Prog Med Phys.
2019 Dec;30(4):112-119. 10.14316/pmp.2019.30.4.112.
Therapeutic Proton Beam Range Measurement with EBT3 Film and Comparison with Tool for Particle Simulation
- Affiliations
-
- 1Department of Radiation Oncology, National Medical Center, Seoul, Korea. nurilee@nmc.or.kr
- 2Proton Therapy Center, National Cancer Center, Goyang, Korea.
- KMID: 2468172
- DOI: http://doi.org/10.14316/pmp.2019.30.4.112
Abstract
- PURPOSE
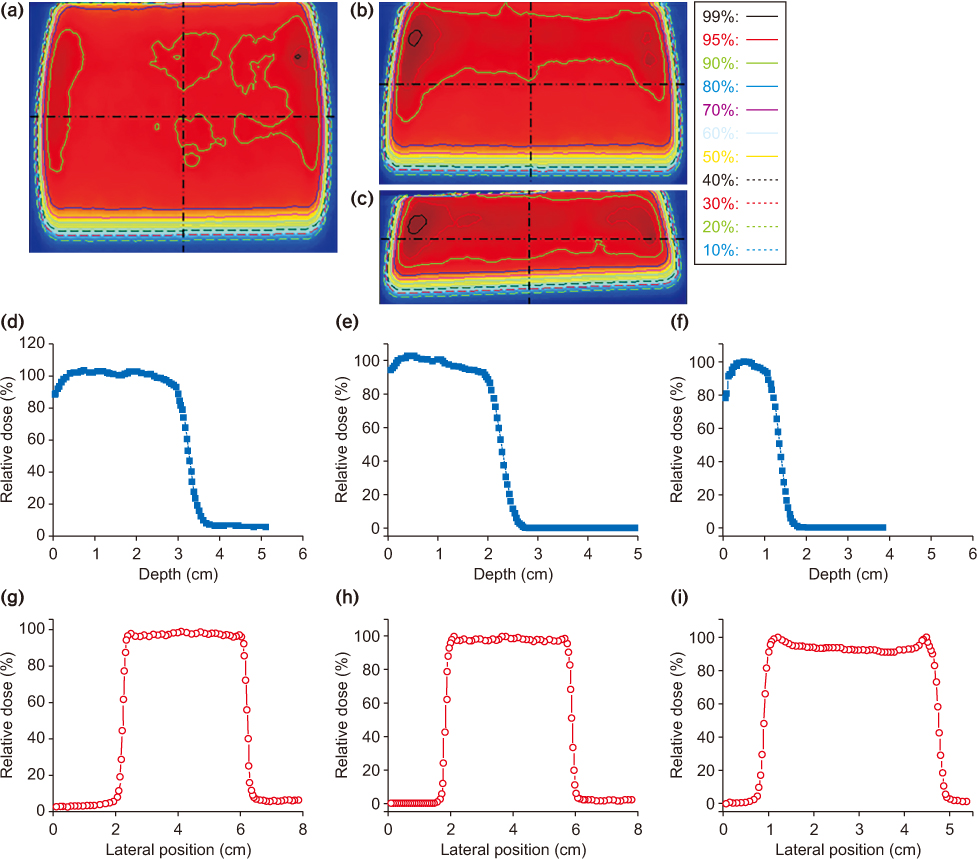
The advantages of ocular proton therapy are that it spares the optic nerve and delivers the minimal dose to normal surrounding tissues. In this study, it developed a solid eye phantom that enabled us to perform quality assurance (QA) to verify the dose and beam range for passive single scattering proton therapy using a single phantom. For this purpose, a new solid eye phantom with a polymethyl-methacrylate (PMMA) wedge was developed using film dosimetry and an ionization chamber.
METHODS
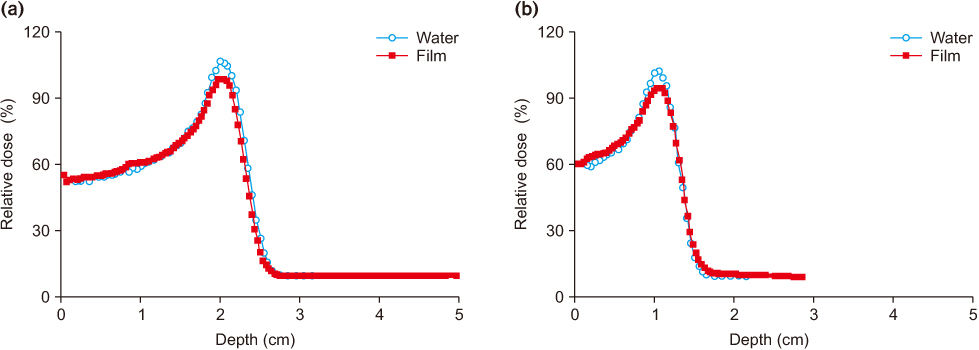
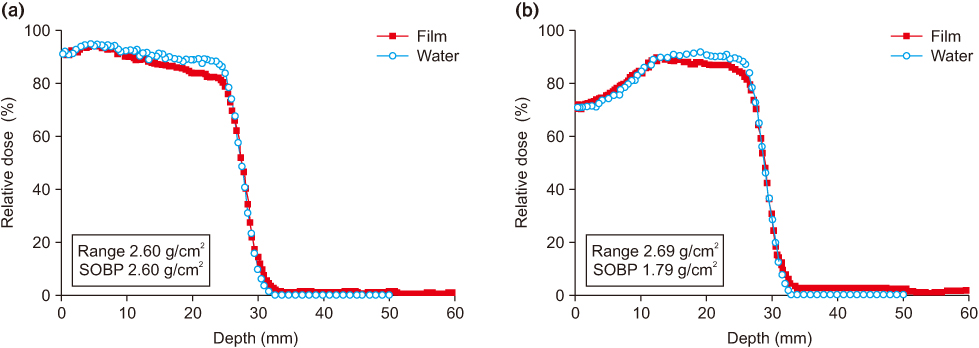
The typical beam shape used for eye treatment is approximately 3 cm in diameter and the beam range is below 5 cm. Since proton therapy has a problem with beam range uncertainty due to differences in the stopping power of normal tissue, bone, air, etc, the beam range should be confirmed before treatment. A film can be placed on the slope of the phantom to evaluate the Spread-out Bragg Peak based on the water equivalent thickness value of PMMA on the film. In addition, an ionization chamber (Pin-point, PTW 31014) can be inserted into a hole in the phantom to measure the absolute dose.
