Diabetes Metab J.
2020 Apr;44(2):267-276. 10.4093/dmj.2019.0001.
Association between Non-Alcoholic Steatohepatitis and Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Mellitus
- Affiliations
-
- 1Departments of Internal Medicine, Yonsei University College of Medicine, Seoul, Korea
- 2Departments of Preventive Medicine, Yonsei University College of Medicine, Seoul, Korea
- 3Division of Endocrinology and Metabolism, Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea
- 4Huh’s Diabetes Center and the 21st Century Diabetes and Vascular Research Institute, Seoul, Korea
- 5Institute of Endocrine Research, Yonsei University College of Medicine, Seoul, Korea
- 6Brain Korea 21 PLUS Project for Medical Science, Yonsei University College of Medicine, Seoul, Korea
- 7Department of Systems Biology, Glycosylation Network Research Center, Yonsei University, Seoul, Korea
- KMID: 2502408
- DOI: http://doi.org/10.4093/dmj.2019.0001
Abstract
- Background
Impaired diastolic heart function has been observed in persons with non-alcoholic fatty liver disease (NAFLD) and/or with type 2 diabetes mellitus (T2DM). However, it is unclear whether NAFLD fibrotic progression, i.e., non-alcoholic steatohepatitis, poses an independent risk for diastolic dysfunction in T2DM. We investigated the association between liver fibrosis and left ventricular (LV) diastolic dysfunction in T2DM.
Methods
