Temporal trends in the prevalence of metabolically healthy overweight and obesity in Korean youth: data from the Korea National Health and Nutrition Examination Survey 2011–2019
- Affiliations
-
- 1Department of Pediatrics, Seoul National University Children's Hospital, Seoul, Korea
- 2Department of Pediatrics, Seoul National University Bundang Hospital, Seongnam, Korea
- 3Department of Pediatrics, Seoul National University College of Medicine, Seoul, Korea
- KMID: 2531278
- DOI: http://doi.org/10.6065/apem.2142192.096
Abstract
- Purpose
Metabolically healthy overweight/obesity (MHO) and metabolically unhealthy overweight/obesity (MUO) are distinct clinical phenotypes classified by the presence of cardiometabolic risk factors in an individual. In the present study, we investigated temporal trends in the prevalence of MHO in Korean adolescents using nationally representative data.
Methods
Data from the Korea National Health and Nutrition Examination Survey 2011–2019 were used in this study. A total of 5,667 adolescents (3,014 boys, 53.2%) aged 10–18 years was included in this study. MHO was defined as a body mass index ≥85th percentile for the corresponding age and sex and absence of any cardiometabolic risk factors.
Results
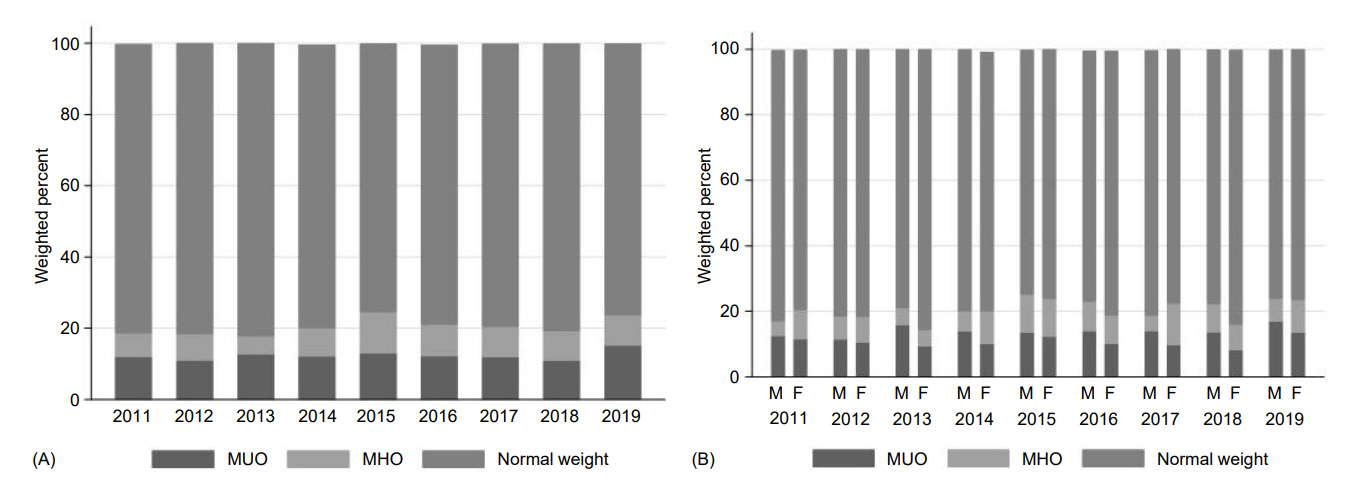
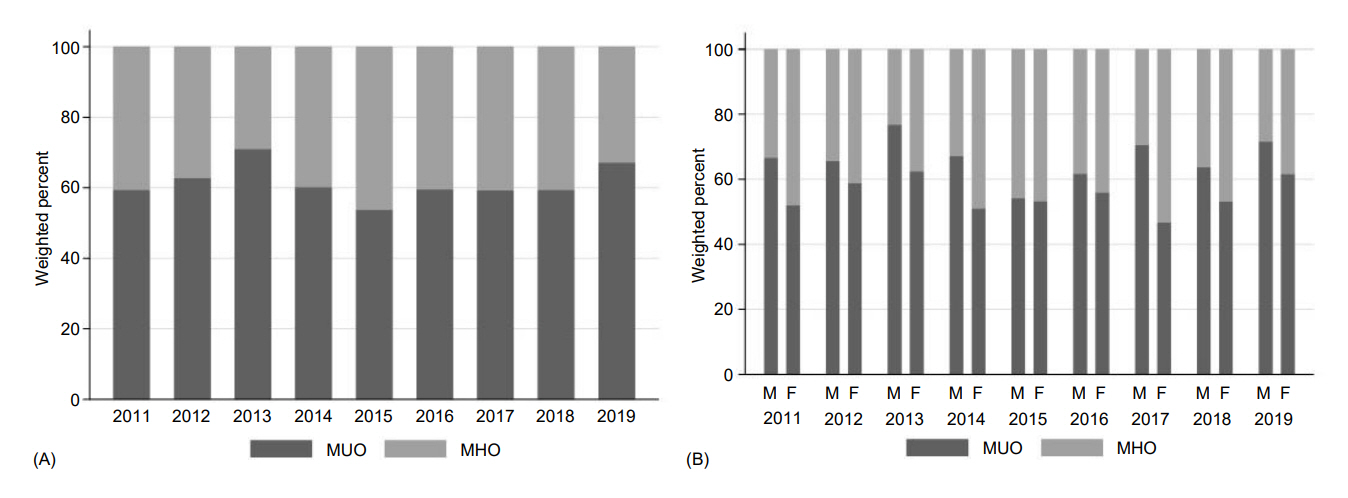
The prevalence of overweight/obesity showed an increasing trend from 18.8% (boys 17.3% and girls 20.6%) in 2011 to 23.7% (boys 24.0% and girls 23.5%) in 2019 (p for trend=0.045). The overall prevalence of MHO during 2011–2019 was 39.2%, which was higher