Ann Pediatr Endocrinol Metab.
2020 Dec;25(4):217-226. 10.6065/apem.2040090.045.
Insulin resistance and type 2 diabetes in children
- Affiliations
-
- 1Department of Pediatrics, University of Chieti, Chieti, Italy
- KMID: 2510892
- DOI: http://doi.org/10.6065/apem.2040090.045
Abstract
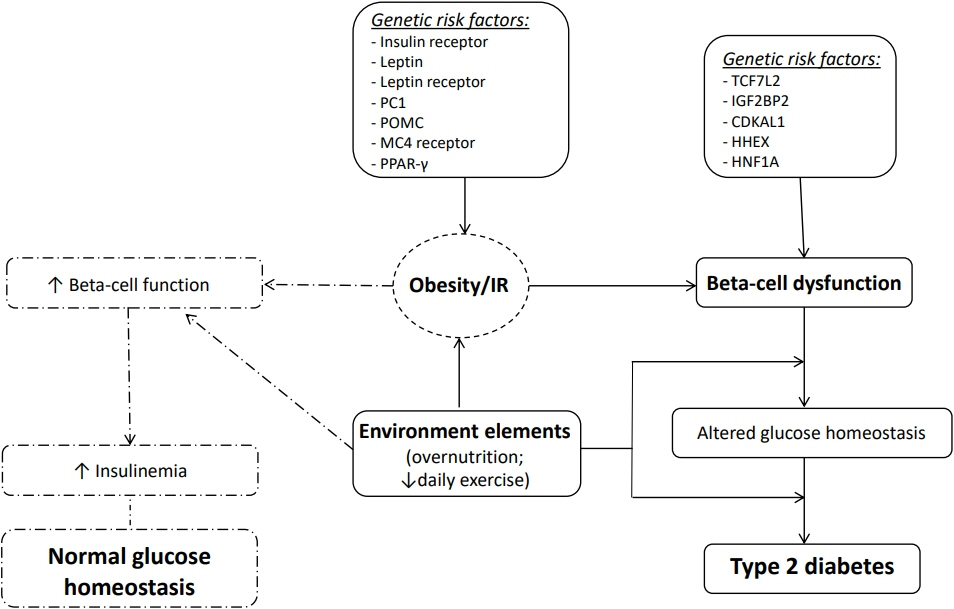
- Type 2 diabetes (T2D) is an emerging health risk in obese children and adolescents. Both environmental (lack of physical activity, excess nutritional intake, sedentary lifestyle) and genetic factors contribute to this global epidemic. The growing prevalence of T2D in youth is also associated with a consistently increased incidence of metabolic and cardiovascular complications. Insulin resistance (IR), i.e., whole-body decreased glucose uptake in response to physiological insulin levels, determines impaired glucose homeostasis and it is recognized as cardinal trigger of T2D and cardiovascular disease in both adults and children. In particular, IR and beta-cell dysfunction lead to the persistent hyperglycemia which characterizes T2D. Indeed, both pathological states influence each other and presumably play a crucial, synergistic role in the pathogenesis of T2D, although the precise mechanisms are not completely understood. However, beta-cell dysfunction and IR induce impaired glucose metabolism, thus leading to the progression to T2D. Therefore, understanding the mechanisms correlated with the decline of beta-cell function and IR is crucial in order to control, prevent, and treat T2D in youth. This review focuses on the current knowledge regarding IR and T2D in children and adolescents and showcases interesting opportunities and stimulating challenges for the development of new preventative approaches and therapeutic strategies for young patients with T2D.
Keyword
Figure
Cited by 3 articles
-
Diagnostic and Therapeutic Strategies of Type 2 Diabetes Mellitus in Youth
Hwa Young Kim, Jae Hyun Kim
Ewha Med J. 2022;45(3):e3. doi: 10.12771/emj.2022.e3.Screening and Management for Dyslipidemia in Korean Children and Adolescents
Jong Seo Yoon, Il Tae Hwang
Ewha Med J. 2022;45(3):e4. doi: 10.12771/emj.2022.e4.Commentary on "Ambient air pollution and endocrinologic disorders in childhood"
Hyun Wook Chae
Ann Pediatr Endocrinol Metab. 2021;26(3):135-135. doi: 10.6065/apem.2121066edi01.