We analyzed 606 patients with T2DM, aged ≥50 years, who had undergone liver ultrasonography and pulsed-wave Doppler echocardiography. Insulin sensitivity was measured by short insulin tolerance test. Presence of NAFLD and/or advanced liver fibrosis was determined by abdominal ultrasonography and NAFLD fibrosis score (NFS). LV diastolic dysfunction was defined according to transmitral peak early to late ventricular filling (E/A) ratio and deceleration time, using echocardiography.
Results
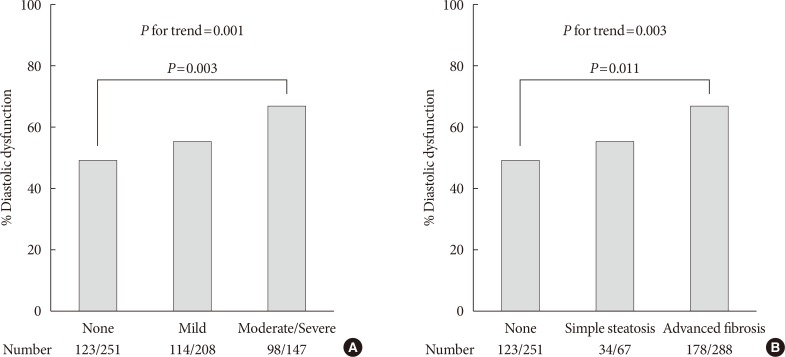
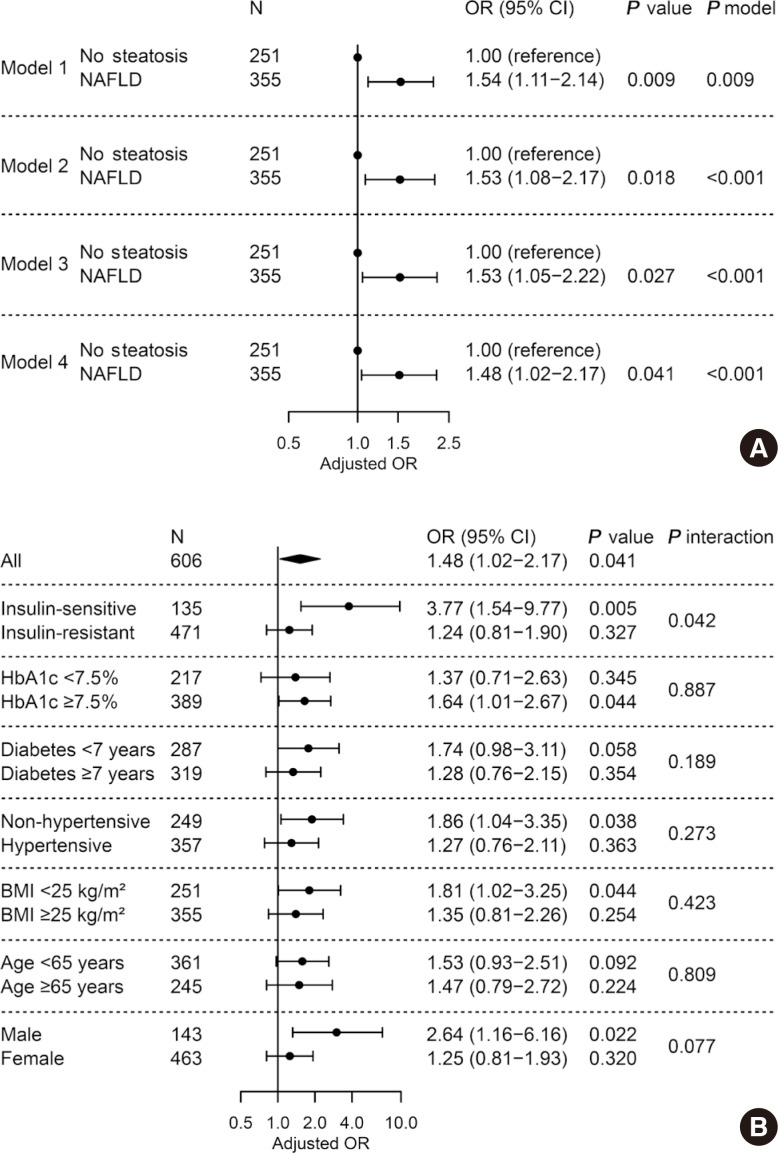
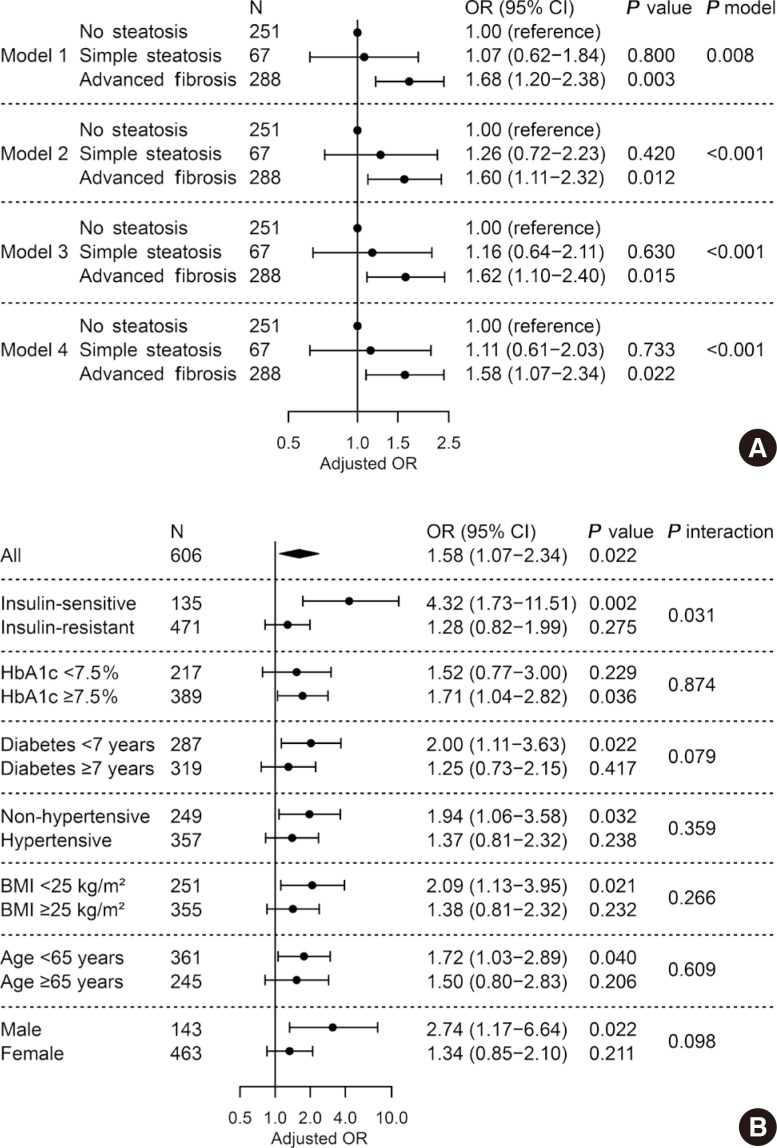
LV diastolic dysfunction was significantly more prevalent in the NAFLD versus non-NAFLD group (59.7% vs. 49.0%, P=0.011). When NAFLD was stratified by NFS, subjects with advanced liver fibrosis exhibited a higher prevalence of diastolic dysfunction (49.0%, 50.7%, 61.8%; none, simple steatosis, advanced fibrosis, respectively; P for trend=0.003). In multivariable logistic regression, liver fibrosis was independently associated with diastolic dysfunction (odds ratio [OR], 1.58; 95% confidence interval [CI], 1.07 to 2.34; P=0.022) after adjusting for insulin resistance and cardiometabolic risk factors. This association remained significant in patients without insulin resistance (OR, 4.32; 95% CI, 1.73 to 11.51; P=0.002).
Conclusions
Liver fibrosis was associated with LV diastolic dysfunction in patients with T2DM and may be an independent risk factor for diastolic dysfunction, especially in patients without systemic insulin resistance.
Keyword
Figure
Cited by 2 articles
-
Letter: Association between Non-Alcoholic Steatohepatitis and Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Mellitus (
