Lab Med Online.
2021 Jul;11(3):183-190. 10.47429/lmo.2021.11.3.183.
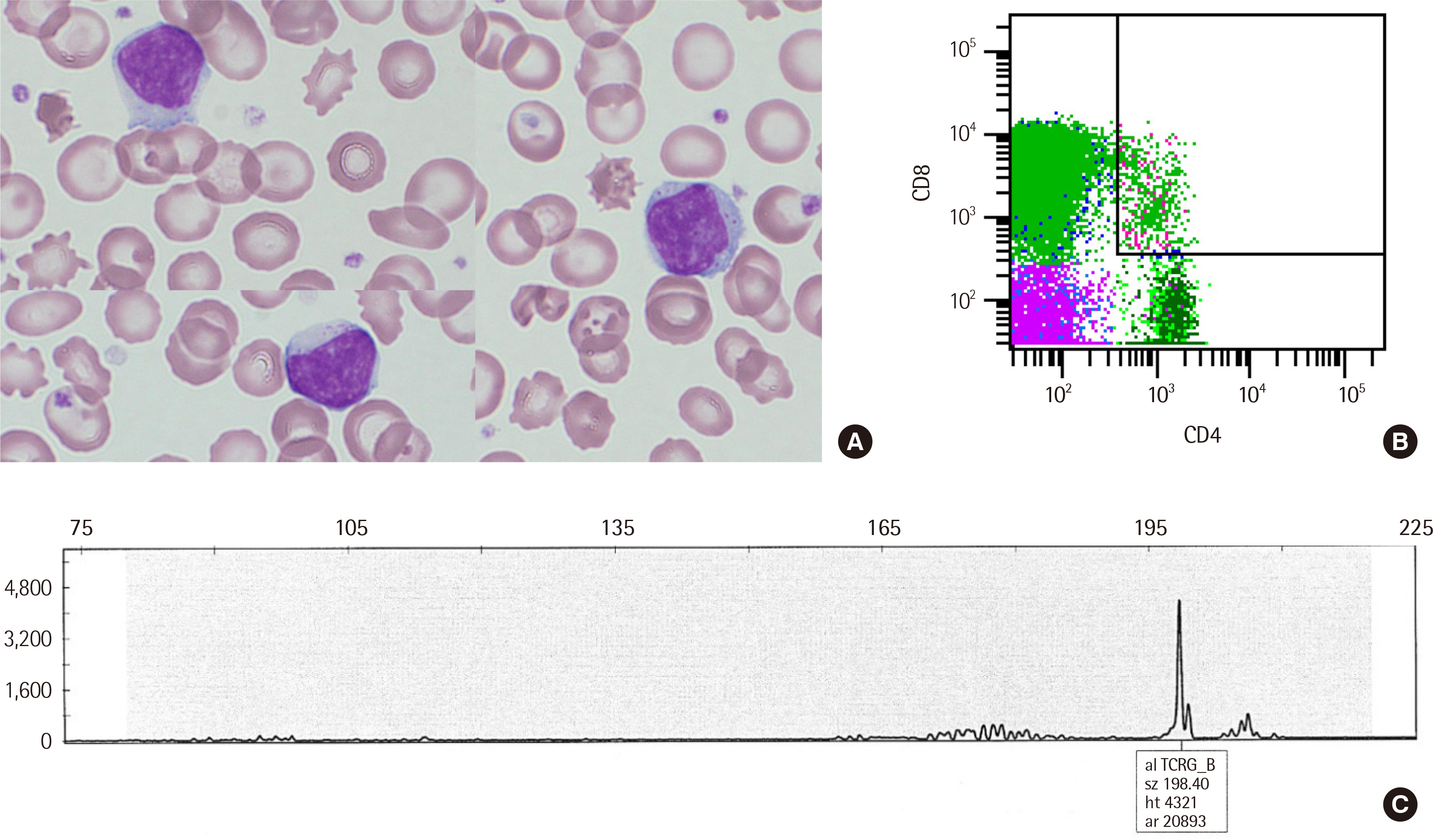
T-cell Large Granular Lymphocytic Leukemia Presenting as Post-transplant Lymphoproliferative Disorder: A Report of Two Cases and Literature Review
- Affiliations
-
- 1Department of Laboratory Medicine, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea
- KMID: 2526066
- DOI: http://doi.org/10.47429/lmo.2021.11.3.183
Abstract
- T-cell large granular lymphocytic leukemia (T-LGLL) can present as a form of post-transplant lymphoproliferative disorder. Here, we described clinicopathological findings from 58 cases of post-transplant T-LGLL (our own 2 cases and 56 cases from literature), and compared clinical features between solid organ transplantation (SOT) and allogeneic hematopoietic stem cell transplantation (alloHSCT) groups. The first of our two cases involved a 39-year-old man diagnosed with T-LGLL and cytomegalovirus (CMV) colitis 81.7 months post liver transplantation. He had underlying primary immunodeficiency, and a probable germline IKZF1 mutation. The second case involved a 51-year-old man with ALL diagnosed with T-LGLL 1.8 months post alloHSCT. The patient tested positive for CMV DNA and the disease was of donor origin. Both patients were alive at the last follow-up, although they had persistent lymphocytosis. Overall, the median duration for T-LGLL onset after transplantation was 43.2 months, and the median number of large granular lymphocytes was 2.5×109 /L. Nearly half of patients (46.0%) had CMV infection. Most patients (80.0%) of those whose clinical data were available showed good outcomes. The alloHSCT group showed significantly shorter latency (P < 0.001) and a trend for higher frequency of CMV positivity (P = 0.067) compared to the SOT group. Eleven patients (9 from the SOT and 2 from the alloHSCT group) showed autoimmune feature occurrence. This study reveals that CMV reactivation is a plausible driver for T-LGLL in the early phase after transplantation, and that the possibility of T-LGLL emergence should be considered, particularly for SOT patients with autoimmune features.
Keyword
Figure
Reference
-
