J Gastric Cancer.
2020 Mar;20(1):72-80. 10.5230/jgc.2020.20.e5.
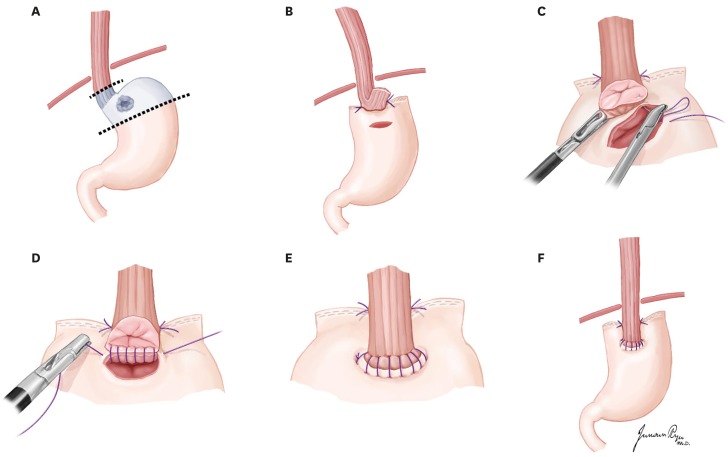
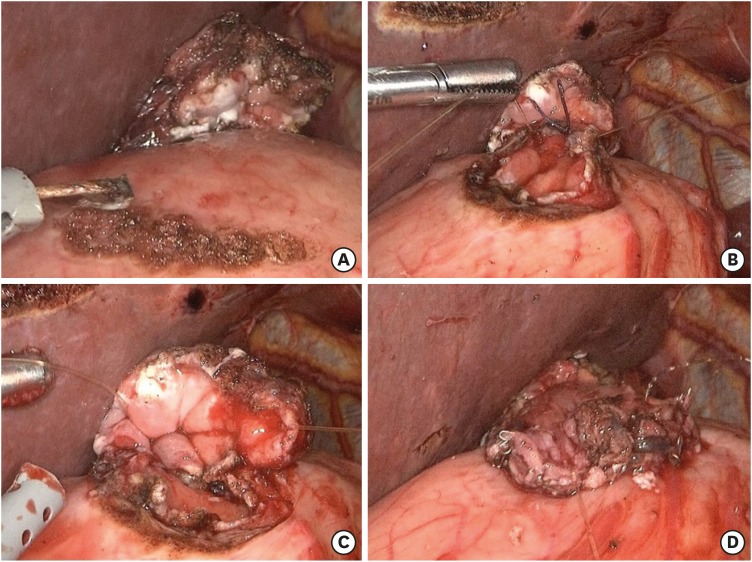
Spade-Shaped Anastomosis Following a Proximal Gastrectomy Using a Double Suture to Fix the Posterior Esophageal Wall to the Anterior Gastric Wall (SPADE Operation): Case-Control Study of Early Outcomes
- Affiliations
-
- 1Center for Gastric Cancer, National Cancer Center, Goyang, Korea. gskim@ncc.re.kr
- 2Department of Otolaryngology-Head and Neck Surgery, Center for Thyroid Cancer, National Cancer Center, Goyang, Korea.
- 3Department of Cancer Control and Population Health, National Cancer Center Graduate School of Cancer Science and Policy, Goyang, Korea.
- KMID: 2471927
- DOI: http://doi.org/10.5230/jgc.2020.20.e5
Abstract
- PURPOSE
Proximal gastrectomy (PG) is a function-preserving surgery in cases of proximally located early-stage gastric cancer. Because gastroesophageal reflux is a major pitfall of this operation, we devised a modified esophagogastrostomy (EG) anastomosis to fix the distal part of the posterior esophageal wall to the proximal part of the anterior stomach wall to produce an anti-reflux mechanism; we named this the SPADE operation. This study aimed to show demonstrate the clinical outcomes of the SPADE operation and compare them to those of previous PG cases.
