J Korean Med Sci.
2022 Apr;37(16):e127. 10.3346/jkms.2022.37.e127.
Association of Maternal Hypertensive Disorders During Pregnancy With Severe Bronchopulmonary Dysplasia: A Systematic Review and Meta-Analysis
- Affiliations
-
- 1Department of Pediatrics, Ulsan University Hospital, University of Ulsan College of Medicine, Ulsan, Korea
- 2Department of Pediatrics, Konkuk University Medical Center, Seoul, Korea
- 3Konkuk University School of Medicine, Seoul, Korea
- KMID: 2529294
- DOI: http://doi.org/10.3346/jkms.2022.37.e127
Abstract
- Background
This meta-analysis was performed to examine the association between maternal hypertension during pregnancy (HDP) and neonatal bronchopulmonary dysplasia (BPD).
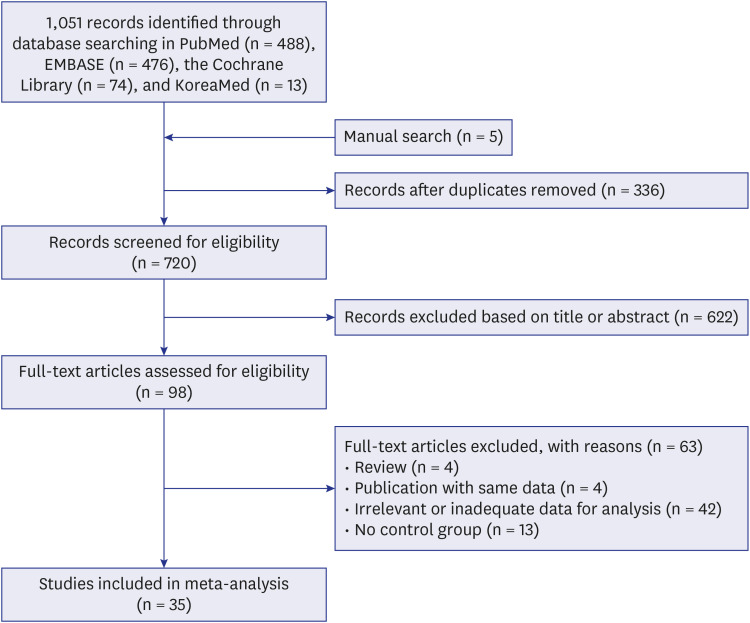
Methods
We systematically searched PubMed, EMBASE, the Cochrane Library, and the KoreaMed database for relevant studies. We used the Newcastle-Ottawa Scale for quality assessment of all included studies. The meta-analysis was performed using Comprehensive Meta-Analysis software (version 3.3).
Results
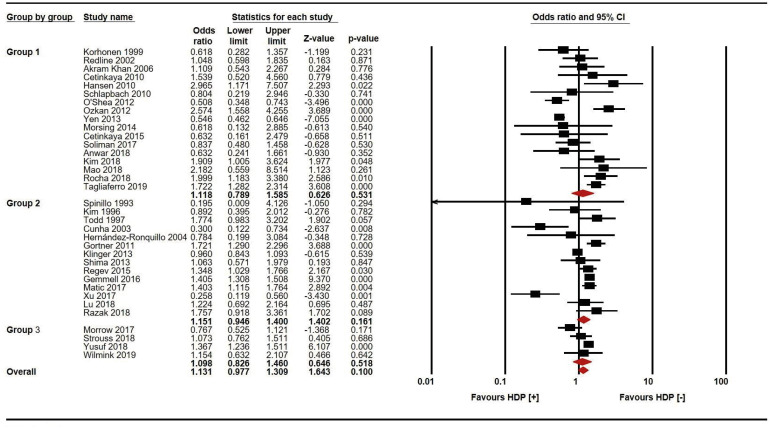
