950 to 2005. Circulation. 2009; 119:1728–35.
Article16. Luk AO, Hui EM, Sin MC, Yeung CY, Chow WS, Ho AY, et al. Declining trends of cardiovascular-renal complications and mortality in type 2 diabetes: the Hong Kong Diabetes Database. Diabetes Care. 2017; 40:928–35.
Article17. Tachkov K, Mitov K, Koleva Y, Mitkova Z, Kamusheva M, Dimitrova M, et al. Life expectancy and survival analysis of patients with diabetes compared to the non diabetic population in Bulgaria. PLoS One. 2020; 15:e0232815.
Article18. Gregg EW, Cheng YJ, Srinivasan M, Lin J, Geiss LS, Albright AL, et al. Trends in cause-specific mortality among adults with and without diagnosed diabetes in the USA: an epidemiological analysis of linked national survey and vital statistics data. Lancet. 2018; 391:2430–40.
Article19. Rosella LC, Calzavara A, Frank JW, Fitzpatrick T, Donnelly PD, Henry D. Narrowing mortality gap between men and women over two decades: a registry-based study in Ontario, Canada. BMJ Open. 2016; 6:e012564.
Article20. Song Y, Liu X, Zhu X, Zhao B, Hu B, Sheng X, et al. Increasing trend of diabetes combined with hypertension or hypercholesterolemia: NHANES data analysis 1999-2012. Sci Rep. 2016; 6:36093.
Article21. Kim MK, Ko SH, Kim BY, Kang ES, Noh J, Kim SK, et al. 2019 Clinical practice guidelines for type 2 diabetes mellitus in Korea. Diabetes Metab J. 2019; 43:398–406.
Article22. American Diabetes Association. 10. Cardiovascular disease and risk management: standards of medical care in diabetes-2020. Diabetes Care. 2020; 43(Suppl 1):S111–34.23. Rawshani A, Rawshani A, Franzen S, Sattar N, Eliasson B, Svensson AM, et al. Risk factors, mortality, and cardiovascular outcomes in patients with type 2 diabetes. N Engl J Med. 2018; 379:633–44.
Article24. Suh S, Kim KW. Diabetes and cancer: cancer should be screened in routine diabetes assessment. Diabetes Metab J. 2019; 43:733–43.
Article25. Campbell PT, Newton CC, Patel AV, Jacobs EJ, Gapstur SM. Diabetes and cause-specific mortality in a prospective cohort of one million U.S. adults. Diabetes Care. 2012; 35:1835–44.
Article26. Cheng YJ, Imperatore G, Geiss LS, Saydah SH, Albright AL, Ali MK, et al. Trends and disparities in cardiovascular mortality among U.S. adults with and without self-reported diabetes, 1988-2015. Diabetes Care. 2018; 41:2306–15.
Article27. Nakamura J, Kamiya H, Haneda M, Inagaki N, Tanizawa Y, Araki E, et al. Causes of death in Japanese patients with diabetes based on the results of a survey of 45,708 cases during 2001-2010: report of Committee on Causes of Death in Diabetes Mellitus. Diabetol Int. 2017; 8:117–36.
Article28. Kim KJ, Kwon TY, Yu S, Seo JA, Kim NH, Choi KM, et al. Ten-year mortality trends for adults with and without diabetes mellitus in South Korea, 2003 to 2013. Diabetes Metab J. 2018; 42:394–401.
Article29. Lee SU, Park JI, Lee S, Oh IH, Choi JM, Oh CM. Changing trends in suicide rates in South Korea from 1993 to 2016: a descriptive study. BMJ Open. 2018; 8:e023144.
Article30. Kim D, Li AA, Cholankeril G, Kim SH, Ingelsson E, Knowles JW, et al. Trends in overall, cardiovascular and cancer-related mortality among individuals with diabetes reported on death certificates in the United States between 2007 and 2017. Diabetologia. 2019; 62:1185–94.
Article31. Bragg F, Holmes MV, Iona A, Guo Y, Du H, Chen Y, et al. Association between diabetes and cause-specific mortality in rural and urban areas of China. JAMA. 2017; 317:280–9.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A guide for the utilization of Health Insurance Review and Assessment Service National Patient Samples
- Using the National Health Information Database of the National Health Insurance Service in Korea for Monitoring Mortality and Life Expectancy at National and Local Levels
- Status of Diabetic Neuropathy in Korea: A National Health Insurance Service-National Sample Cohort Analysis (2006 to 2015) (Diabetes Metab J 2021;45:115-9)
- The Diabetes Epidemic in Korea
- Data Analytic Process of a Nationwide Population-Based Study Using National Health Information Database Established by National Health Insurance Service