Ann Surg Treat Res.
2020 Mar;98(3):116-123. 10.4174/astr.2020.98.3.116.
Prognostic factors predicting survival rate over 10 years of patients with intrahepatic cholangiocarcinoma after hepatic resection
- Affiliations
-
- 1Department of Surgery, Gangneung Asan Hospital, University of Ulsan College of Medicine, Gangneung, Korea.
- 2Division of Hepatobiliary and Pancreatic Surgery, Department of Surgery, Asan Medical Center, University of Ulsan College of Medicine, Seoul, Korea. hbpsurgeon@gmail.com
- 3Department of Surgery, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- KMID: 2471176
- DOI: http://doi.org/10.4174/astr.2020.98.3.116
Abstract
- PURPOSE
Hepatic resection is considered as the optimal treatment for intrahepatic cholangiocarcinoma (IHCC); however, the survival rate after resection is low and the analysis of long-term (≥10 years) survivors is rare. This study aims to analyze the clinicopathological factors affecting the long-term survival of patients with IHCC.
METHODS
Between January 2003 and December 2012, a single-institution cohort of 429 patients who underwent hepatic resection for IHCC were reviewed retrospectively. Surgical results, recurrence, and survival rates were investigated, and multivariate analyses were performed to identify prognostic factors.
RESULTS
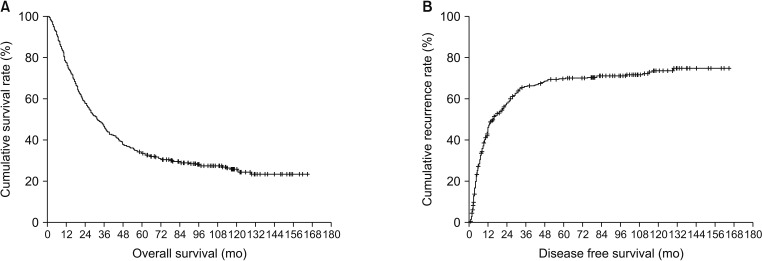
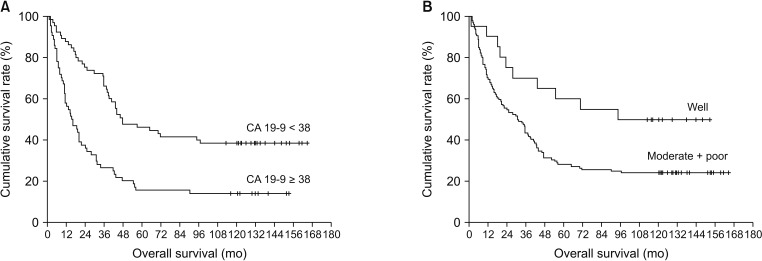
The overall 1- , 3- , 5- and 10-year survival rates of patients were 76.5%, 44.1%, 33.3%, and 25.1%, respectively. Multivariate analysis showed that the serum CA 19-9 level (≥38 U/mL) (P < 0.001), lymph node (LN) metastasis (P = 0.001), and lymphovascular invasion (LVI) (P = 0.012) were independent factors associated with overall survival. In particular, CA 19-9 level and histologic type were determined to be independent factors affecting survival for more than 10 years.
CONCLUSION
CA 19-9 (≥38 U/mL), LN metastasis, and LVI were identified as independent risk factors for survival after resection of IHCC. CA 19-9 (<38 U/mL) and histologic type were independent factors predicting survival for more than 10 years.
Keyword
MeSH Terms
Figure
Reference
-
1. Dodson RM, Weiss MJ, Cosgrove D, Herman JM, Kamel I, Anders R, et al. Intrahepatic cholangiocarcinoma: management options and emerging therapies. J Am Coll Surg. 2013; 217:736–750.e4. PMID: 23890842.
Article2. Khan SA, Toledano MB, Taylor-Robinson SD. Epidemiology, risk factors, and pathogenesis of cholangiocarcinoma. HPB (Oxford). 2008; 10:77–82. PMID: 18773060.
Article3. Poultsides GA, Zhu AX, Choti MA, Pawlik TM. Intrahepatic cholangiocarcinoma. Surg Clin North Am. 2010; 90:817–837. PMID: 20637950.
Article4. Sempoux C, Jibara G, Ward SC, Fan C, Qin L, Roayaie S, et al. Intrahepatic cholangiocarcinoma: new insights in pathology. Semin Liver Dis. 2011; 31:49–60. PMID: 21344350.
Article5. Tan JC, Coburn NG, Baxter NN, Kiss A, Law CH. Surgical management of intrahepatic cholangiocarcinoma--a population-based study. Ann Surg Oncol. 2008; 15:600–608. PMID: 17987347.6. Weimann A, Varnholt H, Schlitt HJ, Lang H, Flemming P, Hustedt C, et al. Retrospective analysis of prognostic factors after liver resection and transplantation for cholangiocellular carcinoma. Br J Surg. 2000; 87:1182–1187. PMID: 10971425.
