Ann Hepatobiliary Pancreat Surg.
2021 May;25(2):307-312. 10.14701/ahbps.2021.25.2.307.
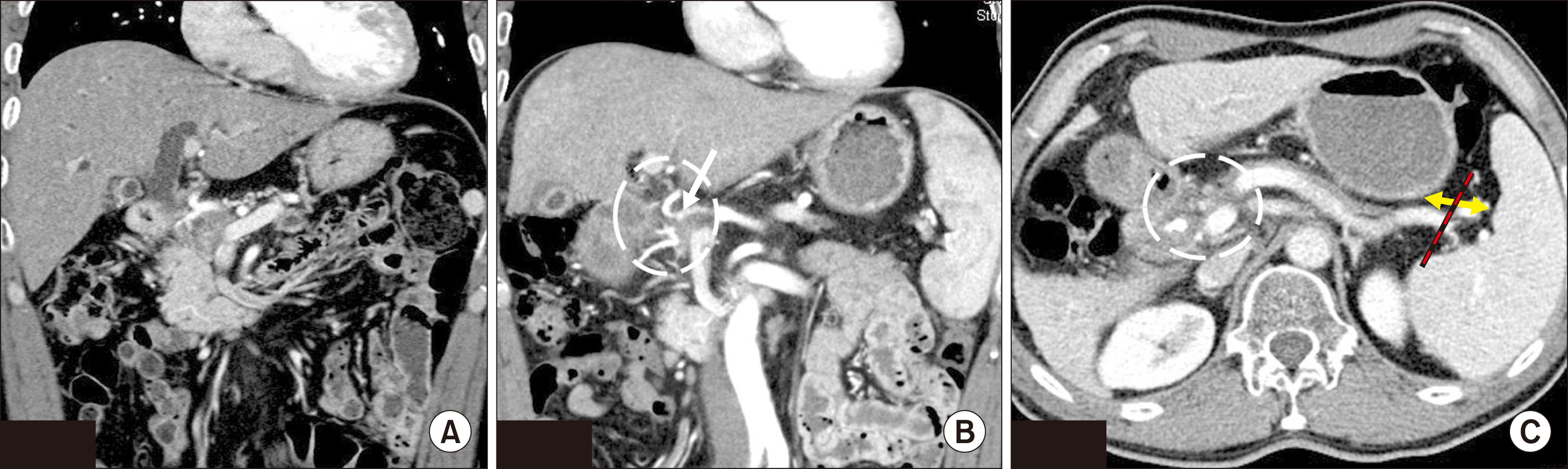
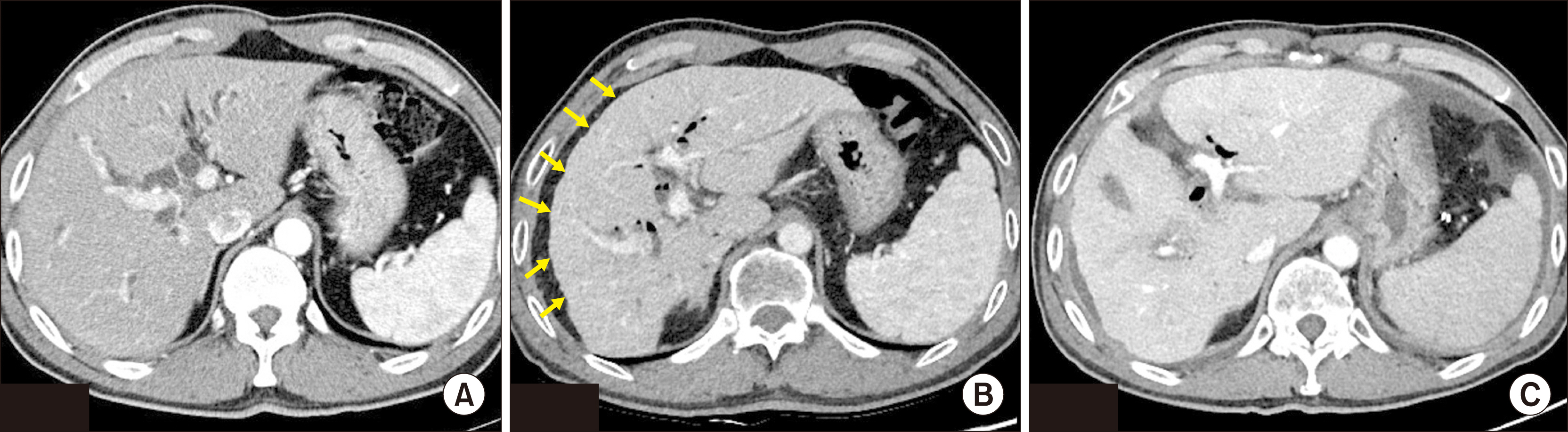
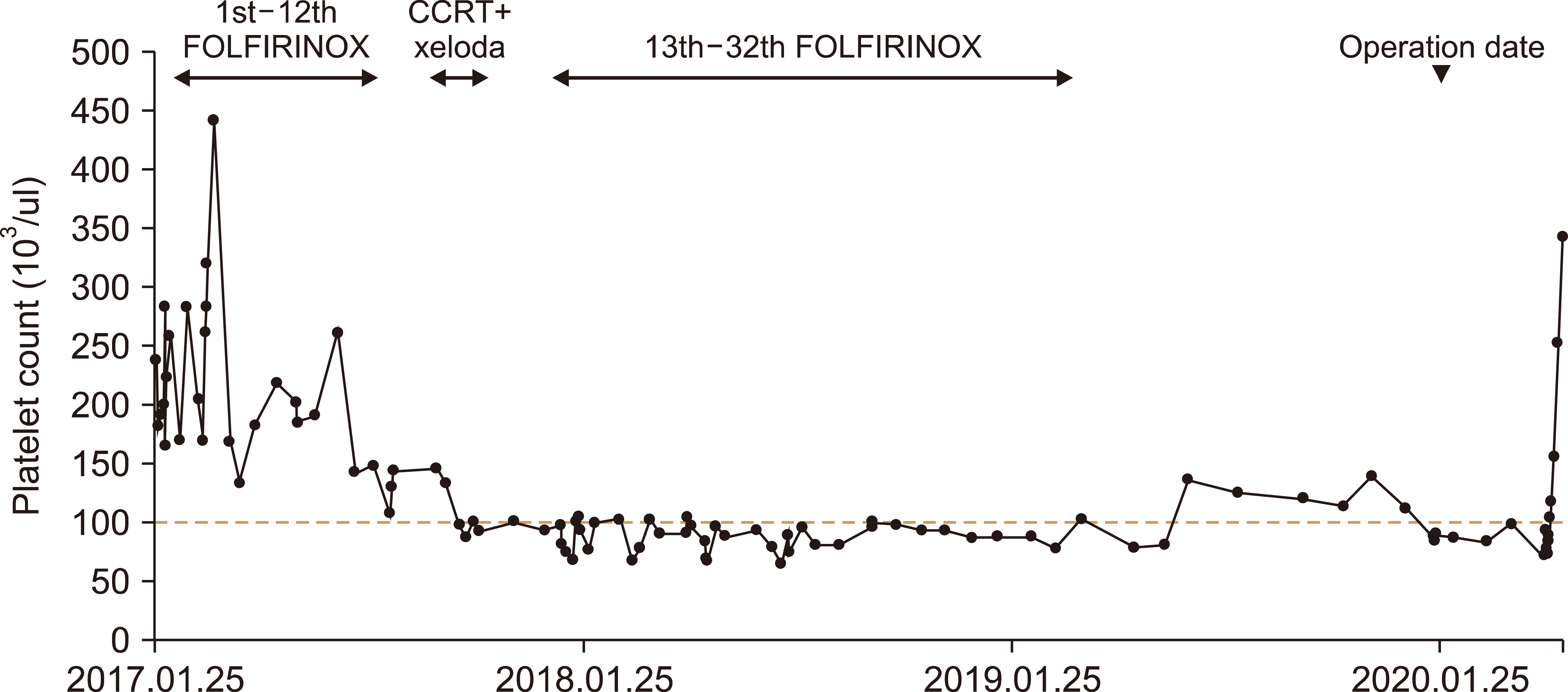
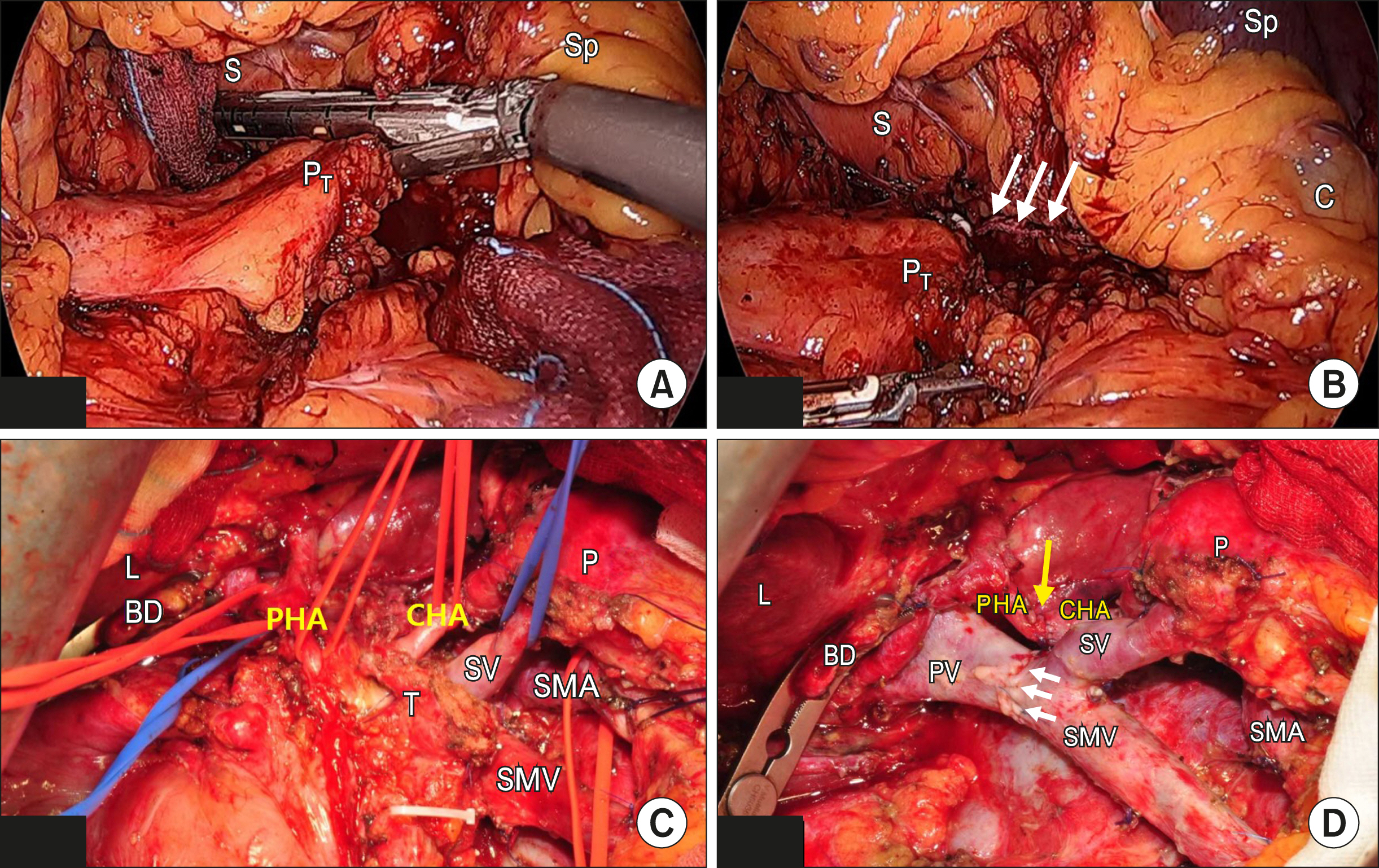
Pancreaticoduodenectomy with combined hepatic artery and portal vein resection after laparoscopic division of pancreaticosplenic ligament due to FOLFIRINOX-induced hepatic toxicity related secondary hypersplenism
- Affiliations
-
- 1Division of Hepatobiliary and Pancreatic Surgery, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- 2Division of Gastroenterology, Department of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- 3Division of Transplantation, Department of Surgery, Yonsei University College of Medicine, Seoul, Korea
