Korean J Gastroenterol.
2020 Jul;76(1):9-16. 10.4166/kjg.2020.76.1.9.
Endoscopic and Endosonographic Features of Histologically Proven Gastric Ectopic Pancreas by Endoscopic Resection
- Affiliations
-
- 1Division of Gastroenterology, Department of Internal Medicine, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- 2Department of Pathology, Chonnam National University Hospital, Chonnam National University Medical School, Gwangju, Korea
- KMID: 2504555
- DOI: http://doi.org/10.4166/kjg.2020.76.1.9
Abstract
- Background/Aims
Distinguishing gastric ectopic pancreas (GEP) from malignant tumors is relatively difficult. This study evaluated the endosonography findings of pathologically proven GEP.
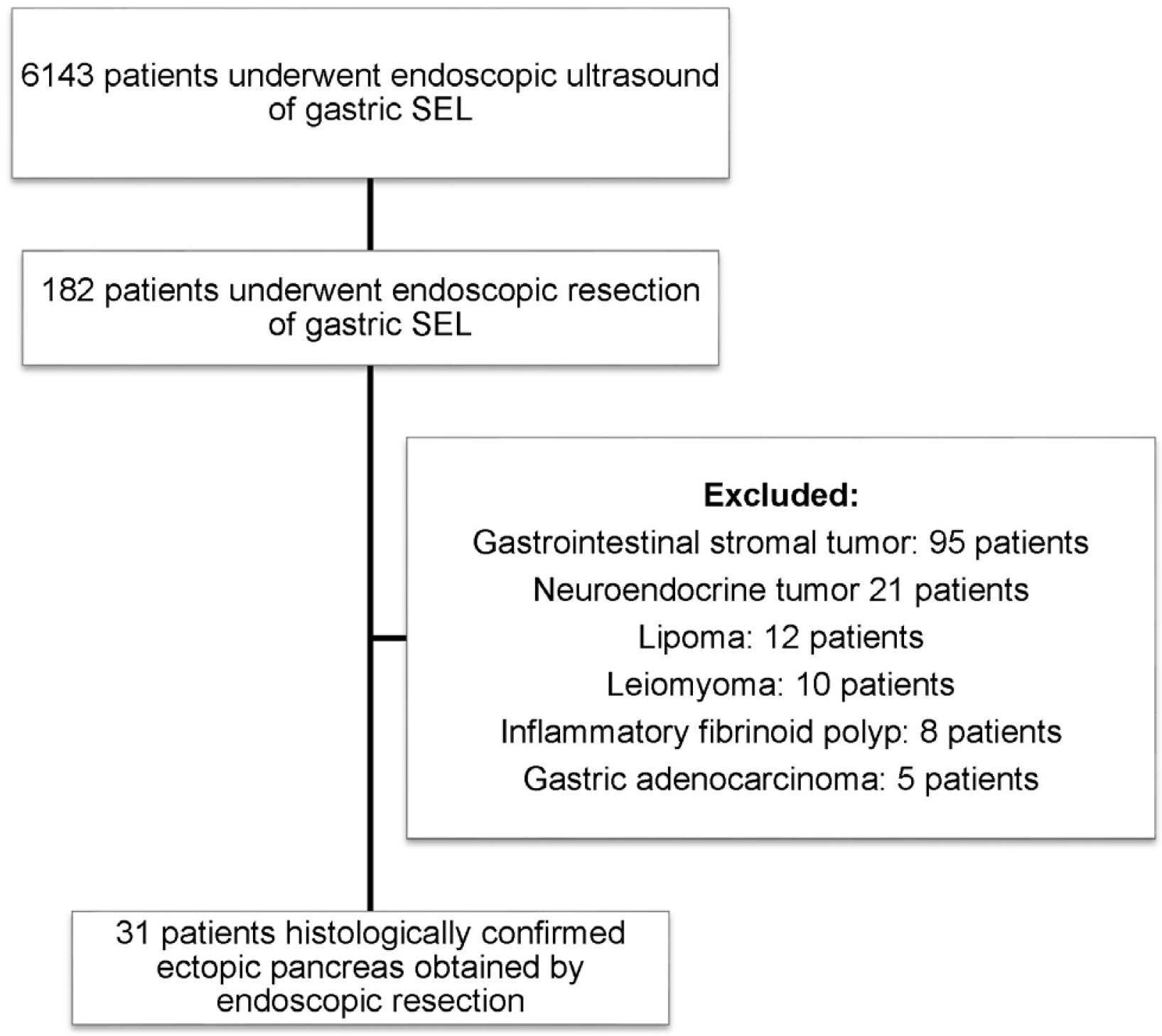
Methods
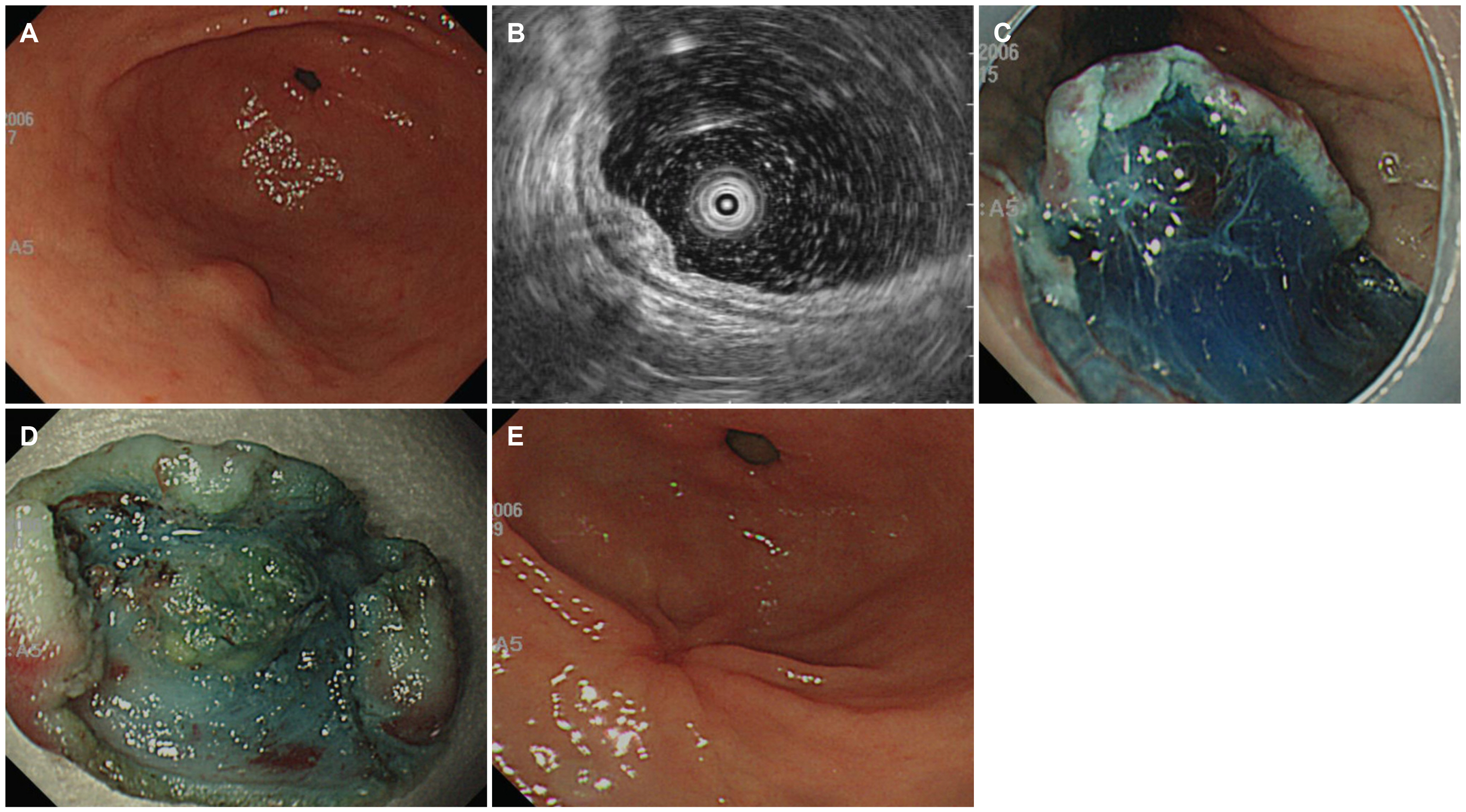
Thirty-one patients diagnosed with GEP based on a histopathological analysis from January 2004 to July 2018 were enrolled in this study. All patients underwent EUS and an endoscopic resection.