Diabetes Metab J 2020;44:267–76)
Sung Hoon Yu
Diabetes Metab J. 2020;44(3):482-483. doi: 10.4093/dmj.2020.0123.Response: Association between Non-Alcoholic Steatohepatitis and Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Mellitus (
Diabetes Metab J 2020;44:267–76)
Hokyou Lee, Gyuri Kim, Yong-ho Lee
Diabetes Metab J. 2020;44(3):486-487. doi: 10.4093/dmj.2020.0127.
Reference
-
1. Loomba R, Sanyal AJ. The global NAFLD epidemic. Nat Rev Gastroenterol Hepatol. 2013; 10:686–690. PMID: 24042449.
Article2. Browning JD, Szczepaniak LS, Dobbins R, Nuremberg P, Horton JD, Cohen JC, Grundy SM, Hobbs HH. Prevalence of hepatic steatosis in an urban population in the United States: impact of ethnicity. Hepatology. 2004; 40:1387–1395. PMID: 15565570.
Article3. Farrell GC, Wong VW, Chitturi S. NAFLD in Asia: as common and important as in the west. Nat Rev Gastroenterol Hepatol. 2013; 10:307–318. PMID: 23458891.4. Musso G, Cassader M, Gambino R. Non-alcoholic steatohepatitis: emerging molecular targets and therapeutic strategies. Nat Rev Drug Discov. 2016; 15:249–274. PMID: 26794269.
Article5. Wong RJ, Aguilar M, Cheung R, Perumpail RB, Harrison SA, Younossi ZM, Ahmed A. Nonalcoholic steatohepatitis is the second leading etiology of liver disease among adults awaiting liver transplantation in the United States. Gastroenterology. 2015; 148:547–555. PMID: 25461851.
Article6. Ong JP, Pitts A, Younossi ZM. Increased overall mortality and liver-related mortality in non-alcoholic fatty liver disease. J Hepatol. 2008; 49:608–612. PMID: 18682312.