1. Lamy T, Moignet A, Loughran TP Jr. 2017; LGL leukemia: from pathogenesis to treatment. Blood. 129:1082–94. DOI: 10.1182/blood-2016-08-692590. PMID: 28115367.
Article2. Herreman A, Dierickx D, Morscio J, Camps J, Bittoun E, Verhoef G, et al. 2013; Clinicopathological characteristics of posttransplant lymphoproliferative disorders of T-cell origin: single-center series of nine cases and meta-analysis of 147 reported cases. Leuk Lymphoma. 54:2190–9. DOI: 10.3109/10428194.2013.775436. PMID: 23402267.
Article3. Walter JE, Ayala IA, Milojevic D. 2019; Autoimmunity as a continuum in primary immunodeficiency. Curr Opin Pediatr. 31:851–62. DOI: 10.1097/MOP.0000000000000833. PMID: 31693597. PMCID: PMC6919226.
Article4. Hoshino A, Okada S, Yoshida K, Nishida N, Okuno Y, Ueno H, et al. 2017; Abnormal hematopoiesis and autoimmunity in human subjects with germline IKZF1 mutations. J Allergy Clin Immunol. 140:223–31. DOI: 10.1016/j.jaci.2016.09.029. PMID: 27939403.
Article5. Awada H, Mahfouz RZ, Durrani J, Kishtagari A, Jagadeesh D, Lichtin AE, et al. 2020; Large granular lymphocytic leukaemia after solid organ and haematopoietic stem cell transplantation. Br J Haematol. 189:318–22. DOI: 10.1111/bjh.16336. PMID: 31958160.
Article6. Alfano G, Fontana F, Colaci E, Mori G, Cerami C, Messerotti A, et al. 2019; T-cell large granular lymphocyte leukemia in solid organ transplant recipients: case series and review of the literature. Int J Hematol. 110:313–21. DOI: 10.1007/s12185-019-02682-2. PMID: 31250283.
Article7. Saeed OAM, Longe HO, Zhou J. 2018; T cell large granular lymphocytic leukemia, a rare form of post lung transplant lymphoproliferative disorder. Ann Hematol. 97:721–2. DOI: 10.1007/s00277-017-3213-5. PMID: 29313058.
Article8. Goyal T, Thakral B, Wang SA, Bueso-Ramos CE, Shi M, Jevremovic D, et al. 2018; T-cell large granular lymphocytic leukemia and coexisting B-cell lymphomas: a study from the bone marrow pathology group. Am J Clin Pathol. 149:164–71. DOI: 10.1093/ajcp/aqx146. PMID: 29365010.9. Ketterl TG, Wu D, Fromm JR, Soma L, Dahlberg AE, Wood BL, et al. 2018; Donor derived T-cell large granular lymphocyte leukemia after cord blood transplant for pediatric T-cell lymphoblastic leukemia. Bone Marrow Transplant. 53:352–5. DOI: 10.1038/s41409-017-0037-9. PMID: 29269802. PMCID: PMC5936635.