RESULTS
The eye phantom was used for independent patient-specific QA. The differences in the output and beam range between the measurement and the planned treatment were less than 1.5% and 0.1 cm, respectively.
CONCLUSIONS
An eye phantom was developed and the performance was successfully validated. The phantom can be employed to verify the output and beam range for ocular proton therapy.
Keyword
MeSH Terms
Figure
Reference
-
1. Piersimoni P, Rimoldi A, Riccardi C, Pirola M, Molinelli S, Ciocca M. Optimization of a general-purpose, actively scanned proton beamline for ocular treatments: Geant4 simulations. J Appl Clin Med Phys. 2015; 16:261–278.
Article2. Barrett A, Dobbs J. Practical radiotherapy planning. 4th ed. London: Hodder Arnold;2009.3. Gradoudas ES, Goitein M, Koehler A, Constable IJ, Wagner MS, Verhey L, et al. Proton irradiation of choroidal melanomas. Preliminary results. Arch Ophthalmol. 1978; 96:1583–1591.4. Goitein M, Miller T. Planning proton therapy of the eye. Med Phys. 1983; 10:275–283.
Article5. Koch N, Newhauser W. Virtual commissioning of a treatment planning system for proton therapy of ocular cancers. Radiat Prot Dosimetry. 2005; 115:159–163.
Article6. Newhauser W, Koch N, Hummel S, Ziegler M, Titt U. Monte Carlo simulations of a nozzle for the treatment of ocular tumours with high-energy proton beams. Phys Med Biol. 2005; 50:5229–5249.
Article7. Vadrucci M, Esposito G, Ronsivalle C, Cherubini R, Marracino F, Montereali RM, et al. Calibration of GafChromic EBT3 for absorbed dose measurements in 5 MeV proton beam and (60)Co γ-rays. Med Phys. 2015; 42:4678–4684.
Article8. Pai S, Das IJ, Dempsey JF, Lam KL, Losasso TJ, Olch AJ, et al. TG-69: radiographic film for megavoltage beam dosimetry. Med Phys. 2007; 34:2228–2258.
Article9. Sipilä P, Ojala J, Kaijaluoto S, Jokelainen I, Kosunen A. Gafchromic EBT3 film dosimetry in electron beams - energy dependence and improved film read-out. J Appl Clin Med Phys. 2016; 17:360–373.
Article10. Reinhardt S, Hillbrand M, Wilkens JJ, Assmann W. Comparison of Gafchromic EBT2 and EBT3 films for clinical photon and proton beams. Med Phys. 2012; 39:5257–5262.
Article11. Sorriaux J, Kacperek A, Rossomme S, Lee JA, Bertrand D, Vynckier S, et al. Evaluation of Gafchromic® EBT3 films characteristics in therapy photon, electron and proton beams. Phys Med. 2013; 29:599–606.
Article12. Birks JB. Theory and Practice of Scintillation Counting. New York: Pergamon;1964.13. Torrisi L. Plastic scintillator investigations for relative dosimetry in proton-therapy. Nucl Instrum Methods Phys Res, Sec B. 2000; 170:523.
Article14. Wang LL, Perles LA, Archambault L, Sahoo N, Mirkovic D, Beddar S. Determination of the quenching correction factors for plastic scintillation detectors in therapeutic highenergy proton beams. Phys Med Biol. 2012; 57:7767–7781.
Article15. Chung K, Kim J, Kim DH, Ahn S, Han Y. The proton therapy nozzles at Samsung Medical Center: a Monte Carlo simulation study using TOPAS. J Korean Phys Soc. 2015; 67:170–174.
Article16. Zhao L, Das IJ. Gafchromic EBT film dosimetry in proton beams. Phys Med Biol. 2010; 55:N291–N301.
Article17. Vatnitsky SM. Radiochromic film dosimetry for clinical proton beams. Appl Radiat Isot. 1997; 48:643–651.
Article18. Kim DW, Chung WK, Shin J, Lim YK, Shin D, Lee SB, et al. Secondary neutron dose measurement for proton eye treatment using an eye snout with a borated neutron absorber. Radiat Oncol. 2013; 8:182.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Measurement of Proton Beam Dose-Averaged Linear Energy Transfer Using a Radiochromic Film
- Dosimetric Impact of Ti Mesh on Proton Beam Therapy
- Linear Energy Transfer Dependence Correction of Spread-Out Bragg Peak Measured by EBT3 Film for Dynamically Scanned Proton Beams
- A Monte Carlo Simulation Study of a Therapeutic Proton Beam Delivery System Using the Geant4 Code
- Monte Carlo Investigation of Dose Enhancement due to Gold Nanoparticle in Carbon-12, Helium-4, and Proton Beam Therapy