Article7. Azzam H, Malnick S. Non-alcoholic fatty liver disease: the heart of the matter. World J Hepatol. 2015; 7:1369–1376. PMID: 26052382.8. Han E, Lee YH. Non-alcoholic fatty liver disease: the emerging burden in cardiometabolic and renal diseases. Diabetes Metab J. 2017; 41:430–437. PMID: 29199410.
Article9. Assy N, Djibre A, Farah R, Grosovski M, Marmor A. Presence of coronary plaques in patients with nonalcoholic fatty liver disease. Radiology. 2010; 254:393–400. PMID: 20093511.
Article10. Jaruvongvanich V, Chenbhanich J, Sanguankeo A, Rattanawong P, Wijarnpreecha K, Upala S. Increased arterial stiffness in nonalcoholic fatty liver disease: a systematic review and meta-analysis. Eur J Gastroenterol Hepatol. 2017; 29:e28–e35. PMID: 28542113.
Article11. Goland S, Shimoni S, Zornitzki T, Knobler H, Azoulai O, Lutaty G, Melzer E, Orr A, Caspi A, Malnick S. Cardiac abnormalities as a new manifestation of nonalcoholic fatty liver disease: echocardiographic and tissue Doppler imaging assessment. J Clin Gastroenterol. 2006; 40:949–955. PMID: 17063117.
Article12. Fotbolcu H, Yakar T, Duman D, Karaahmet T, Tigen K, Cevik C, Kurtoglu U, Dindar I. Impairment of the left ventricular systolic and diastolic function in patients with non-alcoholic fatty liver disease. Cardiol J. 2010; 17:457–463. PMID: 20865675.13. Kim NH, Park J, Kim SH, Kim YH, Kim DH, Cho GY, Baik I, Lim HE, Kim EJ, Na JO, Lee JB, Lee SK, Shin C. Non-alcoholic fatty liver disease, metabolic syndrome and subclinical cardiovascular changes in the general population. Heart. 2014; 100:938–943. PMID: 24721975.
Article14. VanWagner LB, Wilcox JE, Colangelo LA, Lloyd-Jones DM, Carr JJ, Lima JA, Lewis CE, Rinella ME, Shah SJ. Association of nonalcoholic fatty liver disease with subclinical myocardial remodeling and dysfunction: a population-based study. Hepatology. 2015; 62:773–783. PMID: 25914296.
Article15. Bonapace S, Perseghin G, Molon G, Canali G, Bertolini L, Zoppini G, Barbieri E, Targher G. Nonalcoholic fatty liver disease is associated with left ventricular diastolic dysfunction in patients with type 2 diabetes. Diabetes Care. 2012; 35:389–395. PMID: 22210573.
Article16. Mantovani A, Pernigo M, Bergamini C, Bonapace S, Lipari P, Pichiri I, Bertolini L, Valbusa F, Barbieri E, Zoppini G, Bonora E, Targher G. Nonalcoholic fatty liver disease is independently associated with early left ventricular diastolic dysfunction in patients with type 2 diabetes. PLoS One. 2015; 10:e0135329. PMID: 26252899.
Article17. Perseghin G, Lattuada G, De Cobelli F, Esposito A, Belloni E, Ntali G, Ragogna F, Canu T, Scifo P, Del Maschio A, Luzi L. Increased mediastinal fat and impaired left ventricular energy metabolism in young men with newly found fatty liver. Hepatology. 2008; 47:51–58. PMID: 17955548.
Article18. Ekstedt M, Hagstrom H, Nasr P, Fredrikson M, Stal P, Kechagias S, Hultcrantz R. Fibrosis stage is the strongest predictor for disease-specific mortality in NAFLD after up to 33 years of follow-up. Hepatology. 2015; 61:1547–1554. PMID: 25125077.
Article19. Petta S, Argano C, Colomba D, Camma C, Di Marco V, Cabibi D, Tuttolomondo A, Marchesini G, Pinto A, Licata G, Craxi A. Epicardial fat, cardiac geometry and cardiac function in patients with non-alcoholic fatty liver disease: association with the severity of liver disease. J Hepatol. 2015; 62:928–933. PMID: 25445395.