in girls than in boys (boys 33.5%, girls 46.2%, p<0.001), and the change in prevalence of MHO from 2011 to 2019 (from 34.8% to 35.7%) was not significant. Among MUO, the most prevalent cardiometabolic risk factor was dysglycemia (48.8%), followed by elevated blood pressure (41.5%), low high-density lipoprotein cholesterol (35.0%), and high triglycerides (29.7%).
Conclusion
We observed a high prevalence of MHO in Korean youth with overweight/obesity. Although the prevalence of overweight/obesity increased, the prevalence of MHO was stable during 2011-2019. A risk-stratified approach based on metabolic health status can help reducing the medical and socioeconomic costs associated with obesity treatment.
Keyword
Figure
Cited by 3 articles
-
Waist-height ratio and body mass index as indicators of obesity and cardiometabolic risk in Korean children and adolescents
Min Yeong Kim, Sejin An, Young Suk Shim, Hae Sang Lee, Jin Soon Hwang
Ann Pediatr Endocrinol Metab. 2024;29(3):182-190. doi: 10.6065/apem.2346090.045.The impacts of COVID-19 on childhood obesity: prevalence, contributing factors, and implications for management
Min-Ji Kim, Minji Kim, Ju Young Yoon, Chong Kun Cheon, Sukdong Yoo
Ann Pediatr Endocrinol Metab. 2024;29(3):174-181. doi: 10.6065/apem.2346094.047.Association between metabolically healthy obesity and carotid intima-media thickness in Korean adolescents with overweight and obesity
Sohyun Shin, Hwa Young Kim, Joowon Lee, Young Jin Ryu, Ji Young Kim, Jaehyun Kim
Ann Pediatr Endocrinol Metab. 2024;29(4):227-233. doi: 10.6065/apem.2346192.096.