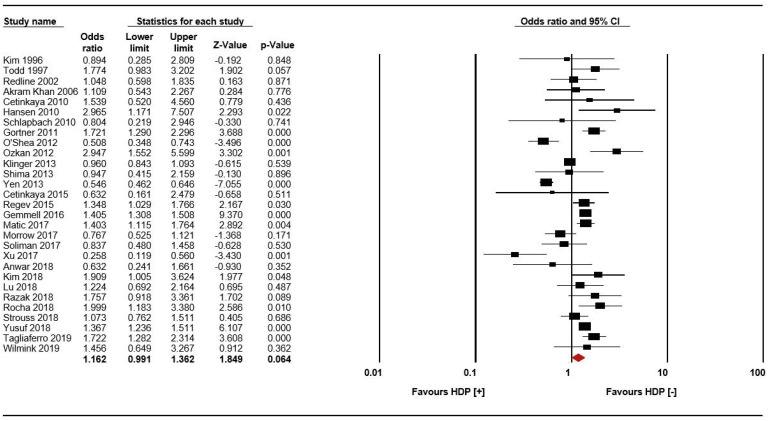
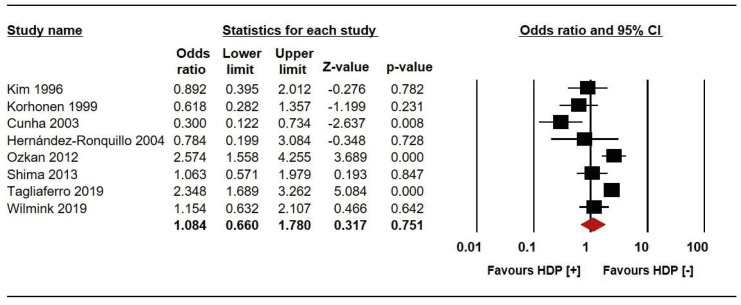
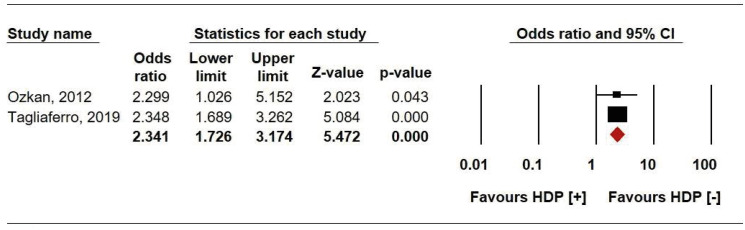
We included 35 studies that fulfilled the inclusion criteria; the total number of infants evaluated came to 97,399 through review process. Maternal HDP was not significantly associated with any definition of BPD, i.e., oxygen dependency at 36 weeks of gestation (odds ratio [OR], 1.162; 95% confidence interval [CI], 0.991–1.362; P = 0.064) in pooled analysis of 29 studies or oxygen dependency at 28 days of age (OR, 1.084; 95% CI, 0.660–1.780; P = 0.751) in pooled analysis of 8 studies. Maternal HDP was significantly associated only with severe BPD (OR, 2.341; 95% CI, 1.726–3.174; P < 0.001). BPD was not associated with HDP in the overall analysis (OR, 1.131; 95% CI, 0.977–1.309; P = 0.100) or subgroup analysis according to the definition of HDP.
Conclusion
Maternal HDP was not associated with neonatal BPD defined by the duration of oxygen dependency (at either 36 weeks of gestation or 28 days of life) but was associated with severe BPD.