Article20. Simon TG, Bamira DG, Chung RT, Weiner RB, Corey KE. Nonalcoholic steatohepatitis is associated with cardiac remodeling and dysfunction. Obesity (Silver Spring). 2017; 25:1313–1316. PMID: 28745025.
Article21. Fang ZY, Prins JB, Marwick TH. Diabetic cardiomyopathy: evidence, mechanisms, and therapeutic implications. Endocr Rev. 2004; 25:543–567. PMID: 15294881.
Article22. Jia G, DeMarco VG, Sowers JR. Insulin resistance and hyperinsulinaemia in diabetic cardiomyopathy. Nat Rev Endocrinol. 2016; 12:144–153. PMID: 26678809.
Article23. Bonora E, Moghetti P, Zancanaro C, Cigolini M, Querena M, Cacciatori V, Corgnati A, Muggeo M. Estimates of in vivo insulin action in man: comparison of insulin tolerance tests with euglycemic and hyperglycemic glucose clamp studies. J Clin Endocrinol Metab. 1989; 68:374–378. PMID: 2645308.24. Kim SK, Choi YJ, Huh BW, Park SW, Lee EJ, Cho YW, Huh KB. Nonalcoholic Fatty liver disease is associated with increased carotid intima-media thickness only in type 2 diabetic subjects with insulin resistance. J Clin Endocrinol Metab. 2014; 99:1879–1884. PMID: 24512497.
Article25. Angulo P, Hui JM, Marchesini G, Bugianesi E, George J, Farrell GC, Enders F, Saksena S, Burt AD, Bida JP, Lindor K, Sanderson SO, Lenzi M, Adams LA, Kench J, Therneau TM, Day CP. The NAFLD fibrosis score: a noninvasive system that identifies liver fibrosis in patients with NAFLD. Hepatology. 2007; 45:846–854. PMID: 17393509.
Article26. Devereux RB, Alonso DR, Lutas EM, Gottlieb GJ, Campo E, Sachs I, Reichek N. Echocardiographic assessment of left ventricular hypertrophy: comparison to necropsy findings. Am J Cardiol. 1986; 57:450–458. PMID: 2936235.
Article27. Lubien E, DeMaria A, Krishnaswamy P, Clopton P, Koon J, Kazanegra R, Gardetto N, Wanner E, Maisel AS. Utility of B-natriuretic peptide in detecting diastolic dysfunction: comparison with Doppler velocity recordings. Circulation. 2002; 105:595–601. PMID: 11827925.28. Cassidy S, Hallsworth K, Thoma C, MacGowan GA, Hollingsworth KG, Day CP, Taylor R, Jakovljevic DG, Trenell MI. Cardiac structure and function are altered in type 2 diabetes and non-alcoholic fatty liver disease and associate with glycemic control. Cardiovasc Diabetol. 2015; 14:23. PMID: 25849783.
Article29. Kim G, Jo K, Kim KJ, Lee YH, Han E, Yoon HJ, Wang HJ, Kang ES, Yun M. Visceral adiposity is associated with altered myocardial glucose uptake measured by (18)FDG-PET in 346 subjects with normal glucose tolerance, prediabetes, and type 2 diabetes. Cardiovasc Diabetol. 2015; 14:148. PMID: 26538247.
Article30. Lee YH, Kim KJ, Yoo ME, Kim G, Yoon HJ, Jo K, Youn JC, Yun M, Park JY, Shim CY, Lee BW, Kang SM, Ha JW, Cha BS, Kang ES. Association of non-alcoholic steatohepatitis with subclinical myocardial dysfunction in non-cirrhotic patients. J Hepatol. 2018; 68:764–772. PMID: 29175242.