- 4Pancreatobiliary Cancer Center, Yonsei Cancer Center, Severance Hospital, Seoul, Korea
- 5Department of Surgery, Yongin Severance, Yongin, Korea
- KMID: 2516500
- DOI: http://doi.org/10.14701/ahbps.2021.25.2.307
Abstract
- Pancreatic cancer is one of the dismal malignant disease in gastrointestinal tract. However, since the recent literature reporting median survival of FOLFIRINOX (leucovorin clcium, fluorouracil, irinotecan hydrochloride, oxaliplatin) chemotherapy was more than 12 months in metastatic pancreatic cancer was published, the positive attitude toward the treatment of the advanced pancreatic cancer is gradually expanded among the medical and surgical oncologists. Due to multiple combination of potent chemotherapeutic agents, potential adverse side effects should be concerned when considering FOLFIRINOX. Herein, we report a 55-year old male patient with locally advanced pancreatic cancer who successfully underwent curative resection following by laparoscopic division of pancreaticosplenic ligament due to long-term preoperative use of FOLFIRINOX related hepatic toxicity associated with secondary hypersplenism. The present case suggests the extended radical PD with combined major vascular resection following laparoscopic division of pancreaticosplenic ligament containing splenic artery and vein can improve the safety of curative resection and may expand the potential indication of pancreatic cancer in well-selected long-term use of preoperative FOLFIRINOX induced hepatic toxicity associated with secondary hypersplenism.
