Ann Surg Treat Res.
2022 Jun;102(6):328-334. 10.4174/astr.2022.102.6.328.
The development and clinical efficacy of simulation training of open duct-to-mucosa pancreaticojejunostomy using pancreas and intestine silicone models
- Affiliations
-
- 1Department of Surgery and Cancer Research Institute, Seoul National University College of Medicine, Seoul, Korea
- 2Department of Surgery, Korea University Guro Hospital, Korea University College of Medicine, Seoul, Korea
- 3Department of Surgery, Chung-Ang University Gwangmyeong Hospital, Gwangmyeong, Korea
- 4Department of Surgery, Korea University Anam Hospital, Korea University College of Medicine, Seoul, Korea
- 5Department of Surgery, Uijeongbu Eulji Medical Center, Eulji University, Uijeongbu, Korea
- 6Department of Surgery, Hallym University Dongtan Sacred Heart Hospital, Hwaseong, Korea
- 7Department of Surgery, Kangbuk Samsung Hospital, Sungkyunkwan University School of Medicine, Seoul, Korea
- 8Department of Surgery, Goodjang Hospital, Seoul, Korea
- KMID: 2530387
- DOI: http://doi.org/10.4174/astr.2022.102.6.328
Abstract
- Purpose
As pancreaticojejunostomy (PJ) is a challenging anastomosis, an education program is needed to train young surgeons to perform PJ. This study evaluated the effects of simulation-based training of open PJ using pancreas and intestine silicone models.
Methods
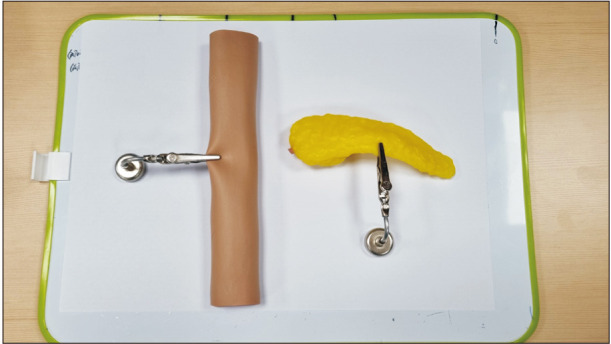
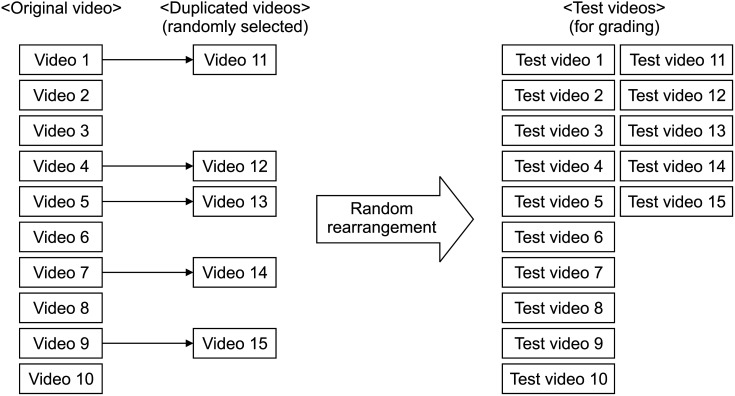
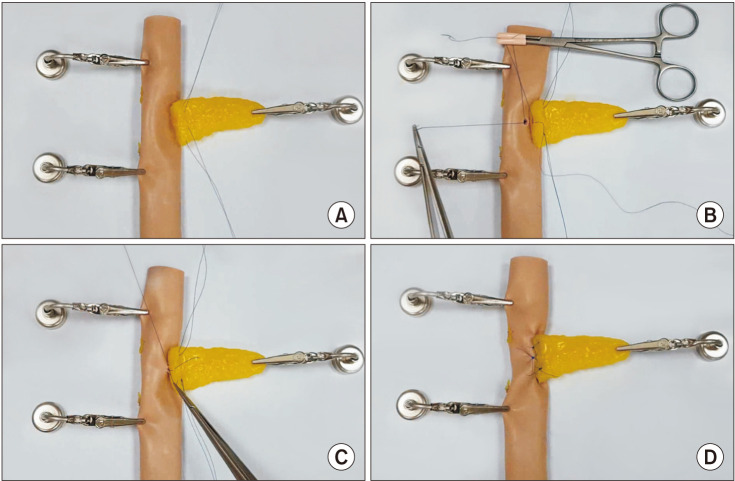
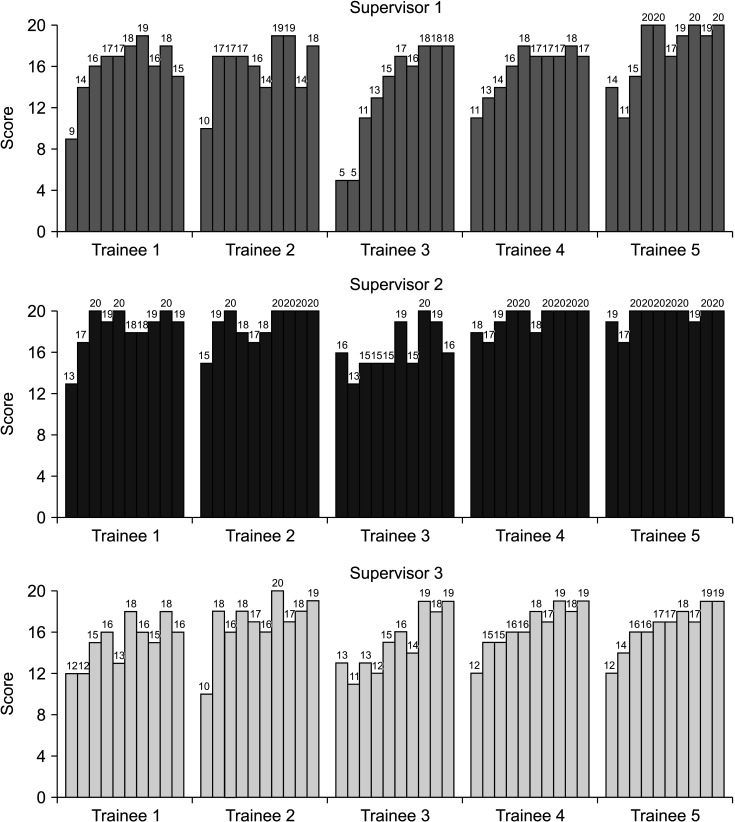