Article7. Jonas S, Thelen A, Benckert C, Biskup W, Neumann U, Rudolph B, et al. Extended liver resection for intrahepatic cholangiocarcinoma: a comparison of the prognostic accuracy of the fifth and sixth editions of the TNM classification. Ann Surg. 2009; 249:303–309. PMID: 19212186.8. Ribero D, Pinna AD, Guglielmi A, Ponti A, Nuzzo G, Giulini SM, et al. Surgical approach for long-term survival of patients with intrahepatic cholangiocarcinoma: a multi-institutional analysis of 434 patients. Arch Surg. 2012; 147:1107–1113. PMID: 22910846.9. Farges O, Fuks D, Boleslawski E, Le Treut YP, Castaing D, Laurent A, et al. Influence of surgical margins on outcome in patients with intrahepatic cholangiocarcinoma: a multicenter study by the AFC-IHCC-2009 study group. Ann Surg. 2011; 254:824–829. PMID: 22042474.10. Dhanasekaran R, Hemming AW, Zendejas I, George T, Nelson DR, Soldevila-Pico C, et al. Treatment outcomes and prognostic factors of intrahepatic cholangiocarcinoma. Oncol Rep. 2013; 29:1259–1267. PMID: 23426976.
Article11. de Jong MC, Nathan H, Sotiropoulos GC, Paul A, Alexandrescu S, Marques H, et al. Intrahepatic cholangiocarcinoma: an international multi-institutional analysis of prognostic factors and lymph node assessment. J Clin Oncol. 2011; 29:3140–3145. PMID: 21730269.
Article12. Guglielmi A, Ruzzenente A, Campagnaro T, Pachera S, Valdegamberi A, Nicoli P, et al. Intrahepatic cholangiocarcinoma: prognostic factors after surgical resection. World J Surg. 2009; 33:1247–1254. PMID: 19294467.
Article13. Yamashita Y, Taketomi A, Morita K, Fukuhara T, Ueda S, Sanefuji K, et al. The impact of surgical treatment and poor prognostic factors for patients with intrahepatic cholangiocarcinoma: retrospective analysis of 60 patients. Anticancer Res. 2008; 28(4C):2353–2359. PMID: 18751418.14. Yamashita YI, Wang H, Kurihara T, Tsujita E, Nishie A, Imai K, et al. Clinical significances of preoperative classification of intrahepatic cholangiocarcinoma: different characteristics of perihilar vs. peripheral ICC. Anticancer Res. 2016; 36:6563–6569. PMID: 27919984.
Article15. Nuzzo G, Giuliante F, Ardito F, De Rose AM, Vellone M, Clemente G, et al. Intrahepatic cholangiocarcinoma: prognostic factors after liver resection. Updates Surg. 2010; 62:11–19. PMID: 20845096.
Article16. Spolverato G, Kim Y, Alexandrescu S, Marques HP, Lamelas J, Aldrighetti L, et al. Management and outcomes of patients with recurrent intrahepatic cholangiocarcinoma following previous curative-intent surgical resection. Ann Surg Oncol. 2016; 23:235–243. PMID: 26059651.
Article17. Si A, Li J, Xiang H, Zhang S, Bai S, Yang P, et al. Actual over 10-year survival after liver resection for patients with intrahepatic cholangiocarcinoma. Oncotarget. 2017; 8:44521–44532. PMID: 28562348.
Article18. Mavros MN, Economopoulos KP, Alexiou VG, Pawlik TM. Treatment and prognosis for patients with intrahepatic cholang ioc arcinoma: systemat ic review and meta-analysis. JAMA Surg. 2014; 149:565–574. PMID: 24718873.19. Cornwell LB, McMasters KM, Chagpar AB. The impact of lymphovascular invasion on lymph node status in patients with breast cancer. Am Surg. 2011; 77:874–877. PMID: 21944350.
Article20. Guntupalli SR, Zighelboim I, Kizer NT, Zhang Q, Powell MA, Thaker PH, et al. Lymphovascular space invasion is an independent risk factor for nodal disease and poor outcomes in endometrioid endometrial cancer. Gynecol Oncol. 2012; 124:31–35. PMID: 22030404.
Article21. Royston D, Jackson DG. Mechanisms of lymphatic metastasis in human colorectal adenocarcinoma. J Pathol. 2009; 217:608–619. PMID: 19253334.
Article22. Brunocilla E, Pernetti R, Martorana G. The prognostic role of lymphovascular invasion in urothelial-cell carcinoma of upper and lower urinary tract. Anticancer Res. 2011; 31:3503–3506. PMID: 21965769.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Clinical Analysis of Intrahepatic Cholangiocarcinoma
- Review: Analysis of Survival Rate and Prognostic Factors of Intrahepatic Cholangiocarcinoma: 318 Cases in Single Institute
- Prognostic Factors for Intrahepatic Cholangiocarcinoma Treated with Surgical Resection
- Analysis of 50 Consecutive Hepatic Resection Cases for Intrahepatic Cholangiocarcinoma
- A Clinical Review for Resected Intrahepatic Cholangiocarcinoma