Allergy Asthma Immunol Res.
2020 May;12(3):443-453. 10.4168/aair.2020.12.3.443.
Risk Factors for Acute Exacerbations in Elderly Asthma: What Makes Asthma in Older Adults Distinctive?
- Affiliations
-
- 1Institute of Allergy and Clinical Immunology, Seoul National University Medical Research Center, Seoul National University College of Medicine, Seoul, Korea. shcho@snu.ac.kr
- 2Department of Internal Medicine, Kyung Hee University Medical Center, Seoul, Korea.
- 3Department of Allergy and Clinical Immunology, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea.
- 4Division of Allergy and Respiratory Medicine, Soonchunhyang University Bucheon Hospital, Bucheon, Korea.
- 5Division of Allergy and Clinical Immunology, Department of Internal Medicine, Seoul National University College of Medicine, Seoul, Korea.
- KMID: 2471228
- DOI: http://doi.org/10.4168/aair.2020.12.3.443
Abstract
- PURPOSE
Asthma in the elderly (EA; ≥ 65 years of age) is increasing, adding a heavy socioeconomic burden to the healthcare system. However, little is known about risk factors associated with acute exacerbations in EA patients. The objective of this study was to investigate risk factors for acute exacerbation in EA compared to non-elderly asthma (NEA).
METHODS
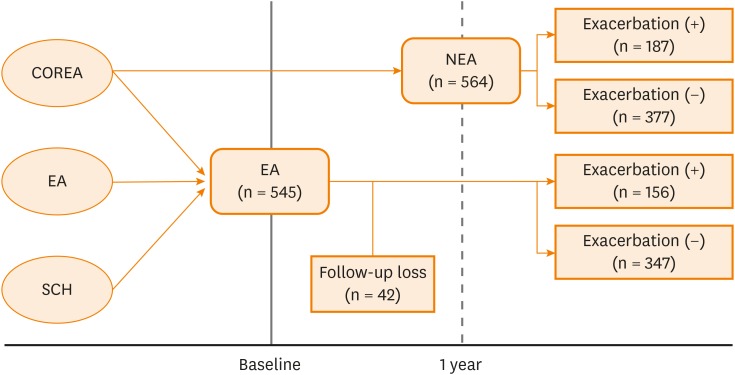
We combined data from 3 adult asthma cohorts under a unified protocol and database. Asthmatic patients with regular follow-up during a 1-year period were selected from the cohorts to identify the risk factors predicting acute exacerbations in EA compared to NEA.
RESULTS
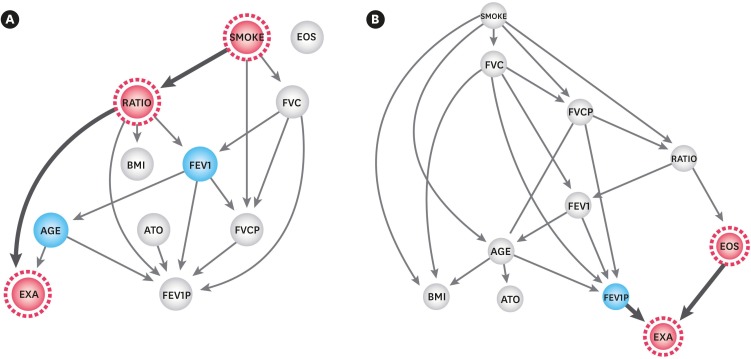
We selected a total of 1,086 patients from the merged cohort. During the observation period, 503 and 583 patients were assigned to the EA and NEA groups, respectively. The exacerbation rate was 31.0% in the EA and 33.2% in the NEA group. Multivariate logistic regression analysis revealed fixed airway obstruction, chronic rhinosinusitis (CRS), and male sex as independent risk factors for exacerbation in the EA group. In the NEA group, exacerbation increased along with an increase in eosinophil count. Bayesian analysis of the interactions among clinical factors revealed that forced expiratory volume in 1 second/forced vital capacity was directly related to exacerbation in the EA group, and eosinophil count was related to exacerbation in the NEA group.
CONCLUSIONS
We suggest that fixed airway obstruction and CRS as the important clinical factors predicting acute exacerbations in EA, whereas in NEA, eosinophil count was the strong predictor of exacerbation.
Keyword
MeSH Terms
Figure
Reference
-
1. Garner R, Kohen D. Changes in the prevalence of asthma among Canadian children. Health Rep. 2008; 19:45–50.2. Gibson PG, McDonald VM, Marks GB. Asthma in older adults. Lancet. 2010; 376:803–813. PMID: 20816547.
