Clin Endosc.
2014 Sep;47(5):455-459. 10.5946/ce.2014.47.5.455.
Acute Ectopic Pancreatitis Occurring after Endoscopic Biopsy in a Gastric Ectopic Pancreas
- Affiliations
-
- 1Department of Internal Medicine, Pusan National University School of Medicine, Busan, Korea. doc0224@pusan.ac.kr
- 2Department of Pathology, Pusan National University School of Medicine, Busan, Korea.
- KMID: 2165380
- DOI: http://doi.org/10.5946/ce.2014.47.5.455
Abstract
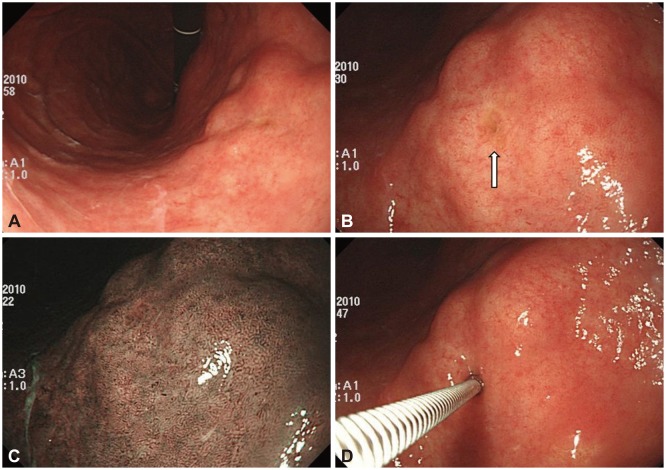
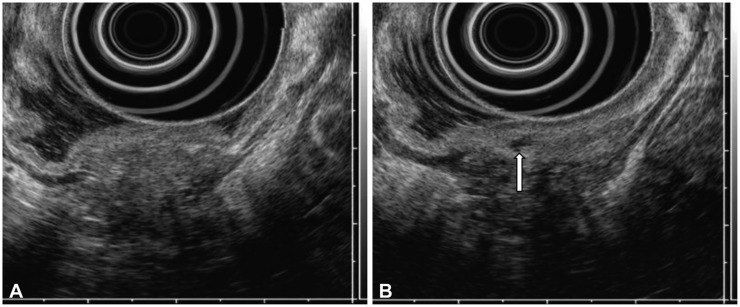
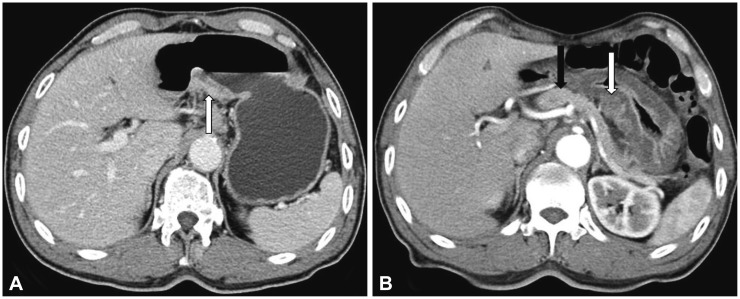
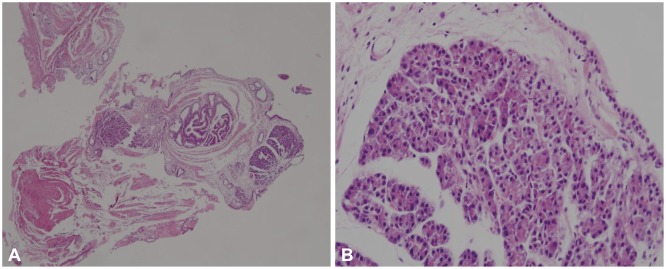
- Ectopic pancreas is a congenital anomaly and the most common type of ectopic tissue in the gastrointestinal tract. Most patients with an ectopic pancreas are asymptomatic and rarely have complications. Ectopic pancreatitis after an endoscopic biopsy has not been reported. We report a patient who developed acute ectopic pancreatitis in the stomach after an endoscopic biopsy. A 71-year-old male patient presented with a subepithelial tumor (SET) in the stomach and had no symptoms. Endoscopic ultrasonography demonstrated a 30-mm hypoechoic mural mass, lobulated margins, and anechoic duct-like lesions. To obtain proper tissue specimen, endoscopic biopsy was performed through the opening on the surface of the mass. The pathologic results confirmed an ectopic pancreas. One day after the endoscopic biopsy, he developed persistent epigastric pain. His serum amylase and lipase elevated. Computed tomography of the abdomen showed swelling of the SET and diffuse edema of the gastric wall. His condition was diagnosed as acute ectopic pancreatitis occurring after endoscopic biopsy.
