Ann Rehabil Med.
2020 Jun;44(3):181-194. 10.5535/arm.19087.
Usefulness of Goal Attainment Scaling in Intensive Stroke Rehabilitation During the Subacute Stage
- Affiliations
-
- 1Department of Rehabilitation Medicine, CHA Bundang Medical Center, CHA University College of Medicine, Seongnam, Korea
- KMID: 2504438
- DOI: http://doi.org/10.5535/arm.19087
Abstract
Objective
To investigate the usefulness of goal attainment scaling (GAS) in intensive stroke rehabilitation during the subacute stage.
Methods
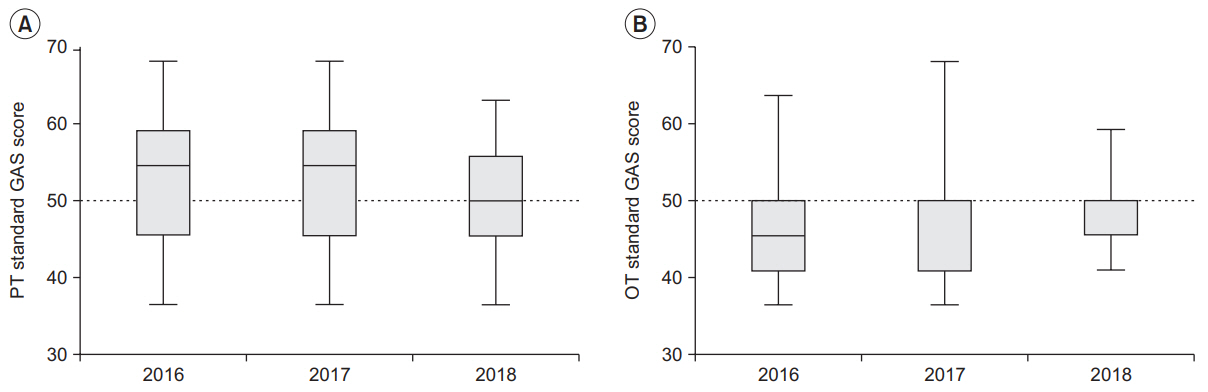
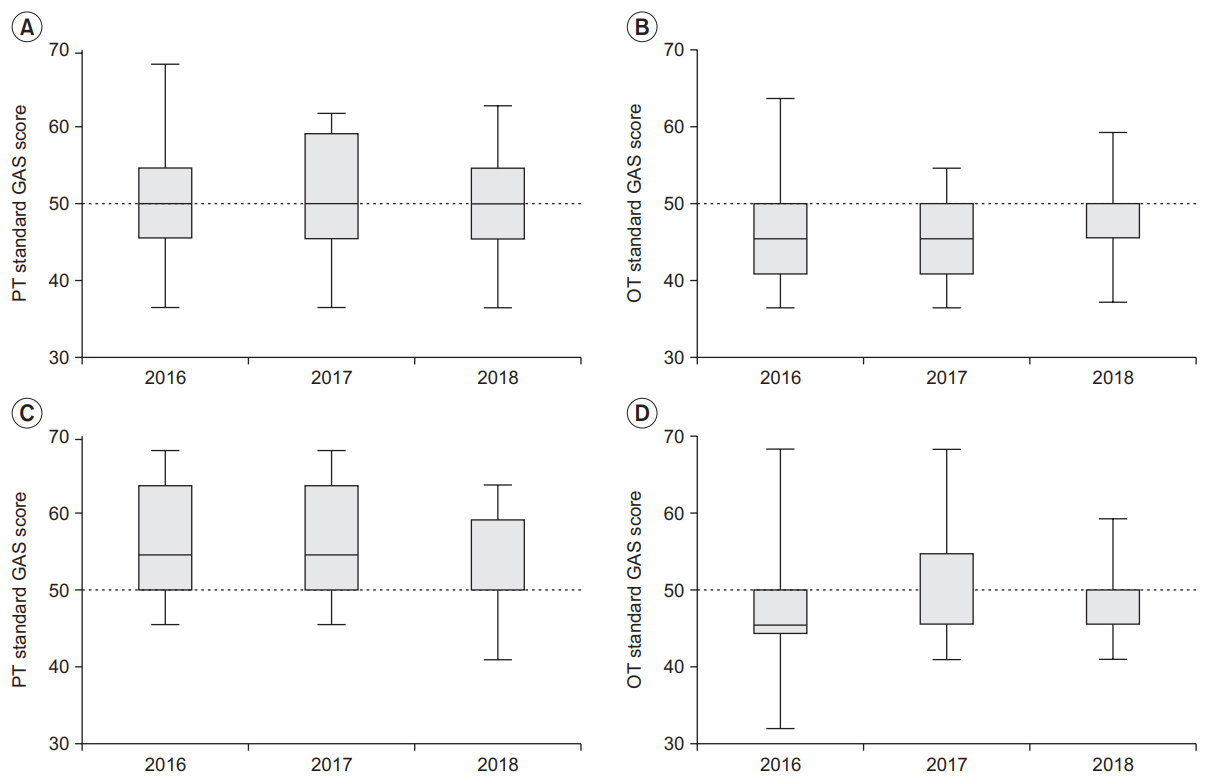
Medical records of subacute post-stroke patients who had undergone intensive rehabilitation under hospitalization, before and after the application of GAS, were collected. GAS was conducted at the initial evaluation of each patient. Specific goals were suggested by physical and occupational therapists and were determined by the responsible physiatrist. A 5-point scale was used for the GAS score after 4 weeks of rehabilitation according to the preset criteria of each goal. To evaluate the influence of GAS in rehabilitation practice, functional improvements were compared between two patient groups before (n=121) and after (n=141) GAS. To assess progress in GAS practice, the standard GAS score was calculated, and the changes were observed over a 3-year period. The standard GAS score converged to 50 points when the goal was achieved. The therapists who used GAS also completed a survey regarding its usefulness.
Results
There were no statistical differences in the motor and cognitive outcomes of the patient groups before and after applying GAS scoring. Successive yearly changes in the standard GAS scores showed progressive convergence to 50 points, signaling that the patient’s goal-setting abilities improved. According to the survey, most therapists felt that GAS enhanced the quality of therapies (84.6%).
Conclusion
GAS improved goal-setting for the rehabilitation of subacute post-stroke patients and might have a positive effect on rehabilitation.
Keyword
Figure
Reference
-
1. Bonita R, Mendis S, Truelsen T, Bogousslavsky J, Toole J, Yatsu F. The global stroke initiative. Lancet Neurol. 2004; 3:391–3.