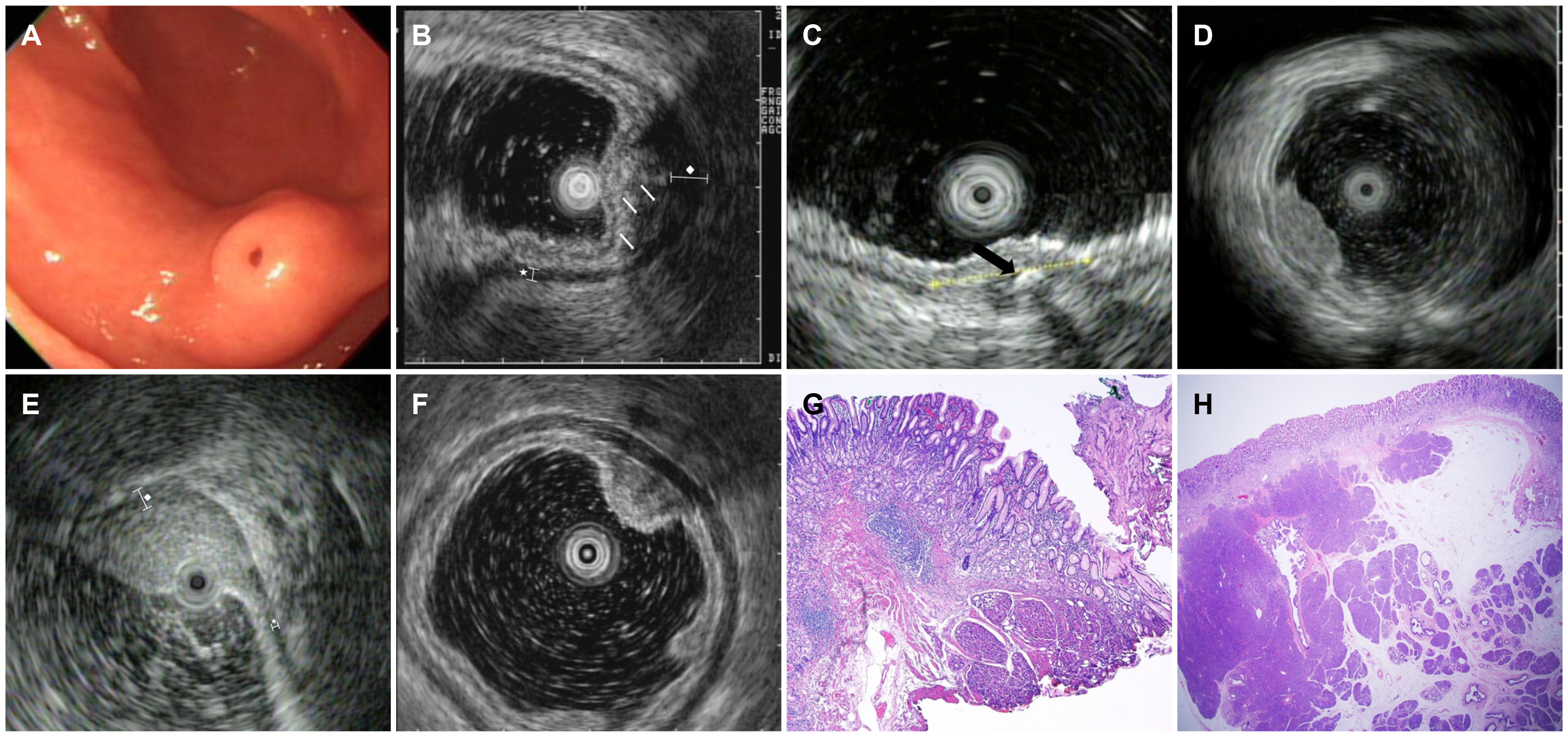
Results
Seventeen patients were female, and the median age was 41.1 years (range, 14-74). The lesions were localized most commonly in the antrum. The mean size of the GEP was 10.6 mm (range, 7-15). Superficial type lesions, lesions with heterogeneous echogenicity, mixed pattern lesions, and lesions with indistinct borders were commonly observed on EUS. Calcification, anechoic duct-like structures, and thickening of the muscularis propria were observed in some patients. Endoscopic mucosal resection (41.9%) and endoscopic submucosal dissection (58.1%) were performed. The mean procedure time was 22.5 minutes. Complete resection was achieved for 71% of patients. No statistically significant results between the endosonography findings and complete resection rates were obtained. The mean follow-up esophagogastroduodenoscopy duration was 4.5 months. None of the patients presented with residual lesions on subsequent endoscopy.
Conclusions
EUS can help identify the features of GEP. Careful observations of the EUS findings can avoid unnecessary removal of GEP.
Figure
Reference
-
1. Lucena JF, Alvarez OA, Gross GW. 1997; Endoscopic resection of heterotopic pancreas of the minor duodenal papilla: case report and review of the literature. Gastrointest Endosc. 46:69–72. DOI: 10.1016/S0016-5107(97)70214-1. PMID: 9260710.
Article2. Slidell MB, Schmidt EF, Jha RC, et al. 2009; Solid pseudopapillary tumor in a pancreatic rest of the jejunum. J Pediatr Surg. 44:E25–E27. DOI: 10.1016/j.jpedsurg.2009.01.074. PMID: 19361620.