Keyword
MeSH Terms
Figure
Reference
-
1. Hsu SD, Wu HS, Kuo CL, Lee YT. Robotic-assisted laparoscopic resection of ectopic pancreas in the posterior wall of gastric high body: case report and review of the literature. World J Gastroenterol. 2005; 11:7694–7696. PMID: 16437703.
Article2. Lai EC, Tompkins RK. Heterotopic pancreas. Review of a 26 year experience. Am J Surg. 1986; 151:697–700. PMID: 3717502.3. Osanai M, Miyokawa N, Tamaki T, Yonekawa M, Kawamura A, Sawada N. Adenocarcinoma arising in gastric heterotopic pancreas: clinicopathological and immunohistochemical study with genetic analysis of a case. Pathol Int. 2001; 51:549–554. PMID: 11472568.
Article4. Tanaka K, Tsunoda T, Eto T, et al. Diagnosis and management of heterotopic pancreas. Int Surg. 1993; 78:32–35. PMID: 8473080.5. Kaneda M, Yano T, Yamamoto T, et al. Ectopic pancreas in the stomach presenting as an inflammatory abdominal mass. Am J Gastroenterol. 1989; 84:663–666. PMID: 2729238.6. Chen SH, Huang WH, Feng CL, et al. Clinical analysis of ectopic pancreas with endoscopic ultrasonography: an experience in a medical center. J Gastrointest Surg. 2008; 12:877–881. PMID: 18246404.
Article7. Park SH, Kim GH, Park do Y, et al. Endosonographic findings of gastric ectopic pancreas: a single center experience. J Gastroenterol Hepatol. 2011; 26:1441–1446. PMID: 21557771.
Article8. Kim JH, Lim JS, Lee YC, et al. Endosonographic features of gastric ectopic pancreases distinguishable from mesenchymal tumors. J Gastroenterol Hepatol. 2008; 23(8 Pt 2):e301–e307. PMID: 18522684.
Article9. Armstrong CP, King PM, Dixon JM, Macleod IB. The clinical significance of heterotopic pancreas in the gastrointestinal tract. Br J Surg. 1981; 68:384–387. PMID: 7237066.
Article10. Mulholland KC, Wallace WD, Epanomeritakis E, Hall SR. Pseudocyst formation in gastric ectopic pancreas. JOP. 2004; 5:498–501. PMID: 15536290.11. Polkowski M, Butruk E. Submucosal lesions. Gastrointest Endosc Clin N Am. 2005; 15:33–54. PMID: 15555950.
Article12. Emerson L, Layfield LJ, Rohr LR, Dayton MT. Adenocarcinoma arising in association with gastric heterotopic pancreas: a case report and review of the literature. J Surg Oncol. 2004; 87:53–57. PMID: 15221920.
Article13. Kwon MS, Lee SS, Ahn GH. Schwannomas of the gastrointestinal tract: clinicopathological features of 12 cases including a case of esophageal tumor compared with those of gastrointestinal stromal tumors and leiomyomas of the gastrointestinal tract. Pathol Res Pract. 2002; 198:605–613. PMID: 12440783.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- A case of asymptomatic gastric ectopic pancreas associated with elevated serum CA 19-9
- Gastric Outlet Obstruction Caused by Gastric Ectopic Pancreas With Pseudocyst Formation
- A Case of Gastric Ectopic Pancreas Complicated by Chronic Pancreatitis
- Duodenal ectopic pancreas complicated by chronic pancreatitis and pseudocyst formation: a case report
- A Case of Gastric Ectopic Pancreas Complicated by Pancreatitis and Pseudocyst Formation