Article10. Hidalgo Lopez JE, Yabe M, Carballo-Zarate AA, Wang SA, Jorgensen JL, Ahmed S, et al. 2016; Donor-derived T-cell large granular lymphocytic leukemia in a patient with peripheral T-cell lymphoma. J Natl Compr Canc Netw. 14:939–44. DOI: 10.6004/jnccn.2016.0100. PMID: 27496109.
Article11. Muñoz-Ballester J, Chen-Liang TH, Hurtado AM, Heras I, de Arriba F, García-Malo MD, et al. 2016; Persistent cytotoxic T lymphocyte expansions after allogeneic haematopoietic stem cell transplantation: kinetics, clinical impact and absence of STAT3 mutations. Br J Haematol. 172:937–46. DOI: 10.1111/bjh.13917. PMID: 26728704.12. Yabe M, Medeiros LJ, Wang SA, Konoplev S, Ok CY, Loghavi S, et al. 2015; Clinicopathologic, immunophenotypic, cytogenetic, and molecular features of γδ t-cell large granular lymphocytic leukemia: an analysis of 14 patients suggests biologic differences with αβ T-cell large granular lymphocytic leukemia. Am J Clin Pathol. 144:607–19. DOI: 10.1309/AJCPJSA1E1YWSZEY. PMID: 26386082.
Article13. Kataria A, Cohen E, Saad E, Atallah E, Bresnahan B. 2014; Large granular lymphocytic leukemia presenting late after solid organ transplantation: a case series of four patients and review of the literature. Transplant Proc. 46:3278–81. DOI: 10.1016/j.transproceed.2014.05.083. PMID: 25240311.
Article14. Nann-Rütti S, Tzankov A, Cantoni N, Halter J, Heim D, Tsakiris D, et al. 2012; Large granular lymphocyte expansion after allogeneic hematopoietic stem cell transplant is associated with a cytomegalovirus reactivation and shows an indolent outcome. Biol Blood Marrow Transplant. 18:1765–70. DOI: 10.1016/j.bbmt.2012.07.007. PMID: 22796340.15. Gill H, Ip AH, Leung R, So JC, Pang AW, Tse E, et al. 2012; Indolent T-cell large granular lymphocyte leukaemia after haematopoietic SCT: a clinicopathologic and molecular analysis. Bone Marrow Transplant. 47:952–6. DOI: 10.1038/bmt.2011.212. PMID: 22041849.
Article16. Stamatopoulos K, Economidou D, Papadaki T, Vadikolia C, Papathanasiou M, Memmos D, et al. 2007; Large granular lymphocyte leukemia after renal transplantation: an immunologic, immunohistochemical, and genotypic study. Transplantation. 83:102–3. DOI: 10.1097/01.tp.0000239189.45186.74. PMID: 17220805.
Article17. Kusumoto S, Mori S, Nosaka K, Morita-Hoshi Y, Onishi Y, Kim SW, et al. 2007; T-cell large granular lymphocyte leukemia of donor origin after cord blood transplantation. Clin Lymphoma Myeloma. 7:475–9. DOI: 10.3816/CLM.2007.n.031. PMID: 17875238.
Article18. Chang H, Kamel-Reid S, Hussain N, Lipton J, Messner HA. 2005; T-cell large granular lymphocytic leukemia of donor origin occurring after allogeneic bone marrow transplantation for B-cell lymphoproliferative disorders. Am J Clin Pathol. 123:196–9. DOI: 10.1309/GLH5NVCFB9BKMV9G. PMID: 15842042.
Article19. Au WY, Lam CC, Lie AK, Pang A, Kwong YL. 2003; T-cell large granular lymphocyte leukemia of donor origin after allogeneic bone marrow transplantation. Am J Clin Pathol. 120:626–30. DOI: 10.1309/VA755A03PVRV9XDT.
Article20. Koskela HL, Eldfors S, Ellonen P, van Adrichem AJ, Kuusanmäki H, Andersson EI, et al. 2012; Somatic STAT3 mutations in large granular lymphocytic leukemia. N Engl J Med. 366:1905–13. DOI: 10.1056/NEJMoa1114885. PMID: 22591296. PMCID: PMC3693860.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- T-cell large granular lymphocytic leukemia: 4 cases
- T-cell Large Granular Lymphocytic Leukemia: A Case Report
- Cerebral Post-Transplant Lymphoproliferative Disorder Occurring after Renal Transplantation: A Case Report
- Leukemic Macrocheilitis Associated with Chronic Lymphocytic Leukemia
- T-large granular lymphocytic leukemia