MATERIALS AND METHODS
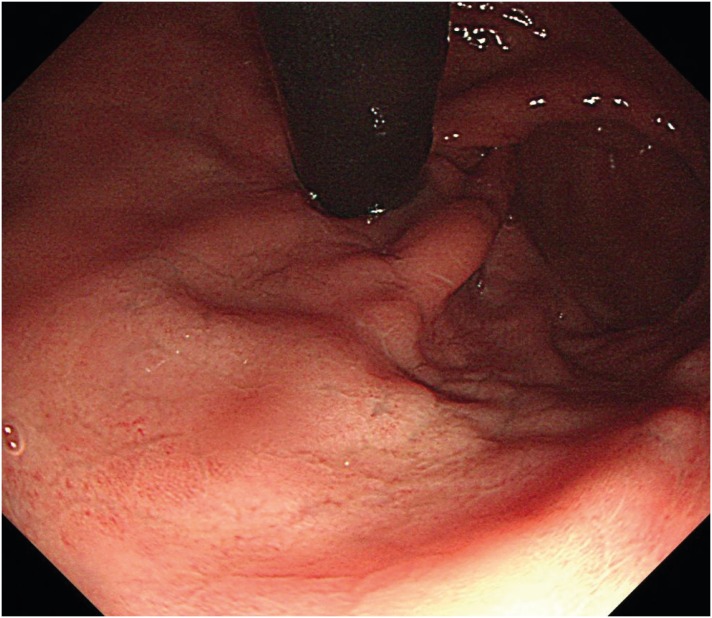
Case details of 56 patients who underwent PG between January 2012 and March 2018 were retrospectively reviewed: 30 underwent conventional esophagogastrostomy (CEG) anastomosis using a circular stapler, while 26 underwent the SPADE operation. Early postoperative clinical outcome-related reflux symptoms, endoscopic findings, and postoperative complications were compared in this case-control study.
RESULTS
Follow-up endoscopy showed more frequent reflux esophagitis cases in the CEG group than in the SPADE group (30% vs. 15.3%, P=0.19). Similarly, bile reflux (26.7% vs. 7.7%, P=0.08) and residual food (P=0.01) cases occurred more frequently in the CEG group than in the SPADE group. In the CEG group, 13 patients (43.3%) had mild reflux symptoms, while 3 patients (10%) had severe reflux symptoms. In the SPADE group, 3 patients (11.5%) had mild reflux symptoms, while 1 had severe reflux symptoms (absolute difference, 31.8%; 95% confidence interval, 1.11-29.64; P=0.01).
CONCLUSIONS
A novel modified EG, the SPADE operation, has the potential to decrease gastroesophageal reflux following a PG.
Keyword
MeSH Terms
Figure
Reference
-
1. Katai H, Sano T, Fukagawa T, Shinohara H, Sasako M. Prospective study of proximal gastrectomy for early gastric cancer in the upper third of the stomach. Br J Surg. 2003; 90:850–853. PMID: 12854112.
Article2. Liedman B. Symptoms after total gastrectomy on food intake, body composition, bone metabolism, and quality of life in gastric cancer patients--is reconstruction with a reservoir worthwhile? Nutrition. 1999; 15:677–682. PMID: 10467612.
Article3. Hosoda K, Yamashita K, Katada N, Moriya H, Mieno H, Shibata T, et al. Potential benefits of laparoscopy-assisted proximal gastrectomy with esophagogastrostomy for cT1 upper-third gastric cancer. Surg Endosc. 2016; 30:3426–3436. PMID: 26511124.
Article4. Adachi Y, Inoue T, Hagino Y, Shiraishi N, Shimoda K, Kitano S. Surgical results of proximal gastrectomy for early-stage gastric cancer: jejunal interposition and gastric tube reconstruction. Gastric Cancer. 1999; 2:40–45. PMID: 11957069.
Article5. Muraoka A, Kobayashi M, Kokudo Y. Laparoscopy-assisted proximal gastrectomy with the hinged double flap method. World J Surg. 2016; 40:2419–2424. PMID: 27094564.
Article6. Huh YJ, Lee HJ, Oh SY, Lee KG, Yang JY, Ahn HS, et al. Clinical outcome of modified laparoscopy-assisted proximal gastrectomy compared to conventional proximal gastrectomy or total gastrectomy for upper-third early gastric cancer with special references to post-operative reflux esophagitis. J Gastric Cancer. 2015; 15:191–200. PMID: 26468417.