Reference
-
References
1. Reaven GM. Insulin resistance:the link between obesity and cardiovascular disease. Endocrinol Metab Clin North Am. 2008; 37:581–601.2. Razani B, Chakravarthy MV, Semenkovich CF. Insulin resistance and atherosclerosis. Endocrinol Metab Clin North Am. 2008; 37:603–21.
Article3. Chiarelli F, Marcovecchio ML. Insulin resistance and obesity in childhood. Eur J Endocrinol. 2008; 159:67–74.
Article4. Volovelsky O, Weiss R. Fatty liver disease in obese children relation to other metabolic risk factors. Int J Pediatric Obes. 2011; 6:59–64.
Article5. Levy-Marchal C, Arslanian S, Cutfield W, Sinaiko A, Druet C, Marcovecchio ML, et al. Insulin resistance in children: consensus, perspective, and future directions. J Clin Endocrinol Metabol. 2010; 95:5189–98.
Article6. Ferrannini E. Insulin resistance is central to the burden of diabetes. Diab Metab Rev. 1997; 13:81–6.
Article7. Giannini C, Caprio S. Islet function in obese adolescents. Diab Obes Metabo. 2012; 14:40–5.
Article8. Lawrence JM, Imperatore G, Dabelea D, Mayer-Davis EJ, Linder B, Saydah S, et al. Trends in incidence of type 1 diabetes among non-Hispanic white youth in the U.S., 2002–2009. Diabetes. 2014; 63:3938–45.
Article9. Dabelea D, Mayer-Davis EJ, Saydah S. Prevalence of type 1 and type 2 diabetes among children and adolescents from 2001 to 2009. JAMA. 2014; 311:1778–86.
Article10. Liu LL, Lawrence JM, Davis C, Liese AD, Pettitt DJ, Pihoker C, et al. Prevalence of overweight and obesity in youth with diabetes in USA: the SEARCH for Diabetes in Youth study. Pediatr Diabetes. 2010; 11:4–11.
Article11. Candler TP, Mahmoud O, Lynn RM, Majbar AA, Barrett TG, Shield JP. Continuing rise of type 2 diabetes incidence in children and young people in the UK. Diabet Med. 2018; 35:737–44.12. Schober E, Waldhoer T, Rami B, Hofer S. Austrian Diabetes Incidence Study Group: incidence and time trend of type 1 and type 2 diabetes in Austrian children 1999-2007. J Pediatr. 2009; 155:190–3.13. Lee JH, Kim YM, Kwak MJ, Kim SY, Kim HJ, Cheon CK. Incidence trends and associated factors of diabetes mellitus in Korean children and adolescents: a retrospective cohort study in Busan and Gyeongnam. Ann Pediatr Endocrinol Metab. 2015; 20:206–12.
Article14. Ye Q, Fu JF. Paediatric type 2 diabetes in China-Pandemic, progression, and potential solutions. Pediatr Diabetes. 2018; 19:27–35.
Article15. Sjardin N, Reed P, Albert B, Mouat F, Carter PJ, Hofman P, et al. Increasing incidence of type 2 diabetes in New Zealand children <15 years of age in a regional-based diabetes service, Auckland, New Zealand. J Paediatr Child Health. 2018; 54:1005–10.
Article16. Imperatore G, Boyle JP, Thompson TJ, Case D, Dabelea D, Hamman RF, et al. Projections of type 1 and type 2 diabetes burden in the U.S. population aged, 20 years through 2050: dynamic modeling of incidence, mortality, and population growth. Diabetes Care. 2012; 35:2515–20.17. Pettitt DJ, Talton J, Dabelea D, Divers J, Imperatore G, Lawrence JM, et al. Prevalence of diabetes in U.S. youth in 2009: the SEARCH for diabetes in youth study. Diabetes Care. 2014; 37:402–8.
Article18. Amed S, Dean HJ, Panagiotopoulos C, S ellers EA, Hadjiyannakis S, Laubscher TA, et al. Type 2 diabetes, medication induced diabetes, and monogenic diabetes in Canadian children: a prospective national surveillance study. Diabetes Care. 2010; 33:786–91.19. Haines L, Wan KC, Lynn R, Barrett TG, Shield JP. Rising incidence of type 2 diabetes in children in the U.K. Diabetes Care. 2007; 30:1097–101.