Figure
Reference
-
1. Jobe AJ. The new BPD: an arrest of lung development. Pediatr Res. 1999; 46(6):641–643. PMID: 10590017.2. Mandell EW, Abman SH. Fetal vascular origins of bronchopulmonary dysplasia. J Pediatr. 2017; 185:7–10.e1. PMID: 28359535.3. Abman SH. Bronchopulmonary dysplasia: “a vascular hypothesis”. Am J Respir Crit Care Med. 2001; 164(10 Pt 1):1755–1756. PMID: 11734417.4. Shim SY, Yun JY, Cho SJ, Kim MH, Park EA. The prediction of bronchopulmonary dysplasia in very low birth weight infants through clinical indicators within 1 hour of delivery. J Korean Med Sci. 2021; 36(11):e81. PMID: 33754511.5. Sung TJ. Bronchopulmonary dysplasia: How can we improve its outcomes? Korean J Pediatr. 2019; 62(10):367–373. PMID: 31122011.6. Park HW, Lim G, Chung SH, Chung S, Kim KS, Kim SN. Early caffeine use in very low birth weight infants and neonatal outcomes: a systematic review and meta-analysis. J Korean Med Sci. 2015; 30(12):1828–1835. PMID: 26713059.7. Jeon GW. Changes in the incidence of bronchopulmonary dysplasia among preterm infants in a single center over 10 years. Neonatal Med. 2020; 27(1):1–7.8. Hansen AR, Barnés CM, Folkman J, McElrath TF. Maternal preeclampsia predicts the development of bronchopulmonary dysplasia. J Pediatr. 2010; 156(4):532–536. PMID: 20004912.9. Bi GL, Chen FL, Huang WM. The association between hypertensive disorders in pregnancy and bronchopulmonary dysplasia: a systematic review. World J Pediatr. 2013; 9(4):300–306. PMID: 24235063.10. Torchin H, Ancel PY, Goffinet F, Hascoët J-M, Truffert P, Tran D, et al. Placental complications and bronchopulmonary dysplasia: EPIPAGE-2 cohort study. Pediatrics. 2016; 137(3):e20152163. PMID: 26908662.11. Dravet-Gounot P, Torchin H, Goffinet F, Aubelle MS, El Ayoubi M, Lefevre C, et al. Bronchopulmonary dysplasia in neonates born to mothers with preeclampsia: impact of small for gestational age. PLoS One. 2018; 13(9):e0204498. PMID: 30248159.12. O’Shea JE, Davis PG, Doyle LW. Victorian Infant Collaborative Study Group. Maternal preeclampsia and risk of bronchopulmonary dysplasia in preterm infants. Pediatr Res. 2012; 71(2):210–214. PMID: 22258134.13. Sibai B, Dekker G, Kupferminc M. Pre-eclampsia. Lancet. 2005; 365(9461):785–799. PMID: 15733721.14. Report of the national high blood pressure education program working group on high blood pressure in pregnancy. Am J Obstet Gynecol. 2000; 183(1):S1–22.15. Mestan KK, Gotteiner N, Porta N, Grobman W, Su EJ, Ernst LM. Cord blood biomarkers of placental maternal vascular underperfusion predict bronchopulmonary dysplasia-associated pulmonary hypertension. J Pediatr. 2017; 185:33–41. PMID: 28162769.16. Strouss L, Goldstein ND, Locke R, Paul DA. Vascular placental pathology and the relationship between hypertensive disorders of pregnancy and neonatal outcomes in very low birth weight infants. J Perinatol. 2018; 38(4):324–331. PMID: 29311628.17. Spinillo A, Stronati M, Ometto A, Fazzi E, Lanzi G, Guaschino S. Infant neurodevelopmental outcome in pregnancies complicated by gestational hypertension and intra-uterine growth retardation. J Perinat Med. 1993; 21(3):195–203. PMID: 8229610.18. Kim CR, Vohr BR, Oh W. Effects of maternal hypertension in very-low-birth-weight infants. Arch Pediatr Adolesc Med. 1996; 150(7):686–691. PMID: 8673191.19. Todd DA, Jana A, John E. Chronic oxygen dependency in infants born at 24-32 weeks’ gestation: the role of antenatal and neonatal factors. J Paediatr Child Health. 1997; 33(5):402–407. PMID: 9401883.20. Cunha GS, Mezzacappa Filho F, Ribeiro JD. Maternal and neonatal factors affecting the incidence of bronchopulmonary dysplasia in very low birth weight newborns. J Pediatr (Rio J). 