Article3. Lemaire J, Delaunoit T, Molle G. 2014; Adenocarcinoma arising in gastric heterotopic pancreas. Case report and review of the literature. Acta Chir Belg. 114:79–81. DOI: 10.1080/00015458.2014.11680983. PMID: 24720145.
Article4. Park SH, Kim GH, Park DY, et al. 2011; Endosonographic findings of gastric ectopic pancreas: a single center experience. J Gastroenterol Hepatol. 26:1441–1446. DOI: 10.1111/j.1440-1746.2011.06764.x. PMID: 21557771.
Article5. Yüksel M, Kacar S, Akpinar MY, et al. 2017; Endosonogragphic features of lesions suggesting gastricectopic pancreas: experience of a single tertiary center. Turk J Med Sci. 47:313–317. DOI: 10.3906/sag-1602-181. PMID: 28263508.
Article6. Kim JH, Lim JS, Lee YC, et al. 2008; Endosonographic features of gastric ectopic pancreases distinguishable from mesenchymal tumors. J Gastroenterol Hepatol. 23:e301–e307. DOI: 10.1111/j.1440-1746.2008.05351.x. PMID: 18522684.
Article7. Ryu DY, Kim GH, Park DY, et al. 2010; Endoscopic removal of gastric ectopic pancreas: an initial experience with endoscopic submucosal dissection. World J Gastroenterol. 16:4589–4593. DOI: 10.3748/wjg.v16.i36.4589. PMID: 20857531. PMCID: PMC2945492.
Article8. Shim CS, Jung IS. 2005; Endoscopic removal of submucosal tumors:preprocedure diagnosis, technical options, and results. Endoscopy. 37:646–654. DOI: 10.1055/s-2005-861477. PMID: 16010609.9. Attwell A, Sams S, Fukami N. 2015; Diagnosis of ectopic pancreas by endoscopic ultrasound with fine-needle aspiration. World J Gastroenterol. 21:2367–2373. DOI: 10.3748/wjg.v21.i8.2367. PMID: 25741143. PMCID: PMC4342912.