Article20. Pavkov ME, Hanson RL, Knowler WC, Bennett PH, Krakoff J, Nelson RG. Changing patterns of type 2 diabetes incidence among Pima Indians. Diabetes Care. 2007; 30:1758–63.
Article21. Arslanian S, Bacha F, Grey M, Marcus MD, White NH, Zeitler P. Evaluation and management of youth-onset type 2 diabetes: a position statement by the American Diabetes Association. Diabetes Care. 2018; 41:2648–68.
Article22. Zeitler P, Hirs K, Pyle L, Linder B, Copeland K, Arslanian S, et al. A clinical trial to maintain glycemic control in youth with type 2 diabetes. N Engl J Med. 2012; 366:2247–56.
Article23. Todd JN, Srinivasan S, Pollin TI. Advances in the genetics of youth-onset type 2 diabetes. Curr Diab Rep. 2018; 18:57.
Article24. Ashcroft FM, Rorsman P. Diabetes mellitus and the beta cell:the last ten years. Cell. 2012; 148:1160–71.25. Dupuis J, Langenberg C, Prokopenko I, Saxena R, Soranzo N, Jackson AU, et al. New genetic loci implicated in fasting glucose homeostasis and their impact on type 2 diabetes risk. Nat Genet. 2010; 42:105–16.26. B arker A, Shar p SJ, Timps on NJ, B ouatia-Naji N, Warrington NM, Kanoni S, et al. Association of genetic Loci with glucose levels in childhood and adolescence:a meta-analysis of over 6,000 children. Diabetes. 2011; 60:1805–12.27. Giannini C, Dalla Man C, Groop L, Cobelli C, Zhao H, Shaw MM, et al. Co-occurrence of risk alleles in or near genes modulating insulin secretion predisposes obese youth to prediabetes. Diabetes Care. 2014; 37:475–82.
Article28. Cropano C, Santoro N, Groop L, Dalla Man C, Cobelli C, Galderisi A, et al. The rs7903146 variant in the TCF7L2 gene increases the risk of prediabetes/type 2 diabetes in obese adolescents by impairing β-cell function and hepatic insulin sensitivity. Diabetes Care. 2017; 40:1082–9.29. Kahn SE, Prigeon RL, McCulloch DK, Boyko EJ, Bergman RN, Schwartz MW, et al. Quantification of the relationship between insulin sensitivity and beta-cell function in human subjects. Evidence for a hyperbolic function. Diabetes. 1993; 42:1663–72.
Article30. Bacha F, Lee S, Gungor N, Arslanian SA. From pre-diabetes to type 2 diabetes in obese youth:pathophysiological characteristics along the spectrum of glucose dysregulation. Diabetes Care. 2010; 33:2225–31.31. Bacha F, Gungor N, Lee S, Arslanian SA. In vivo insulin sensitivity and secretion in obese youth: what are the differences between normal glucose tolerance, impaired glucose tolerance, and type 2 diabetes? Diabetes Care. 2009; 32:100–5.32. Giannini C, Weiss R, Cali A, Bonadonna R, Santoro N, Pierpont B, et al. Evidence for early defects in insulin sensitivity and secretion before the onset of glucose dysregulation in obese youths: a longitudinal study. Diabetes. 2012; 61:606–14.33. Cnop M, Welsh N, Jonas JC, Jorns A, Lenzen S, Eizirik DL. Mechanisms of pancreatic beta-cell death in type 1 and type 2 diabetes: many differences, few similarities. Diabetes. 2005; 54:S97–107.34. Lenzen S. Oxidative stress: the vulnerable beta-cell. Biochem Soc Trans. 2008; 36:343–7.35. Arslanian SA, Bacha F, Saad R, Gungor N. Family history of type 2 diabetes is associated with decreased insulin sensitivity and an impaired balance between insulin sensitivity and insulin secretion in white youth. Diabetes Care. 2005; 28:115–9.
Article36. Ball GD, Huang TT, Gower BA, Cruz ML, Shaibi GQ, Weigensberg MJ, et al. Longitudinal changes in insulin sensitivity, insulin secretion, and beta-cell function during puberty. J Pediatr. 2006; 148:16–22.