Article7. Hsu CP, Chen CY, Hsieh YH, Hsia JY, Shai SE, Kao CH. Esophageal reflux after total or proximal gastrectomy in patients with adenocarcinoma of the gastric cardia. Am J Gastroenterol. 1997; 92:1347–1350. PMID: 9260804.8. Ahn SH, Jung DH, Son SY, Lee CM, Park DJ, Kim HH. Laparoscopic double-tract proximal gastrectomy for proximal early gastric cancer. . Gastric Cancer. 2014; 17:562–570. PMID: 24052482.
Article9. Han WH, Kim YW, Kim DH, Shahin MA, Yun YI. Video of totally laparoscopic modified esophagogastrostomy using a spade shaped anastomosis following proximal gastrectomy (SPADE Operation). J Minim Invasive Surg. 2017; 20:163–165.
Article10. Delattre JF, Avisse C, Marcus C, Flament JB. Functional anatomy of the gastroesophageal junction. Surg Clin North Am. 2000; 80:241–260. PMID: 10685151.
Article11. Armstrong D, Bennett JR, Blum AL, Dent J, De Dombal FT, Galmiche JP, et al. The endoscopic assessment of esophagitis: a progress report on observer agreement. Gastroenterology. 1996; 111:85–92. PMID: 8698230.
Article12. Kubo M, Sasako M, Gotoda T, Ono H, Fujishiro M, Saito D, et al. Endoscopic evaluation of the remnant stomach after gastrectomy: proposal for a new classification. Gastric Cancer. 2002; 5:83–89. PMID: 12111583.
Article13. Japanese gastric cancer treatment guidelines 2014 (ver. 4). Gastric Cancer. 2017; 20:1–19.14. Kayani B, Garas G, Arshad M, Athanasiou T, Darzi A, Zacharakis E. Is hand-sewn anastomosis superior to stapled anastomosis following oesophagectomy? Int J Surg. 2014; 12:7–15. PMID: 24239928.
Article15. Saluja SS, Ray S, Pal S, Sanyal S, Agrawal N, Dash NR, et al. Randomized trial comparing side-to-side stapled and hand-sewn esophagogastric anastomosis in neck. J Gastrointest Surg. 2012; 16:1287–1295. PMID: 22528571.
Article16. Ohyama S, Tokunaga M, Hiki N, Fukunaga T, Fujisaki J, Seto Y, et al. A clinicopathological study of gastric stump carcinoma following proximal gastrectomy. Gastric Cancer. 2009; 12:88–94. PMID: 19562462.
Article17. Takeshita K, Saito N, Saeki I, Honda T, Tani M, Kando F, et al. Proximal gastrectomy and jejunal pouch interposition for the treatment of early cancer in the upper third of the stomach: surgical techniques and evaluation of postoperative function. Surgery. 1997; 121:278–286. PMID: 9092128.
Article18. Kamikawa Y, Kobayashi T, Ueyama S, Satomoto K. A new antireflux procedure in esophagogastrostomy after proximal gastrectomy. Gastroenterol Surg. 2001; 24:1053–1060.19. Nishigori T, Okabe H, Tsunoda S, Shinohara H, Obama K, Hosogi H, et al. Superiority of laparoscopic proximal gastrectomy with hand-sewn esophagogastrostomy over total gastrectomy in improving postoperative body weight loss and quality of life. Surg Endosc. 2017; 31:3664–3672. PMID: 28078458.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Video of Totally Laparoscopic Modified Esophagogastrostomy Using a Spade Shaped Anastomosis Following Proximal Gastrectomy (SPADE Operation)
- Proximal Anterior-Antrum Posterior (PAAP) Overlapping Anastomosis in Minimally Invasive Pylorus-Preserving Gastrectomy for Early Gastric Cancer Located in the High Body and Posterior Wall of the Stomach
- Inflammatory Myofibroblastic Tumor Treated with Laparoscopic Proximal Gastrectomy and Double-Tract Anastomosis
- Continuous Sutures for Microarterial Anastomosis
- Omental Free Shaped Flap Reinforcement on Anastomosis and Dissected Area (OFFROAD) Following Gastrectomy