2003; 79(6):550–556. PMID: 14685454.21. Akram Khan M, Kuzma-O’Reilly B, Brodsky NL, Bhandari V. Site-specific characteristics of infants developing bronchopulmonary dysplasia. J Perinatol. 2006; 26(7):428–435. PMID: 16724120.22. Cetinkaya M, Ozkan H, Köksal N, Karali Z, Ozgür T. Neonatal outcomes of premature infants born to preeclamptic mothers. J Matern Fetal Neonatal Med. 2010; 23(5):425–430. PMID: 19670043.23. Schlapbach LJ, Ersch J, Adams M, Bernet V, Bucher HU, Latal B. Impact of chorioamnionitis and preeclampsia on neurodevelopmental outcome in preterm infants below 32 weeks gestational age. Acta Paediatr. 2010; 99(10):1504–1509. PMID: 20456275.24. Ozkan H, Cetinkaya M, Koksal N. Increased incidence of bronchopulmonary dysplasia in preterm infants exposed to preeclampsia. J Matern Fetal Neonatal Med. 2012; 25(12):2681–2685. PMID: 22759075.25. Shima Y, Kumasaka S, Migita M. Perinatal risk factors for adverse long-term pulmonary outcome in premature infants: comparison of different definitions of bronchopulmonary dysplasia/chronic lung disease. Pediatr Int. 2013; 55(5):578–581. PMID: 23745727.26. Yen TA, Yang HI, Hsieh WS, Chou HC, Chen CY, Tsou KI, et al. Preeclampsia and the risk of bronchopulmonary dysplasia in VLBW infants: a population based study. PLoS One. 2013; 8(9):e75168. PMID: 24073247.27. Morsing E, Maršál K. Pre-eclampsia- an additional risk factor for cognitive impairment at school age after intrauterine growth restriction and very preterm birth. Early Hum Dev. 2014; 90(2):99–101. PMID: 24388669.28. Gemmell L, Martin L, Murphy KE, Modi N, Håkansson S, Reichman B, et al. Hypertensive disorders of pregnancy and outcomes of preterm infants of 24 to 28 weeks’ gestation. J Perinatol. 2016; 36(12):1067–1072. PMID: 27583388.29. Matić M, Inati V, Abdel-Latif ME, Kent AL. NSW ACT NICUS Network. Maternal hypertensive disorders are associated with increased use of respiratory support but not chronic lung disease or poorer neurodevelopmental outcomes in preterm neonates at <29 weeks of gestation. J Paediatr Child Health. 2017; 53(4):391–398. PMID: 28121046.30. Soliman N, Chaput K, Alshaikh B, Yusuf K. Preeclampsia and the risk of bronchopulmonary dysplasia in preterm infants less than 32 weeks’ gestation. Am J Perinatol. 2017; 34(6):585–592. PMID: 27919118.31. Kim DH, Shin SH, Kim EK, Kim HS. Association of increased cord blood soluble endoglin with the development of bronchopulmonary dysplasia in preterm infants with maternal preeclampsia. Pregnancy Hypertens. 2018; 13:148–153. PMID: 30177044.32. Lu CQ, Lin J, Yuan L, Zhou JG, Liang K, Zhong QH, et al. Pregnancy induced hypertension and outcomes in early and moderate preterm infants. Pregnancy Hypertens. 2018; 14:68–71. PMID: 30527121.33. Razak A, Patel W, Durrani N, McDonald SD, Vanniyasingam T, Thabane L, et al. Neonatal respiratory outcomes in pregnancy induced hypertension: introducing a novel index. J Matern Fetal Neonatal Med. 2020; 33(4):625–663. PMID: 30157682.34. Rocha G, de Lima FF, Machado AP, Guimarães H. Collaborators of the Hypertensive Disorders of Pregnancy Study Group. Preeclampsia predicts higher incidence of bronchopulmonary dysplasia. J Perinatol. 2018; 38(9):1165–1173. PMID: 29808003.35. Yusuf K, Alshaikh B, da Silva O, Lodha AK, Wilson RD, Alvaro RE, et al. Neonatal outcomes of extremely preterm infants exposed to maternal hypertension and cigarette smoking. J Perinatol. 2018; 38(8):1051–1059. PMID: 29740191.36. Tagliaferro T, Jain D, Vanbuskirk S, Bancalari E, Claure N. Maternal preeclampsia and respiratory outcomes in extremely premature infants. Pediatr Res. 2019; 85(5):693–696. PMID: 30770862.37. Wilmink FA, Reijnierse J, Reiss IK, Steegers EA, de Jonge RC. Research Consortium Neonatology South-West of the Netherlands. Preeclampsia and risk of developing bronchopulmonary dysplasia in very preterm neonates. Pregnancy Hypertens. 