Article3. Moorman JE, Akinbami LJ, Bailey CM, Zahran HS, King ME, Johnson CA, et al. National surveillance of asthma: United States, 2001–2010. Vital Health Stat 3. 2012; 1–58. PMID: 24252609.4. Tsai CL, Lee WY, Hanania NA, Camargo CA. Age-related differences in clinical outcomes for acute asthma in the United States, 2006–2008. J Allergy Clin Immunol. 2012; 129:1252–1258.e1. PMID: 22385630.
Article5. Szefler SJ. Asthma across the lifespan: time for a paradigm shift. J Allergy Clin Immunol. 2018; 142:773–780. PMID: 29627424.
Article6. Song WJ, Cho SH. Challenges in the management of asthma in the elderly. Allergy Asthma Immunol Res. 2015; 7:431–439. PMID: 26122503.
Article7. Park HW, Kim TW, Song WJ, Kim SH, Park HK, Kim SH, et al. Prediction of asthma exacerbations in elderly adults: results of a 1-year prospective study. J Am Geriatr Soc. 2013; 61:1631–1632. PMID: 24028367.
Article8. Park HW, Kwon HS, Kim TB, Kim SH, Chang YS, Jang AS, et al. Differences between asthma in young and elderly: results from the COREA study. Respir Med. 2013; 107:1509–1514. PMID: 23927852.9. Sano H, Iwanaga T, Nishiyama O, Sano A, Higashimoto Y, Tomita K, et al. Characteristics of phenotypes of elderly patients with asthma. Allergol Int. 2016; 65:204–209. PMID: 26786397.
Article10. Inoue H, Niimi A, Takeda T, Matsumoto H, Ito I, Matsuoka H, et al. Pathophysiological characteristics of asthma in the elderly: a comprehensive study. Ann Allergy Asthma Immunol. 2014; 113:527–533. PMID: 25216975.
Article11. Ulambayar B, Lee SH, Yang EM, Ye YM, Park HS. Association between epithelial cytokines and clinical phenotypes of elderly asthma. Allergy Asthma Immunol Res. 2019; 11:79–89. PMID: 30479079.
Article12. Shoemaker JS, Painter IS, Weir BS. Bayesian statistics in genetics: a guide for the uninitiated. Trends Genet. 1999; 15:354–358. PMID: 10461203.
Article13. Ashby D. Bayesian statistics in medicine: a 25 year review. Stat Med. 2006; 25:3589–3631. PMID: 16947924.
Article14. Arora P, Boyne D, Slater JJ, Gupta A, Brenner DR, Druzdzel MJ. Bayesian networks for risk prediction using real-world data: a tool for precision medicine. Value Health. 2019; 22:439–445. PMID: 30975395.
Article15. Kim TB, Jang AS, Kwon HS, Park JS, Chang YS, Cho SH, et al. Identification of asthma clusters in two independent Korean adult asthma cohorts. Eur Respir J. 2013; 41:1308–1314. PMID: 23060627.
Article16. Kim TB, Park CS, Bae YJ, Cho YS, Moon HB. COREA Study Group. Factors associated with severity and exacerbation of asthma: a baseline analysis of the cohort for reality and evolution of adult asthma in Korea (COREA). Ann Allergy Asthma Immunol. 2009; 103:311–317. PMID: 19852195.
Article17. Reddel HK, Taylor DR, Bateman ED, Boulet LP, Boushey HA, Busse WW, et al. An official American Thoracic Society/European Respiratory Society statement: asthma control and exacerbations: standardizing endpoints for clinical asthma trials and clinical practice. Am J Respir Crit Care Med. 2009; 180:59–99. PMID: 19535666.18. Purdy S, Griffin T, Salisbury C, Sharp D. Ambulatory care sensitive conditions: terminology and disease coding need to be more specific to aid policy makers and clinicians. Public Health. 2009; 123:169–173. PMID: 19144363.
Article19. Warner SM, Knight DA. Airway modeling and remodeling in the pathogenesis of asthma. Curr Opin Allergy Clin Immunol. 2008; 8:44–48. PMID: 18188017.
Article20. Barnes PJ. Corticosteroid resistance in patients with asthma and chronic obstructive pulmonary disease. J Allergy Clin Immunol. 2013; 131:636–645. PMID: 23360759.
Article21. Global Initiative for Asthma. Global strategy for asthma management and prevention [Internet]. Fontana (WI): Global Initiative for Asthma;2019. Available from: http://ginasthma.org/gina-reports.22. Kerstjens HA, Engel M, Dahl R, Paggiaro P, Beck E, Vandewalker M, et al. Tiotropium in asthma poorly controlled with standard combination therapy. N Engl J Med. 2012; 367:1198–1207. PMID: 22938706.