Five videos pancreatobiliary clinical fellows who did not perform PJ participated in this study. After watching the master video created by a senior pancreatobiliary surgeon, each trainee performed the PJ using silicone models and recorded them 10 times using a video camera. Of these videos, 5 were randomly duplicated due to the validation of the scoring system. The scoring system developed consisted of 20 scores. Three pancreatobiliary professors scored their performance by watching videos.
Results
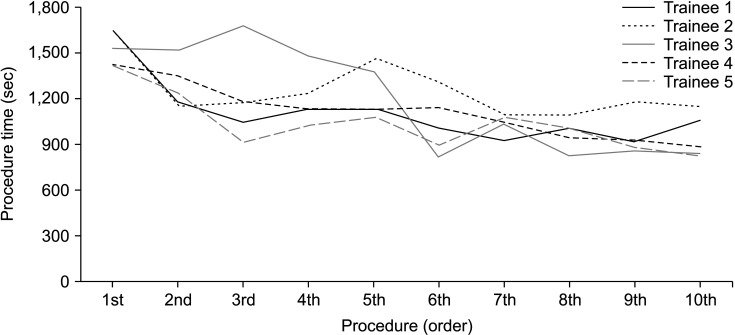
The mean procedure time of the 5 trainees was 25.4 minutes (range, 23.5–27.3 minutes) in the first video and 15.8 minutes (range, 13.8–19.1 minutes) in the 10th video. The mean score was 12.6 (range, 5–19) and 18.3 (range, 15–20) in the first and 10th videos, respectively. The scores were similar among the duplicated videos for each supervisor.
Conclusion
This education system would help pancreatobiliary trainees to overcome learning curves efficiently without ethical issues related to animal models or direct practice to human patients.
Figure
Cited by 1 articles
-
Training efficacy of robotic duct-to-mucosa pancreaticojejunostomy simulation using silicone models for surgical fellows
Mirang Lee, Youngmin Han, Jae Seung Kang, Yoo Jin Choi, Hee Ju Sohn, Wooil Kwon, Jin-Young Jang
Ann Surg Treat Res. 2024;106(1):45-50. doi: 10.4174/astr.2024.106.1.45.
Reference
-
1. Egle JP, Malladi SV, Gopinath N, Mittal VK. Simulation training improves resident performance in hand-sewn vascular and bowel anastomoses. J Surg Educ. 2015; 72:291–296. PMID: 25481803.
Article2. Fonseca AL, Evans LV, Gusberg RJ. Open surgical simulation in residency training: a review of its status and a case for its incorporation. J Surg Educ. 2013; 70:129–137. PMID: 23337682.