Article2. Langhorne P, Bernhardt J, Kwakkel G. Stroke rehabilitation. Lancet. 2011; 377:1693–702.
Article3. Carod-Artal FJ, Gonzalez-Gutierrez JL, Herrero JA, Horan T, De Seijas EV. Functional recovery and instrumental activities of daily living: follow-up 1-year after treatment in a stroke unit. Brain Inj. 2002; 16:207–16.
Article4. Dobkin BH. Clinical practice: rehabilitation after stroke. N Engl J Med. 2005; 352:1677–84.5. Wressle E, Oberg B, Henriksson C. The rehabilitation process for the geriatric stroke patient: an exploratory study of goal setting and interventions. Disabil Rehabil. 1999; 21:80–7.6. Siegert RJ, Taylor WJ. Theoretical aspects of goal-setting and motivation in rehabilitation. Disabil Rehabil. 2004; 26:1–8.
Article7. Sugavanam T, Mead G, Bulley C, Donaghy M, van Wijck F. The effects and experiences of goal setting in stroke rehabilitation: a systematic review. Disabil Rehabil. 2013; 35:177–90.8. Kiresuk TJ, Sherman RE. Goal attainment scaling: a general method for evaluating comprehensive community mental health programs. Community Ment Health J. 1968; 4:443–53.
Article9. Hurn J, Kneebone I, Cropley M. Goal setting as an outcome measure: a systematic review. Clin Rehabil. 2006; 20:756–72.
Article10. Turner-Stokes L. Goal attainment scaling (GAS) in rehabilitation: a practical guide. Clin Rehabil. 2009; 23:362–70.
Article11. Krasny-Pacini A, Hiebel J, Pauly F, Godon S, Chevignard M. Goal attainment scaling in rehabilitation: a literature-based update. Ann Phys Rehabil Med. 2013; 56:212–30.
Article12. Grant M, Ponsford J. Goal attainment scaling in brain injury rehabilitation: strengths, limitations and recommendations for future applications. Neuropsychol Rehabil. 2014; 24:661–77.
Article13. Malec JF, Smigielski JS, DePompolo RW. Goal attainment scaling and outcome measurement in postacute brain injury rehabilitation. Arch Phys Med Rehabil. 1991; 72:138–43.14. Brock K, Black S, Cotton S, Kennedy G, Wilson S, Sutton E. Goal achievement in the six months after inpatient rehabilitation for stroke. Disabil Rehabil. 2009; 31:880–6.