2019; 15:57–63. PMID: 30825928.38. Klinger G, Sokolover N, Boyko V, Sirota L, Lerner-Geva L, Reichman B, et al. Perinatal risk factors for bronchopulmonary dysplasia in a national cohort of very-low-birthweight infants. Am J Obstet Gynecol. 2013; 208(2):115.e1–115.e9. PMID: 23178245.39. Regev RH, Arnon S, Litmanovitz I, Bauer-Rusek S, Boyko V, Lerner-Geva L, et al. Outcome of singleton preterm small for gestational age infants born to mothers with pregnancy-induced hypertension. A population-based study. J Matern Fetal Neonatal Med. 2015; 28(6):666–673. PMID: 24871570.40. Davey DA, MacGillivray I. The classification and definition of the hypertensive disorders of pregnancy. Am J Obstet Gynecol. 1988; 158(4):892–898. PMID: 3364501.41. Jobe AH, Bancalari E. Bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001; 163(7):1723–1729. PMID: 11401896.42. Korhonen P, Tammela O, Koivisto AM, Laippala P, Ikonen S. Frequency and risk factors in bronchopulmonary dysplasia in a cohort of very low birth weight infants. Early Hum Dev. 1999; 54(3):245–258. PMID: 10321791.43. Hernández-Ronquillo L, Téllez-Zenteno JF, Weder-Cisneros N, Salinas-Ramírez V, Zapata-Pallagi JA, da Silva O. Risk factors for the development of bronchopulmonary dysplasia: a case-control study. Arch Med Res. 2004; 35(6):549–553. PMID: 15631883.44. Redline RW, Wilson-Costello D, Hack M. Placental and other perinatal risk factors for chronic lung disease in very low birth weight infants. Pediatr Res. 2002; 52(5):713–719. PMID: 12409518.45. Gortner L, Misselwitz B, Milligan D, Zeitlin J, Kollée L, Boerch K, et al. Rates of bronchopulmonary dysplasia in very preterm neonates in Europe: results from the MOSAIC cohort. Neonatology. 2011; 99(2):112–117. PMID: 20733331.46. Çetinkaya M, Çekmez F, Erener-Ercan T, Buyukkale G, Demirhan A, Aydemir G, et al. Maternal/neonatal vitamin D deficiency: a risk factor for bronchopulmonary dysplasia in preterms? J Perinatol. 2015; 35(10):813–817. PMID: 26226242.47. Anwar M, Ismat S, Qamber JH, Bano M. Bronchopulmonary dysplasia: a hazard factor in preterms due to maternal/neonatal vitamin D inadequacy. Pak J Med Health Sci. 2018; 12(3):1291–1295.48. Wells GA, Shea B, O'Connell D, Peterson J, Welch V, Losos M, et al. The Newcastle-Ottawa Scale (NOS) for assessing the quality of nonrandomised studies in meta-analyses. Accessed July 19, 2019. http://www.ohri.ca/programs/clinical_epidemiology/oxford.asp .49. Morrow LA, Wagner BD, Ingram DA, Poindexter BB, Schibler K, Cotten CM, et al. Antenatal determinants of bronchopulmonary dysplasia and late respiratory disease in preterm infants. Am J Respir Crit Care Med. 2017; 196(3):364–374. PMID: 28249118.50. Xu SZ, Hu XY, Zhao F, Zhou YX, Zhang SC. Effect of pregnancy-induced hypertension syndrome on complications in very low birth weight preterm infants. Zhongguo Dang Dai Er Ke Za Zhi. 2017; 19(4):402–404. PMID: 28407825.51. Mao X, Qiu J, Zhao L, Xu J, Yin J, Yang Y, et al. Vitamin D and IL-10 deficiency in preterm neonates with bronchopulmonary dysplasia. Front Pediatr. 2018; 6:246. PMID: 30246004.52. Mammaro A, Carrara S, Cavaliere A, Ermito S, Dinatale A, Pappalardo EM, et al. Hypertensive disorders of pregnancy. J Prenat Med. 2009; 3(1):1–5. PMID: 22439030.53. Hypertension in pregnancy. Report of the American College of Obstetricians and Gynecologists’ task force on hypertension in pregnancy. Obstet Gynecol. 2013; 122(5):1122–1131. PMID: 24150027.54. Gortner L, Wauer RR, Stock GJ, Reiter HL, Reiss I, Jorch G, et al. Neonatal outcome in small for gestational age infants: do they really better? J Perinat Med. 1999; 27(6):484–489. PMID: 10732308.55. Jobe A. The new BPD. Neoreviews. 