Reference
-
References
1. Abarca-Gómez L, Abdeen ZA, Hamid ZA, Abu-Rmeileh NM, Acosta-Cazares B, Acuin C, et al. Worldwide trends in body-mass index, underweight, overweight, and obesity from 1975 to 2016: a pooled analysis of 2416 population-based measurement studies in 128·9 million children, adolescents, and adults. Lancet. 2017; 390:2627–42.2. Steinberger J, Daniels SR, Eckel RH, Hayman L, Lustig RH, McCrindle B, et al. Progress and challenges in metabolic syndrome in children and adolescents: a scientific statement from the American Heart Association Atherosclerosis, Hypertension, and Obesity in the Young Committee of the Council on Cardiovascular Disease in the Young; Council on Cardiovascular Nursing; and Council on Nutrition, Physical Activity, and Metabolism. Circulation. 2009; 119:628–47.3. Singh AS, Mulder C, Twisk JW, Van Mechelen W, Chinapaw MJ. Tracking of childhood overweight into adulthood: a systematic review of the literature. Obes Rev. 2008; 9:474–88.4. Park MH, Falconer C, Viner RM, Kinra S. The impact of childhood obesity on morbidity and mortality in adulthood: a systematic review. Obes Rev. 2012; 13:985–1000.5. Prince RL, Kuk JL, Ambler KA, Dhaliwal J, Ball GD. Predictors of metabolically healthy obesity in children. Diabetes Care. 2014; 37:1462–8.6. Ma LZ, Sun FR, Wang ZT, Tan L, Hou XH, Ou YN, et al. Metabolically healthy obesity and risk of stroke: a metaanalysis of prospective cohort studies. Ann Transl Med. 2021; 9:197.7. Caleyachetty R, Thomas GN, Toulis KA, Mohammed N, Gokhale KM, Balachandran K, et al. Metabolically healthy obese and incident cardiovascular disease events among 3.5 million men and women. J Am Coll Cardiol. 2017; 70:1429–37.8. Damanhoury S, Newton A, Rashid M, Hartling L, Byrne J, Ball G. Defining metabolically healthy obesity in children: a scoping review. Obes Rev. 2018; 19:1476–91.9. Yoon DY, Lee YA, Lee J, Kim JH, Shin CH, Yang SW. Prevalence and clinical characteristics of metabolically healthy obesity in Korean children and adolescents: data from the Korea National Health and Nutrition Examination Survey. J Korean Med Sci. 2017; 32:1840–7.10. Kweon S, Kim Y, Jang MJ, Kim Y, Kim K, Choi S, et al. Data resource profile: the Korea national health and nutrition examination survey (KNHANES). Int J Epidemiol. 2014; 43:69–77.11. Kim JH, Yun S, Hwang SS, Shim JO, Chae HW, Lee YJ, et al. The 2017 Korean National Growth Charts for children and adolescents: development, improvement, and prospects. Korean J Pediatr. 2018; 61:135–49.12. Styne DM, Arslanian SA, Connor EL, Farooqi IS, Murad MH, Silverstein JH, et al. Pediatric obesity–assessment, treatment, and prevention: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metabol. 2017; 102:709–57.13. Petersmann A, Müller-Wieland D, Müller UA, Landgraf R, Nauck M, Freckmann G, et al. Definition, classification and diagnosis of diabetes mellitus. Exp Clin Endocrinol Diabetes. 2019; 127(S 01):S1–7.14. Di Cesare M, Sorić M, Bovet P, Miranda JJ, Bhutta Z, Stevens GA, et al. The epidemiological burden of obesity in childhood: a worldwide epidemic requiring urgent action. BMC Med. 2019; 17:212.15. Kim JH, Moon JS. Secular trends in pediatric overweight and obesity in Korea. J Obesity Metab Syndr. 2020; 29:12–7.16. Seo MY, Kim SH, Park MJ. Changes in anthropometric indices among Korean school students based on the 2010 and 2018 Korea School Health Examination Surveys. Ann Pediatr Endocrinol Metab. 2021; 26:38–45.17. Korea Disease Control and Prevention Agency. The sixteenth Korea Youth Risk Behavior Web-based Survey (KYRBS) [Internet]. Cheongju (Korea): Korea Disease Control and Prevention Agency;2020. [cited 2021 Oct 5]. Available from: https://www.kdca.go.kr/yhs/home.jsp.18. Skinner AC, Perrin EM, Moss LA, Skelton JA. Cardiometabolic risks and severity of obesity in children and young adults. N Engl J Med. 2015; 373:1307–17.19. Castorani V, Polidori N, Giannini C, Blasetti A, Chiarelli F. Insulin resistance and type 2 diabetes in children. Ann Pediatr Endocrinol Metab. 2020; 25:217–26.20. Velho S, Paccaud F, Waeber G, Vollenweider P, Marques-Vidal P. Metabolically healthy obesity: different prevalences using different criteria. Eur J Clin Nutr. 2010; 64:1043–51.21. Blüher S, Schwarz P. Metabolically healthy obesity from childhood to adulthood –does weight status alone matter? Metabolism. 