Article15. Bernhardt J, Dewey H, Thrift A, Donnan G. Inactive and alone: physical activity within the first 14 days of acute stroke unit care. Stroke. 2004; 35:1005–9.16. Lim KB, Lee HJ, Yoo J, Kwon YG. Effect of low-frequency rTMS and NMES on subacute unilateral hemispheric stroke with dysphagia. Ann Rehabil Med. 2014; 38:592–602.
Article17. Jimenez Bunuales MT, Gonzalez Diego P, Martin Moreno JM. International Classification of Functioning, Disability and Health (ICF) 2001. Rev Esp Salud Publica. 2002; 76:271–9.
Article18. Barbarotto R, Cerri M, Acerbi C, Molinari S, Capitani E. Is SIB or BNP better than MMSE in discriminating the cognitive performance of severely impaired elderly patients? Arch Clin Neuropsychol. 2000; 15:21–9.
Article19. Bucher L. Evaluating the affective domain: consider a Likert scale. J Nurs Staff Dev. 1991; 7:234–8.20. Stolee P, Awad M, Byrne K, Deforge R, Clements S, Glenny C, et al. A multi-site study of the feasibility and clinical utility of Goal Attainment Scaling in geriatric day hospitals. Disabil Rehabil. 2012; 34:1716–26.
Article21. Steenbeek D, Ketelaar M, Galama K, Gorter JW. Goal attainment scaling in paediatric rehabilitation: a critical review of the literature. Dev Med Child Neurol. 2007; 49:550–6.
Article22. Kong KH, Chua KS, Lee J. Recovery of upper limb dexterity in patients more than 1 year after stroke: frequency, clinical correlates and predictors. NeuroRehabilitation. 2011; 28:105–11.
Article23. Buma F, Kwakkel G, Ramsey N. Understanding upper limb recovery after stroke. Restor Neurol Neurosci. 2013; 31:707–22.
Article24. Pollock A, Baer G, Campbell P, Choo PL, Forster A, Morris J, et al. Physical rehabilitation approaches for the recovery of function and mobility following stroke. Cochrane Database Syst Rev. 2014; (4):CD001920.
Article25. Prigatano GP, Wong JL. Cognitive and affective improvement in brain dysfunctional patients who achieve inpatient rehabilitation goals. Arch Phys Med Rehabil. 1999; 80:77–84.
Article26. Skidmore ER, Whyte EM, Holm MB, Becker JT, Butters MA, Dew MA, et al. Cognitive and affective predictors of rehabilitation participation after stroke. Arch Phys Med Rehabil. 2010; 91:203–7.
Article27. Wressle E, Eeg-Olofsson AM, Marcusson J, Henriksson C. Improved client participation in the rehabilitation process using a client-centred goal formulation structure. J Rehabil Med. 2002; 34:5–11.
Article28. Wade DT. Goal setting in rehabilitation: an overview of what, why and how. Clin Rehabil. 2009; 23:291–5.
Article29. Bouwens SF, van Heugten CM, Verhey FR. The practical use of goal attainment scaling for people with acquired brain injury who receive cognitive rehabilitation. Clin Rehabil. 2009; 23:310–20.
Article30. Doig E, Fleming J, Kuipers P, Cornwell PL. Clinical utility of the combined use of the Canadian Occupational Performance Measure and Goal Attainment Scaling. Am J Occup Ther. 2010; 64:904–14.
Article31. Bovend’Eerdt TJ, Botell RE, Wade DT. Writing SMART rehabilitation goals and achieving goal attainment scaling: a practical guide. Clin Rehabil. 2009; 23:352–61.
Article32. Forbes DA. Goal Attainment Scaling: a responsive measure of client outcomes. J Gerontol Nurs. 1998; 24:34–40.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Role of Intensive Inpatient Rehabilitation for Prevention of Disability after Stroke: The Korean Stroke Cohort for Functioning and Rehabilitation (KOSCO) Study
- Short-Term Effects of Intensive Inpatient Rehabilitation in Patients with Brain Tumor: a Single-Center Experience
- Mean Platelet Component Change according to Stage in Stroke Patients
- Changes in Epidemiological Trends and Rehabilitation Usage in Neurological Diseases in Korea: Stroke
- Trunk Impairment Scale for Predicting Lumbar Spine Bone Mineral Density in Young Male Patients With Subacute Stroke