Figure
Reference
-
1. Conroy T, Desseigne F, Ychou M, Bouché O, Guimbaud R, Bécouarn Y, et al. 2011; FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N Engl J Med. 364:1817–1825. DOI: 10.1056/NEJMoa1011923. PMID: 21561347.
Article2. Sohal DP, Mangu PB, Khorana AA, Shah MA, Philip PA, O'Reilly EM, et al. 2016; Metastatic pancreatic cancer: American Society of Clinical Oncology clinical practice guideline. J Clin Oncol. 34:2784–2796. DOI: 10.1200/JCO.2016.67.1412. PMID: 27247222. PMCID: PMC5019760.
Article3. Conroy T, Hammel P, Hebbar M, Ben Abdelghani M, Wei AC, Raoul JL, et al. 2018; FOLFIRINOX or gemcitabine as adjuvant therapy for pancreatic cancer. N Engl J Med. 379:2395–2406. DOI: 10.1056/NEJMoa1809775. PMID: 30575490.
Article4. Stein SM, James ES, Deng Y, Cong X, Kortmansky JS, Li J, et al. 2016; Final analysis of a phase II study of modified FOLFIRINOX in locally advanced and metastatic pancreatic cancer. Br J Cancer. 114:737–743. DOI: 10.1038/bjc.2016.45. PMID: 27022826. PMCID: PMC4984865.
Article5. Clancy TE. 2015; Surgery for pancreatic cancer. Hematol Oncol Clin North Am. 29:701–716. DOI: 10.1016/j.hoc.2015.04.001. PMID: 26226905.
Article6. Janssen QP, Buettner S, Suker M, Beumer BR, Addeo P, Bachellier P, et al. 2019; Neoadjuvant FOLFIRINOX in patients with borderline resectable pancreatic cancer: a systematic review and patient-level meta-analysis. J Natl Cancer Inst. 111:782–794. DOI: 10.1093/jnci/djz073. PMID: 31086963. PMCID: PMC6695305.
Article7. Boone BA, Steve J, Krasinskas AM, Zureikat AH, Lembersky BC, Gibson MK, et al. 2013; Outcomes with FOLFIRINOX for borderline resectable and locally unresectable pancreatic cancer. J Surg Oncol. 108:236–241. DOI: 10.1002/jso.23392. PMID: 23955427. PMCID: PMC3816713.
Article8. Seo AN, Kim H. 2014; Sinusoidal obstruction syndrome after oxaliplatin-based chemotherapy. Clin Mol Hepatol. 20:81–84. DOI: 10.3350/cmh.2014.20.1.81. PMID: 24757663. PMCID: PMC3992335.
Article9. El Chediak A, Haydar AA, Hakim A, Massih SA, Hilal L, Mukherji D, et al. 2018; Increase in spleen volume as a predictor of oxaliplatin toxicity. Ther Clin Risk Manag. 14:653–657. DOI: 10.2147/TCRM.S150968. PMID: 29695909. PMCID: PMC5905497.
Article10. Pei Y, Chai S, Zhang Y, Zhang Z, Chen X, Zhang W. 2019; Benefits of splenectomy and curative treatments for patients with hepatocellular carcinoma and portal hypertension: a retrospective study. J Gastrointest Surg. 23:2151–2162. DOI: 10.1007/s11605-018-3981-9. PMID: 30511133. PMCID: PMC6831533.