2014; 63:1084–92.22. Rey-López JP, De Rezende LF, Pastor-Valero M, Tess BH. The prevalence of metabolically healthy obesity: a systematic review and critical evaluation of the definitions used. Obes Rev. 2014; 15:781–90.23. Videira-Silva A, Freira S, Fonseca H. Metabolically healthy overweight adolescents: definition and components. Ann Pediatr Endocrinol Metab. 2020; 25:256–64.24. Sénéchal M, Wicklow B, Wittmeier K, Hay J, MacIntosh AC, Eskicioglu P, et al. Cardiorespiratory fitness and adiposity in metabolically healthy overweight and obese youth. Pediatrics. 2013; 132:e85–92.25. Choi YS, Beltran TA, Klaric JS. Prevalence of optimal metabolic health in U.S. adolescents, NHANES 2007–2016. Metab Syndr Relat Disord. 2021; 19:56–63.26. Aldhoon-Hainerová I, Zamrazilová H, Hill M, Hainer V. Insulin sensitivity and its relation to hormones in adolescent boys and girls. Metabolism. 2017; 67:90–8.27. Cadenas-Sanchez C, Ruiz JR, Labayen I, Huybrechts I, Manios Y, González-Gross M, et al. Prevalence of metabolically healthy but overweight/obese phenotype and its association with sedentary time, physical activity, and fitness. J Adolesc Health. 2017; 61:107–14.28. Vukovic R, Milenkovic T, Mitrovic K, Todorovic S, Plavsic L, Vukovic A, et al. Preserved insulin sensitivity predicts metabolically healthy obese phenotype in children and adolescents. Eur J Pediatr. 2015; 174:1649–55.29. Isasi CR, Parrinello CM, Ayala GX, Delamater AM, Perreira KM, Daviglus ML, et al. Sex differences in cardiometabolic risk factors among Hispanic/Latino youth. J Pediatr. 2016; 176:121–7.e1.30. Camhi SM, Crouter SE, Hayman LL, Must A, Lichtenstein AH. Lifestyle behaviors in metabolically healthy and unhealthy overweight and obese women: a preliminary study. PLoS One. 2015; 10:e0138548.31. Hankinson AL, Daviglus ML, Horn LV, Chan Q, Brown I, Holmes E, et al. Diet composition and activity level of at risk and metabolically healthy obese American adults. Obesity (Silver Spring). 2013; 21:637–43.32. Matta J, Nasreddine L, Jomaa L, Hwalla N, Mehio Sibai A, Czernichow S, et al. Metabolically healthy overweight and obesity is associated with higher adherence to a traditional dietary pattern: a cross-sectional study among adults in Lebanon. Nutrients. 2016; 8:432.33. Camhi SM, Evans EW, Hayman LL, Lichtenstein AH, Must A. Healthy eating index and metabolically healthy obesity in U.S. adolescents and adults. Prev Med. 2015; 77:23–7.34. Phillips CM, Dillon C, Harrington JM, McCarthy VJ, Kearney PM, Fitzgerald AP, et al. Defining metabolically healthy obesity: role of dietary and lifestyle factors. PLoS One. 2013; 8:e76188.35. de Rooij BH, van der Berg JD, van der Kallen CJ, Schram MT, Savelberg HH, Schaper NC, et al. Physical activity and sedentary behavior in metabolically healthy versus unhealthy obese and non-obese individuals – The Maastricht Study. PLoS One. 2016; 11:e0154358.36. Phillips CM. Metabolically healthy obesity: personalised and public health implications. Trends Endocrinol Metab. 2016; 27:189–91.37. Li S, Chen W, Srinivasan SR, Xu J, Berenson GS. Relation of childhood obesity/cardiometabolic phenotypes to adult cardiometabolic profile: the Bogalusa Heart Study. Am J Epidemiol. 2012; 176 Suppl 7:S142–9.38. Achilike I, Hazuda HP, Fowler SP, Aung K, Lorenzo C. Predicting the development of the metabolically healthy obese phenotype. Int J Obes (Lond). 2015; 39:228–34.39. Mongraw-Chaffin M, Foster MC, Anderson CA, Burke GL, Haq N, Kalyani RR, et al. Metabolically healthy obesity, transition to metabolic syndrome, and cardiovascular risk. J Am Coll Cardiol. 2018; 71:1857–65.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Trends in the Prevalence of Obesity and Its Phenotypes Based on the Korea National Health and Nutrition Examination Survey from 2007 to 2017 in Korea
- Prevalence Rates and Risk Factors of Overweight and Obesity in Children and Adolescents: Using Korean National Health and Nutrition Examination Survey 2005 Data
- Trends in Obesity Prevalence by Occupation Based on Korean National Health and Nutrition Examination Survey From 1998 to 2015
- Comparison of Obesity and Overweight Prevalence Among Korean Adults According to Community Health Survey and Korea National Health and Nutrition Examination Survey
- Prevalence and Clinical Characteristics of Metabolically Healthy Obesity in Korean Children and Adolescents: Data from the Korea National Health and Nutrition Examination Survey