Article37. Copeland KC, Zeitler P, Geffner M, Guandalini C, Higgins J, Hirst K, et al. Characteristics of adolescents and youth with recent-onset type 2 diabetes:the TODAY cohort at baseline. J Clin Endocrinol Metab. 2011; 96:159–67.38. Chernausek SD, Arslanian S, Caprio S, Copeland KC, El ghormli L, Kelsey MM, et al. Relationship between parental diabetes and presentation of metabolic and glycemic function in youth with type 2 diabetes: baseline findings from the TODAY trial. Diabetes Care. 2016; 39:110–7.
Article39. Dabelea D, Mayer-Davis EJ, Lamichhane AP, D'Agostino RB Jr, Liese AD, Vehik KS, et al. Association of intrauterine exposure to maternal diabetes and obesity with type 2 diabetes in youth: the SEARCH Case-Control Study. Diabetes Care. 2008; 31:1422–6.40. American Diabetes Association. Children and adolescent: standards of medical care in Diabetes-2020. Diabetes Care. 2020; 43:S163–82.41. Czech MP. Insulin action and resistance in obesity and type 2 diabetes. Nat Med. 2017; 11;23:804–14.
Article42. Boucher J, Kleinridders A, Kahn CR. Insulin receptor signaling in normal and insulin-resistant states. Cold Spring Harb Perspect Biol. 2014; 6:a009191.
Article43. Choi SM, Tucker DF, Gross DN, Easton RM, DiPilato LM, Dean AS, et al. Insulin regulates adipocyte lipolysis via an Akt-independent signaling pathway. Mol Cell Biol. 2010; 30:5009–20.
Article44. Kahn BB, Flier JS. Obesity and insulin resistance. J Clin Investig. 2000; 106:473–81.
Article45. Matt haei S, Stumvol l M, Kel lerer M, Haring HU. Pathophysiology and pharmacological treatment of insulin resistance. Endocr Rev. 2000; 21:585–618.
Article46. Kahn SE, Hull RL, Utzschneider KM. Mechanisms linking obesity to insulin resistance and type 2 diabetes. Nature. 2006; 444:840–6.
Article47. Bonora E. Insulin resistance as an independent risk factor for cardiovascular disease: clinical assessment and therapy approaches. Av Diabetol. 2005; 21:255–61.48. DeFronzo RA, Tobin JD, Andres R. Glucose clamp technique: a method for quantifying insulin secretion and resistance. Am J Physiol. 1979; 237:214–23.
Article49. Muniyappa R, Lee S, Chen H, Quon MJ. Current approaches for assessing insulin sensitivity and resistance in vivo: advantages, limitations, and appropriate usage. Am J Physiol Endocrinol Metab. 2008; 294:15–26.
Article50. Arslanian SA. Clamp techniques in paediatrics: what have we learned? Horm Res. 2005; 64:16–24.
Article51. van der Aa MP, Knibbe CA, Boer A, van der Vorst MM. Definition of insulin resistance affects prevalence rate in pediatric patients:a systematic review and call for consensus. J Pediatr Endocrinol Metab. 2017; 30:123–31.52. Gutch M, Kumar S, Razi SM, Gupta KK, Gupta A. Assessment of insulin sensitivity/resistance. Indian J Endocrinol Metab. 2015; 19:160–4.
Article53. Hwu CM. Me asurements of insulin resistance in hypertension: where are we now? J Human Hypertens. 2007; 21:693–6.54. Lee S, Muniyappa R, Yan X, Chen H, Yue LQ, Hong EG, et al. Comparison between surrogate indexes of insulin sensitivity and resistance and hyperinsulinemic euglycemic clamp estimates in mice. Am J Physiol Endocrinol Metab. 2008; 294:261–70.
Article55. Rasmussen-Torvik LJ, Pankow JS, Jacobs DR, Steffen LM, Moran AM, Steinberger J, et al. Heritability and genetic correlations of insulin sensitivity measured by the euglycaemic clam. Diabet Med. 2007; 24:1286–9.56. Keskin M, Kurtoglu S, Kendirci M, Atabek ME, Yazici C. Homeostasis model assessment is more reliable than the fasting glucose/insulin ratio and quantitative insulin sensitivity check index for assessing insulin resistance among obese children and adolescents. Pediatrics. 2005; 115:500–3.