Article3. Hogg ME, Zenati M, Novak S, Chen Y, Jun Y, Steve J, et al. Grading of surgeon technical performance predicts postoperative pancreatic fistula for pancreaticoduodenectomy independent of patient-related variables. Ann Surg. 2016; 264:482–491. PMID: 27433897.
Article4. Davies J, Khatib M, Bello F. Open surgical simulation: a review. J Surg Educ. 2013; 70:618–627. PMID: 24016373.5. Santos DR, Calvo FC, Feijó DH, Araújo NP, Teixeira RK, Yasojima EY. New training model using chickens intestine for pediatric intestinal anastomosis. Acta Cir Bras. 2019; 34:e201900709. PMID: 31531529.
Article6. Uemura M, Yamashita M, Tomikawa M, Obata S, Souzaki R, Ieiri S, et al. Objective assessment of the suture ligature method for the laparoscopic intestinal anastomosis model using a new computerized system. Surg Endosc. 2015; 29:444–452. PMID: 25005015.
Article7. Choi M, Kang CM. Developing an in vivo porcine model of duct-to-mucosa pancreaticojejunostomy (Yonsei-PJDTM). Ann Gastroenterol Surg. 2020; 4:180–184. PMID: 32258985.
Article8. Tam V, Zenati M, Novak S, Chen Y, Zureikat AH, Zeh HJ 3rd, et al. Robotic pancreatoduodenectomy biotissue curriculum has validity and improves technical performance for surgical oncology fellows. J Surg Educ. 2017; 74:1057–1065. PMID: 28578981.
Article9. Wei F, Xu M, Lai X, Zhang J, Yiengpruksawan A, Lu Y, et al. Three-dimensional printed dry lab training models to simulate robotic-assisted pancreaticojejunostomy. ANZ J Surg. 2019; 89:1631–1635. PMID: 31692187.
Article10. Yang JR, Xiao R, Zhou J, Wang L, Wang JX, Zhang Q, et al. Establishment of a canine training model for digestive tract reconstruction after pancreaticoduodenectomy. J Invest Surg. 2021; 34:561–567. PMID: 31588822.
Article11. Yoshioka R, Imamura H, Ichida H, Gyoda Y, Mizuno T, Mise Y, et al. Simulation training in pancreatico-jejunostomy using an inanimate biotissue model improves the technical skills of hepatobiliary-pancreatic surgical fellows. PLoS One. 2021; 16:e0244915. PMID: 33439895.
Article12. Martin JA, Regehr G, Reznick R, MacRae H, Murnaghan J, Hutchison C, et al. Objective structured assessment of technical skill (OSATS) for surgical residents. Br J Surg. 1997; 84:273–278. PMID: 9052454.
Article13. Byun Y, Choi YJ, Han Y, Kang JS, Kim H, Kwon W, et al. Outcomes of 5000 pancreatectomies in Korean single referral center and literature reviews. J Hepatobiliary Pancreat Sci. 2021; 02. 26. DOI: 10.1002/jhbp.933. [Epub].
Article14. Malas T, Al-Atassi T, Brandys T, Naik V, Lapierre H, Lam BK. Impact of visualization on simulation training for vascular anastomosis. J Thorac Cardiovasc Surg. 2018; 155:1686–1693. PMID: 29554789.
Article15. Fisher WE, Hodges SE, Wu MF, Hilsenbeck SG, Brunicardi FC. Assessment of the learning curve for pancreaticoduodenectomy. Am J Surg. 2012; 203:684–690. PMID: 22079032.
Article16. Schmidt CM, Turrini O, Parikh P, House MG, Zyromski NJ, Nakeeb A, et al. Effect of hospital volume, surgeon experience, and surgeon volume on patient outcomes after pancreaticoduodenectomy: a single-institution experience. Arch Surg. 2010; 145:634–640. PMID: 20644125.
Article17. Ziv A, Wolpe PR, Small SD, Glick S. Simulation-based medical education: an ethical imperative. Simul Healthc. 2006; 1:252–256. PMID: 19088599.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Training efficacy of robotic duct-to-mucosa pancreaticojejunostomy simulation using silicone models for surgical fellows
- The Duct to mucosa method for a pancreaticojejun-ostomy:continuous stitches modification
- CORRIGENDUM: Training efficacy of robotic duct-to-mucosa pancreaticojejunostomy simulation using silicone models for surgical fellows
- The Complication Rate according to the Method of Pancreaticojejunostomy after Pancreaticoduodenectomy
- Congenital Heart Surgery Skill Training Using Simulation Models: Not an Option but a Necessity