Article10. Hebrok M, Kim SK, St Jacques B, McMahon AP, Melton DA. 2000; Regulation of pancreas development by hedgehog signaling. Development. 127:4905–4913. PMID: 11044404.
Article11. Yamada T, Ichikawa H. 1974; X-ray diagnosis of elevated lesions of the stomach. Radiology. 110:79–83. DOI: 10.1148/110.1.79. PMID: 4808543.
Article12. Chou JW, Cheng KS, Ting CF, et al. 2014; Endosonographic features of histologically proven gastric ectopic pancreas. Gastroenterol Res Pract. 2014:160601. DOI: 10.1155/2014/160601. PMID: 25371670. PMCID: PMC4209789.
Article13. Gress F, Schmitt C, Savides T, et al. 2001; Interobserver agreement for EUS in the evaluation and diagnosis of submucosal masses. Gastrointest Endosc. 53:71–76. DOI: 10.1067/mge.2001.111384. PMID: 11154492.
Article14. Gottschalk U, Dietrich CF, Jenssen C. 2018; Ectopic pancreas in the upper gastrointestinal tract: is endosonographic diagnosis reliable? Data from the German Endoscopic Ultrasound Registry and review of the literature. Endosc Ultrasound. 7:270–278. DOI: 10.4103/eus.eus_18_17. PMID: 28836514. PMCID: PMC6106155.
Article15. Matsushita M, Hajiro K, Okazaki K, Takakuwa H. 1999; Gastric aberrant pancreas: EUS analysis in comparison with the histology. Gastrointest Endosc. 49:493–497. DOI: 10.1016/S0016-5107(99)70049-0. PMID: 10202065.
Article16. Hase S, Nakazawa S, Yoshino J, et al. 1989; A study on gastric and small intestinal aberrant pancreas by endoscopic ultrasonography--with special reference to comparison with histological appearance. Nihon Shokakibyo Gakkai Zasshi. 86:1684–1691. PMID: 2685422.17. Kida M, Kawaguchi Y, Miyata E, et al. 2017; Endoscopic ultrasonography diagnosis of subepithelial lesions. Dig Endosc. 29:431–443. DOI: 10.1111/den.12854. PMID: 28258621.
Article18. Yoshida T, Sakamoto A, Kuroki K, Kojo A, Watanabe H. 1976; Electrocoagulation biopsy of aberrant pancreas of the stomach. A case of aberrant gastric pancreas. Am J Gastroenterol. 66:554–558. PMID: 1020743.19. Kojima T, Takahashi H, Parra-Blanco A, Kohsen K, Fujita R. 1999; Diagnosis of submucosal tumor of the upper GI tract by endoscopic resection. Gastrointest Endosc. 50:516–522. DOI: 10.1016/S0016-5107(99)70075-1. PMID: 10502173.
Article20. Lai EC, Tompkins RK. 1986; Heterotopic pancreas. Review of a 26 year experience. Am J Surg. 151:697–700. DOI: 10.1016/0002-9610(86)90045-0. PMID: 3717502.21. Ormarsson OT, Gudmundsdottir I, Mårvik R. 2006; Diagnosis and treatment of gastric heterotopic pancreas. World J Surg. 30:1682–1689. DOI: 10.1007/s00268-005-0669-6. PMID: 16902740.
Article22. Khashab MA, Cummings OW, DeWitt JM. 2009; Ligation-assisted endoscopic mucosal resection of gastric heterotopic pancreas. World J Gastroenterol. 15:2805–2808. DOI: 10.3748/wjg.15.2805. PMID: 19522034. PMCID: PMC2695899.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Endoscopic Findings of Ectopic Pancreas in the Stomach
- Advancements in Endoscopic Treatment for Gastric Subepithelial Tumors
- A case of asymptomatic gastric ectopic pancreas associated with elevated serum CA 19-9
- Acute Ectopic Pancreatitis Occurring after Endoscopic Biopsy in a Gastric Ectopic Pancreas
- Endoscopic Treatment for Gastric Subepithelial Tumor