Article57. Cutfield WS, Jefferies CA, Jackson WE, Robinson EM, Hofman PL. Evaluation of HOMA and QUICKI as measures of insulin sensitivity in prepubertal children. Pediatr Diabetes. 2003; 4:119–25.
Article58. Wallace TM, Matthews DR. The assessment of insulin resistance in man. Diabet Med. 2002; 19:527–34.
Article59. Gungor N, Saad R, Janosky J, Arslanian S. Validation of surro gate est imates of insu lin s ensit iv ity and insulin secretion in children and adolescents. J Pediatr. 2004; 144:47–55.
Article60. Giannini C, Santoro N, Caprio S, Kim G, Lartaud D, Shaw M, et al. The triglyceride-to-HDL cholesterol ratio:association with insulin resistance in obese youths of different ethnic backgrounds. Diabetes Care. 2011; 34:1869–74.61. McAuley KA, Williams SM, Mann JI, Walker RJ, Lewis-Barned NJ, Temple LA, et al. Diagnosing insulin resistance in the general population. Diabetes Care. 2001; 24:460–4.
Article62. Jayagopal V, Kilpatrick ES, Jennings PE, Holding S, Hepburn DA, Atkin SL, et al. the biological variation of sex hormonebinding globulin in type 2 diabetes: implications for sex hormone-binding globulin as a surrogate marker of insulin resistance. Diabetes Care. 2004; 27:278–80.63. Monzillo LU, Hamdy O. Evaluation of insulin sensitivity in clinical practice and in research settings. Nutr Rev. 2003; 61:397–412.
Article64. Matsuda M, DeFronzo RA. Insulin sensitivity indices obtained from oral glucose tolerance testing: comparison with the euglycemic insulin clamp. Diabetes Care. 1999; 22:1462–70.
Article65. Cederholm J, Wibell L. Insulin release and peripheral sensitivity at the oral glucose tolerance test. Diab Res Clin Pract. 1990; 10:167–75.
Article66. Rossner SM, Neovius M, Mattsson A, Marcus C, Norgren S. HOMA-IR and QUICKI: decide on a general standard instead of making further comparisons. Acta Paediatr. 2010; 99:1735–40.
Article67. Rivera P, Martos-Moreno GA, Barrios V, Suárez J, Pavón FJ, Chowen JA, et al. A novel approach to childhood obesity: circulating chemokines and growth factors as biomarkers of insulin resistance. Pediatric Obesity. 2019; 14:12473.
Article68. Xu H, Barnes GT, Yang Q, Tan G, Yang D, Chou CJ, et al. Chronic inflammation in fat plays a crucial role in the development of obesity-related insulin resistance. J Clin Invest. 2003; 112:1821–30.
Article69. Ignacio RM, Gibbs CR, Lee ES, Son DS. Differential chemokine signature between human preadipocytes and adipocytes. Immune Netw. 2016; 16:189–94.
Article70. da Silva CC, Zambon MP, Vasques AC, Camilo DF, De Bernardi Rodrigues AM, Antonio MÂRGM, et al. Homeostatic model assessment of adiponectin (HOMAAdiponectin) as a surrogate measure of insulin resistance in adolescents: comparison with the hyperglycaemic clamp and homeostatic model assessment of insulin resistance. PLoS One. 2019; 14:e0214081.
Article71. Yadav A, Kataria MA, Saini V, Yadav A. Role of leptin and adiponectin in insulin resistance. Clin Chim Acta. 2013; 417:80–4.
Article72. Lee S, Bacha F, Gungor N, Arslanian SA. Racial differences in adiponectin in youth: relationship to visceral fat and insulin sensitivity. Diabetes Care. 2006; 29:51–6.73. Weiss R, Dufour S, Groszmann A, Petersen K, Dziura J, Taksali SE, et al. Low adiponectin levels in adolescent obesity: a marker of increased intramyocellular lipid accumulation. J Clin Endocrinol Metab. 2003; 88:2014–8.
Article74. Vieira-Ribeiro SA, Fonseca PC, Andreoli CS, Ribeiro AQ, Herms- dorff HH, Pereira PF, et al. The TyG index cutoff point and its association with body adiposity and lifestyle in children. J Pediatr. 2019; 95:217–23.