2006; 7(10):e531–e545.56. Tang JR, Karumanchi SA, Seedorf G, Markham N, Abman SH. Excess soluble vascular endothelial growth factor receptor-1 in amniotic fluid impairs lung growth in rats: linking preeclampsia with bronchopulmonary dysplasia. Am J Physiol Lung Cell Mol Physiol. 2012; 302(1):L36–L46. PMID: 22003089.57. Tsao PN, Su YN, Li H, Huang PH, Chien CT, Lai YL, et al. Overexpression of placenta growth factor contributes to the pathogenesis of pulmonary emphysema. Am J Respir Crit Care Med. 2004; 169(4):505–511. PMID: 14644931.58. Bhatt AJ, Pryhuber GS, Huyck H, Watkins RH, Metlay LA, Maniscalco WM. Disrupted pulmonary vasculature and decreased vascular endothelial growth factor, Flt-1, and TIE-2 in human infants dying with bronchopulmonary dysplasia. Am J Respir Crit Care Med. 2001; 164(10 Pt 1):1971–1980. PMID: 11734454.59. Jakkula M, Le Cras TD, Gebb S, Hirth KP, Tuder RM, Voelkel NF, et al. Inhibition of angiogenesis decreases alveolarization in the developing rat lung. Am J Physiol Lung Cell Mol Physiol. 2000; 279(3):L600–L607. PMID: 10956636.60. Leaños-Miranda A, Navarro-Romero CS, Sillas-Pardo LJ, Ramírez-Valenzuela KL, Isordia-Salas I, Jiménez-Trejo LM. Soluble endoglin as a marker for preeclampsia, its severity, and the occurrence of adverse outcomes. Hypertension. 2019; 74(4):991–997. PMID: 31446801.61. Le Cras TD, Markham NE, Tuder RM, Voelkel NF, Abman SH. Treatment of newborn rats with a VEGF receptor inhibitor causes pulmonary hypertension and abnormal lung structure. Am J Physiol Lung Cell Mol Physiol. 2002; 283(3):L555–L562. PMID: 12169575.62. Abman SH, Groothius JR. Pathophysiology and treatment of bronchopulmonary dysplasia. Current issues. Pediatr Clin North Am. 1994; 41(2):277–315. PMID: 8139877.63. Palta M, Gabbert D, Weinstein MR, Peters ME. Multivariate assessment of traditional risk factors for chronic lung disease in very low birth weight neonates. The Newborn Lung Project. J Pediatr. 1991; 119(2):285–292. PMID: 1861218.64. Hakulinen A, Heinonen K, Jokela V, Kiekara O. Occurrence, predictive factors and associated morbidity of bronchopulmonary dysplasia in a preterm birth cohort. J Perinat Med. 1988; 16(5-6):437–446. PMID: 3241290.65. Shin SH, Shin SH, Kim SH, Kim YJ, Cho H, Kim EK, et al. The association of pregnancy-induced hypertension with bronchopulmonary dysplasia - a retrospective study based on the Korean Neonatal Network database. Sci Rep. 2020; 10(1):5600. PMID: 32221404.66. Walsh MC, Yao Q, Gettner P, Hale E, Collins M, Hensman A, et al. Impact of a physiologic definition on bronchopulmonary dysplasia rates. Pediatrics. 2004; 114(5):1305–1311. PMID: 15520112.67. Abman SH, Collaco JM, Shepherd EG, Keszler M, Cuevas-Guaman M, Welty SE, et al. Interdisciplinary care of children with severe bronchopulmonary dysplasia. J Pediatr. 2017; 181:12–28.e1. PMID: 27908648.68. Kim HR, Jung YH, Kim BI, Kim SY, Choi CW. Differences in comorbidities and clinical burden of severe bronchopulmonary dysplasia based on disease severity. Front Pediatr. 2021; 9:664033. PMID: 34277516.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparative study between pregnancies with and without hypertensive disorders in placental abruption
- Effect of maternal smoking during pregnancy on Tourette syndrome and chronic tic disorders among offspring: a systematic review and meta-analysis
- Systematic Review and Meta-analysis in Digestive Cancer Research
- Prenatal Maternal Risk Factors Contributing to Atopic Dermatitis: A Systematic Review and Meta-Analysis of Cohort Studies
- An Introduction of the Systematic Review and Meta-Analysis