Article31. Levelt E, Pavlides M, Banerjee R, Mahmod M, Kelly C, Sellwood J, Ariga R, Thomas S, Francis J, Rodgers C, Clarke W, Sabharwal N, Antoniades C, Schneider J, Robson M, Clarke K, Karamitsos T, Rider O, Neubauer S. Ectopic and visceral fat deposition in lean and obese patients with type 2 diabetes. J Am Coll Cardiol. 2016; 68:53–63. PMID: 27364051.32. Cherian S, Lopaschuk GD, Carvalho E. Cellular cross-talk between epicardial adipose tissue and myocardium in relation to the pathogenesis of cardiovascular disease. Am J Physiol Endocrinol Metab. 2012; 303:E937–E949. PMID: 22895783.
Article33. Targher G, Day CP, Bonora E. Risk of cardiovascular disease in patients with nonalcoholic fatty liver disease. N Engl J Med. 2010; 363:1341–1350. PMID: 20879883.
Article34. van Heerebeek L, Hamdani N, Handoko ML, Falcao-Pires I, Musters RJ, Kupreishvili K, Ijsselmuiden AJ, Schalkwijk CG, Bronzwaer JG, Diamant M, Borbely A, van der Velden J, Stienen GJ, Laarman GJ, Niessen HW, Paulus WJ. Diastolic stiffness of the failing diabetic heart: importance of fibrosis, advanced glycation end products, and myocyte resting tension. Circulation. 2008; 117:43–51. PMID: 18071071.
Article35. Meex RCR, Watt MJ. Hepatokines: linking nonalcoholic fatty liver disease and insulin resistance. Nat Rev Endocrinol. 2017; 13:509–520. PMID: 28621339.
Article36. Adams LA, Anstee QM, Tilg H, Targher G. Non-alcoholic fatty liver disease and its relationship with cardiovascular disease and other extrahepatic diseases. Gut. 2017; 66:1138–1153. PMID: 28314735.
Article37. Poirier P, Bogaty P, Garneau C, Marois L, Dumesnil JG. Diastolic dysfunction in normotensive men with well-controlled type 2 diabetes: importance of maneuvers in echocardiographic screening for preclinical diabetic cardiomyopathy. Diabetes Care. 2001; 24:5–10. PMID: 11194240.
Article38. Bella JN, Palmieri V, Roman MJ, Liu JE, Welty TK, Lee ET, Fabsitz RR, Howard BV, Devereux RB. Mitral ratio of peak early to late diastolic filling velocity as a predictor of mortality in middle-aged and elderly adults: the Strong Heart Study. Circulation. 2002; 105:1928–1933. PMID: 11997279.39. Tsang TS, Gersh BJ, Appleton CP, Tajik AJ, Barnes ME, Bailey KR, Oh JK, Leibson C, Montgomery SC, Seward JB. Left ventricular diastolic dysfunction as a predictor of the first diagnosed nonvalvular atrial fibrillation in 840 elderly men and women. J Am Coll Cardiol. 2002; 40:1636–1644. PMID: 12427417.
Article40. Fischer M, Baessler A, Hense HW, Hengstenberg C, Muscholl M, Holmer S, Doring A, Broeckel U, Riegger G, Schunkert H. Prevalence of left ventricular diastolic dysfunction in the community. Results from a Doppler echocardiographic-based survey of a population sample. Eur Heart J. 2003; 24:320–328. PMID: 12581679.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Letter: Association between Non-Alcoholic Steatohepatitis and Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Mellitus (
Diabetes Metab J 2020;44:267–76) - Response: Association between Non-Alcoholic Steatohepatitis and Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Mellitus (
Diabetes Metab J 2020;44:267–76) - Left Ventricular Diastolic Functions by M-Mode Echocardiogram in Essential Hypertensive Patients
- Risk Factors Associated with Left Ventricular Diastolic Dysfunction in Type 2 Diabetic Patients without Hypertension
- Preoperative echocardiographic evaluation of cardiac systolic and diastolic function in liver transplant recipients with diabetes mellitus: a propensity-score matched analysis
- Letter: Association between Non-Alcoholic Steatohepatitis and Left Ventricular Diastolic Dysfunction in Type 2 Diabetes Mellitus (