Article75. Guerrero-Romero F, Villalobos-Molina R, Simental-Mendía LE, Méndez-Cruz R, MurguíaRomero M, et al. Fasting triglycerides and glucose index as a diagnostic test for insulin resistance in young adults. Arch Med Res. 2016; 47:382–7.
Article76. Kang B, Yang Y, Lee EY, Yang HK, Kim HS, Lim SY, et al. Triglycerides/glucose index is a useful surrogate marker of insulin resistance among adolescents. Int J Obes. 2017; 41:789–92.
Article77. Moon S, Park JS, Ahn Y. The cut-off values of triglycerides and glucose index for metabolic syndrome in American and Korean adolescents. J Korean Med Sci. 2017; 32:427–33.
Article78. Cerf ME. Beta cell dysfunction and insulin resistance. Front Endocrinol (Lausanne). 2013; 4:37.
Article79. Ono H. Molecular mechanisms of hypothalamic insulin resistance. Int J Mol Sci. 2019; 15:1317.
Article80. Chiasson JL, Rabasa-Lhoret R. Prevention of type 2 diabetes: insulin resistance and beta-cell function. Diabetes. 2004; 53:S34. –8.81. Shanik MH, Xu Y, Skrha J, Dankner R, Zick Y, Roth J. Insulin resistance and hyperinsulinemia: is hyperinsulinemia the cart or the horse? Diabetes Care. 2008; 31:S262–8.82. Parker VE, Savage DB, O’Rahilly S, Semple RK. Mechanistic insights into insulin resistance in the genetic era. Diabet Med. 2011; 28:1476–86.
Article83. Klotz LO, Sánchez-Ramos C, Prieto-Arroyo I, Urbánek P, Steinbrenner H, Monsalve M, et al. Redox regulation of FoxO transcription factors. Redox Biol. 2015; 6:51–72.
Article84. Ryder JW, Gilbert M, Zierath JR. Skeletal muscle and insulin sensitivity: pathophysiological alterations. Front Biosci. 2001; 6:D154–63.
Article85. Gross DN, van den Heuvel AP, Birnbaum MJ. The role of FoxO in the regulation of metabolism. Oncogene. 2008; 27:2320–36.
Article86. Titchenell PM, Quinn WJ, Lu M, Chu Q, Lu W, Li C, et al. Direct hepatocyte insulin signaling is required for lipogenesis but is dispensable for the suppression of glucose production. Cell Metab. 2016; 23:1154–66.
Article87. Banks AS, Kim-Muller JY, Mastracci TL, Kofler NM, Qiang L, Haeusler RA, et al. Dissociation of the glucose and lipid regulatory functions of FoxO1 by targeted knockin of acetylation-defective alleles in mice. Cell Metab. 2011; 14:587–97.
Article88. Corkey BE. Banting lecture 2011: hyperinsulinemia: cause or consequence? Diabetes. 2012; 61:4–13.89. Corkey BE. Diabetes: have we got it all wrong? Insulin hypersecretion and food additives: cause of obesity and diabetes? Diabetes Care. 2012; 35:2432–7.90. Kim MK, Reaven GM, Chen YD, Kim E, Kim SH. Hyperinsulinemia in individuals with obesity: role of insulin clearance. Obesity (Silver Spring). 2015; 23:2430–4.
Article91. Agrawal NK, Kant S. Targeting inflammation in diabetes: newer therapeutic options. World J Diabetes. 2014; 5:697–710.
Article92. Wang X, Bao W, Liu J, Ouyang YY, Wang D, Rong S, et al. Inflammatory markers and risk of type 2 diabetes: a systematic review and meta-analysis. Diabetes Care. 2013; 36:166–75.93. Reinehr T. Inflammator y markers in children and adolescents with type 2 diabetes mellitus. Clin Chim Acta. 2019; 496:100–7.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Using Motivational Interviewing to Overcome Psychological Insulin Resistance
- Glut4 in the insulin resistance of NIDDM
- Insulin Resistance and Insulin Resistance Syndrome
- Psychological Insulin Resistance: Key Factors and Intervention
- Letter: Effects of Aerobic Exercise Intensity on Insulin Resistance in Patients with Type 2 Diabetes Mellitus (Korean Diabetes J 33(5):401-411, 2009)