Article23. Kim SW, Kim JH, Park CK, Kim TJ, Lee SY, Kim YK, et al. Effect of roflumilast on airway remodelling in a murine model of chronic asthma. Clin Exp Allergy. 2016; 46:754–763. PMID: 26542330.
Article24. Barua P, O'Mahony MS. Overcoming gaps in the management of asthma in older patients: new insights. Drugs Aging. 2005; 22:1029–1059. PMID: 16363886.25. Kim YK, Kim SH, Tak YJ, Jee YK, Lee BJ, Kim SH, et al. High prevalence of current asthma and active smoking effect among the elderly. Clin Exp Allergy. 2002; 32:1706–1712. PMID: 12653160.
Article26. Park HW, Song WJ, Kim SH, Park HK, Kim SH, Kwon YE, et al. Classification and implementation of asthma phenotypes in elderly patients. Ann Allergy Asthma Immunol. 2015; 114:18–22. PMID: 25455518.
Article27. Sutherland ER, Goleva E, King TS, Lehman E, Stevens AD, Jackson LP, et al. Cluster analysis of obesity and asthma phenotypes. PLoS One. 2012; 7:e36631. PMID: 22606276.
Article28. Moore WC, Meyers DA, Wenzel SE, Teague WG, Li H, Li X, et al. Identification of asthma phenotypes using cluster analysis in the Severe Asthma Research Program. Am J Respir Crit Care Med. 2010; 181:315–323. PMID: 19892860.
Article29. Amelink M, de Groot JC, de Nijs SB, Lutter R, Zwinderman AH, Sterk PJ, et al. Severe adult-onset asthma: a distinct phenotype. J Allergy Clin Immunol. 2013; 132:336–341. PMID: 23806634.
Article30. Bachert C, van Steen K, Zhang N, Holtappels G, Cattaert T, Maus B, et al. Specific IgE against Staphylococcus aureus enterotoxins: an independent risk factor for asthma. J Allergy Clin Immunol. 2012; 130:376–381.e8. PMID: 22738677.31. Song WJ, Sintobin I, Sohn KH, Kang MG, Park HK, Jo EJ, et al. Staphylococcal enterotoxin IgE sensitization in late-onset severe eosinophilic asthma in the elderly. Clin Exp Allergy. 2016; 46:411–421. PMID: 26436720.
Article32. Morse JC, Li P, Ely KA, Shilts MH, Wannemuehler TJ, Huang LC, et al. Chronic rhinosinusitis in elderly patients is associated with an exaggerated neutrophilic proinflammatory response to pathogenic bacteria. J Allergy Clin Immunol. 2019; 143:990–1002.e6. PMID: 30468775.
Article33. Ulrik CS, Backer V. Nonreversible airflow obstruction in life-long nonsmokers with moderate to severe asthma. Eur Respir J. 1999; 14:892–896. PMID: 10573238.
Article34. ten Brinke AN, Zwinderman AH, Sterk PJ, Rabe KF, Bel EH. Factors associated with persistent airflow limitation in severe asthma. Am J Respir Crit Care Med. 2001; 164:744–748. PMID: 11549526.
Article35. Milanese M, Di Marco F, Corsico AG, Rolla G, Sposato B, Chieco-Bianchi F, et al. Asthma control in elderly asthmatics. An Italian observational study. Respir Med. 2014; 108:1091–1099. PMID: 24958604.
Article36. Garin N, Koyanagi A, Chatterji S, Tyrovolas S, Olaya B, Leonardi M, et al. Global multimorbidity patterns: a cross-sectional, population-based, multi-country study. J Gerontol A Biol Sci Med Sci. 2016; 71:205–214. PMID: 26419978.
Article37. Kauppi P, Kupiainen H, Lindqvist A, Tammilehto L, Kilpeläinen M, Kinnula VL, et al. Overlap syndrome of asthma and COPD predicts low quality of life. J Asthma. 2011; 48:279–285. PMID: 21323613.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Treatment of Severe Asthma
- Seasonality of asthma exacerbation in children caused by respiratory virus infection and allergen sensitization
- Factors Predicting Recovery From Asthma Exacerbations
- New Tread of Association of Rhinovirus and Asthma
- Effects of Obesity and Depression on the Incidence of Asthma in Korean Older Adults: A Secondary Analysis of the Korea National Health and Nutrition Examination Survey 2020