Article11. Wang Q, Dang T, Meng X, Li K, Ren W, Ma X, et al. 2019; Is concomitant splenectomy necessary in radical gastric cancer surgery? A systematic review and meta-analysis. Asia Pac J Clin Oncol. 15:e28–e35. DOI: 10.1111/ajco.13052. PMID: 30178572.
Article12. Yamamoto N, Okano K, Oshima M, Akamoto S, Fujiwara M, Tani J, et al. 2015; Laparoscopic splenectomy for patients with liver cirrhosis: improvement of liver function in patients with Child-Pugh class B. Surgery. 158:1538–1544. DOI: 10.1016/j.surg.2015.05.008. PMID: 26070848.13. Shoup M, Brennan MF, McWhite K, Leung DH, Klimstra D, Conlon KC. 2002; The value of splenic preservation with distal pancreatectomy. Arch Surg. 137:164–168. DOI: 10.1001/archsurg.137.2.164. PMID: 11822953.
Article14. Dalla Bona E, Beltrame V, Liessi F, Sperti C. 2012; Fatal pneumococcal sepsis eleven years after distal pancreatectomy with splenectomy for pancreatic cancer. JOP. 13:693–695. DOI: 10.1155/2012/951358. PMID: 23197988. PMCID: PMC3502873.15. Hwang HK, Kang CM, Lee SH, Murakami T, Kiyuna T, Kim SH, et al. 2018; Fluorescence-guided surgery with splenic preservation prevents tumor recurrence in an orthotopic nude-mouse model of human pancreatic cancer. Anticancer Res. 38:665–670. DOI: 10.21873/anticanres.12270.
Article16. Stefanidis D, Grove KD, Schwesinger WH, Thomas CR Jr. 2006; The current role of staging laparoscopy for adenocarcinoma of the pancreas: a review. Ann Oncol. 17:189–199. DOI: 10.1093/annonc/mdj013. PMID: 16236756.
Article17. Pandit S, Samant H, Kohli K, Shokouh-Amiri HM, Wellman G, Zibari GB. 2019; Incidental liver metastasis in pancreatic adenocar-cinoma. J Surg Case Rep. 2019:rjz084. DOI: 10.1093/jscr/rjz084.
Article18. Wang L, Wu D, Cheng YG, Xu JW, Chu HB, Zhang GY, et al. 2019; Warshaw technique in laparoscopic spleen-preserving distal pancreatectomy: surgical strategy and late outcomes of splenic preservation. Biomed Res Int. 2019:4074369. DOI: 10.1155/2019/4074369. PMID: 31317027. PMCID: PMC6601470.
Article19. Suzumura K, Hatano E, Okada T, Fujimoto J. 2017; Perioperative and long-term outcome of the Warshaw technique in laparoscopic spleen-preserving distal pancreatectomy. Surg Laparosc Endosc Percutan Tech. 27:474–478. DOI: 10.1097/SLE.0000000000000484. PMID: 29016391.
Article20. Kawaguchi K, Motoi F, Yokoyama S, Takemura S, Doi T, Nozawa Y, et al. 2013; [A case of curatively resected locally advanced pancreatic cancer with combined resection of the portal vein and common hepatic artery after neoadjuvant chemotherapy]. Gan To Kagaku Ryoho. 40:1875–1877. Japanese.21. Delpero JR, Sauvanet A. 2020; Vascular resection for pancreatic cancer: 2019 French recommendations based on a literature review from 2008 to 6-2019. Front Oncol. 10:40. DOI: 10.3389/fonc.2020.00040. PMID: 32117714. PMCID: PMC7010716.
Article22. Oba A, Bao QR, Barnett CC, Al-Musawi MH, Croce C, Schulick RD, et al. 2020; Vascular resections for pancreatic ductal adenocarci-noma: vascular resections for PDAC. Scand J Surg. 109:18–28. DOI: 10.1177/1457496919900413. PMID: 31960765.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Spontaneous hepatic arterioportal fistula in extrahepatic portal vein obstruction: Combined endovascular and surgical management
- Hepatic artery pseudoaneurysm after pancreaticoduodenectomy treated with coil embolization in combination with portomesenteric venous stenting
- Successful laparoscopic living donor right hepatectomy in a case with challenging portal vein variation
- A Case of Hepatic Artery-Portal Vein Fistula
- Ultrasonographic Measurement of the Diameter of a Normal Bile Duct, Hepatic Artery and Portal Vein in Infants Younger Than 3 Months