Electrolyte Blood Press.
2019 Dec;17(2):45-53. 10.5049/EBP.2019.17.2.45.
Incidence of Acute Kidney Injury after Adrenalectomy in Patients with Primary Aldosteronism
- Affiliations
-
- 1Department of Internal Medicine, Institute of Kidney Disease Research, Yonsei University College of Medicine, Seoul, Korea. siberian82@yuhs.ac
- 2Division of Nephrology, Soonchunhyang University Hospital, Soonchunhyang University College of Medicine, Seoul, Korea.
- 3Department of Internal Medicine, Severance Biomedical Science Institute, Brain Korea 21 PLUS, Yonsei University College of Medicine, Seoul, Korea.
- KMID: 2467960
- DOI: http://doi.org/10.5049/EBP.2019.17.2.45
Abstract
- BACKGROUND
Aldosterone-induced glomerular hyperfiltration can lead to masked preoperative renal dysfunction in primary aldosteronism(PA) patients. We evaluated whether PA patients had a higher prevalence of acute kidney injury (AKI) after unilateral adrenalectomy. In addition, we identified risk factors for AKI in these subjects.
METHODS
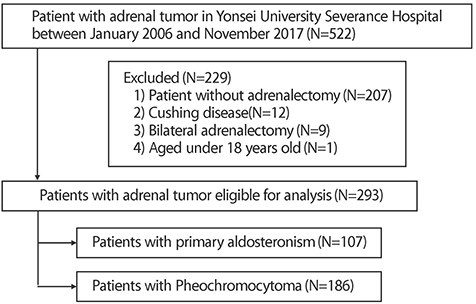
This retrospective study included 107 PA patients, and 186 pheochromocytoma patients as a control group, all of whom underwent adrenalectomy between January 2006 and November 2017 at Yonsei University Severance Hospital. The primary outcome was AKI within 48 hours after adrenalectomy. Univariate and multivariate logistic regression analyses were performed to identify predictors of AKI after adrenalectomy.
RESULTS
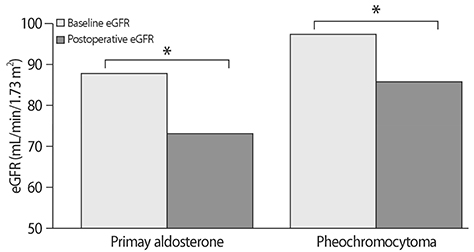
Overall incidence of AKI was 49/293 (16.7%). In PA patients, the incidence of AKI was 29/107 (27.1%). In contrast, incidence of AKI was 20/186 (10.7%) in pheochromocytoma patients. Univariate and multivariate logistic regression analysis both showed a higher risk of postoperative AKI in PA patients compared to pheochromocytoma patients. In addition, old age, diabetes, longer duration of hypertension, lower preoperative estimated glomerular filtration rate, high aldosterone-cortisol ratio (ACR) and lateralization index (LI) were identified as independent risk factors for postoperative AKI in PA patients after unilateral adrenalectomy.
CONCLUSION
Incidence and risk of postoperative AKI were significantly higher in PA patients after surgical treatment. High ACR on the tumor side and high LI were associated with higher risk of AKI in PA patients compared to pheochromocytoma patients.
MeSH Terms
Figure
Reference
-
1. Conn JW. Part I. Painting background. Part II. Primary aldosteronism, a new clinical syndrome, 1954. J Lab Clin Med. 1990; 116(2):253–267.2. Funder JW, Carey RM, Fardella C, et al. Case detection, diagnosis, and treatment of patients with primary aldosteronism: an endocrine society clinical practice guideline. J Clin Endocrinol Metab. 2008; 93(9):3266–3281.
Article3. Monticone S, Sconfienza E, D'Ascenzo F, et al. Renal damage in primary aldosteronism: a systematic review and meta-analysis. J Hypertens. 2020; 38(1):3–12.4. Hung CS, Sung SH, Liao CW, et al. Aldosterone induces vascular damage. Hypertension. 2019; 74(3):623–629.
Article5. Catena C, Colussi G, Sechi LA. Treatment of primary aldosteronism and organ protection. Int J Endocrinol. 2015; 2015:597247.
Article6. Ma TK, Szeto CC. Mineralocorticoid receptor antagonist for renal protection. Ren Fail. 2012; 34(6):810–817.
Article7. Rossi GP, Sacchetto A, Pavan E, et al. Remodeling of the left ventricle in primary aldosteronism due to Conn's adenoma. Circulation. 1997; 95(6):1471–1478.
Article8. Wu VC, Chueh SC, Chang HW, et al. Association of kidney function with residual hypertension after treatment of aldosterone-producing adenoma. Am J Kidney Dis. 2009; 54(4):665–673.
Article9. Tuck ML, Corry DB. Renal damage in primary aldosteronism: results of the PAPY study. Curr Hypertens Rep. 2007; 9(2):87–89. DOI: 10.1007/s11906-007-0016-4.
Article10. Kramers BJ, Kramers C, Lenders JW, Deinum J. Effects of treating primary aldosteronism on renal function. J Clin Hypertens (Greenwich). 2017; 19(3):290–295.
Article11. Stowasser M, Gordon RD, Rutherford JC, Nikwan NZ, Daunt N, Slater GJ. Diagnosis and management of primary aldosteronism. Journal of the Renin-Angiotensin-Aldosterone System. 2001; 2(3):156–169.12. Davison AS, Jones DM, Ruthven S, Helliwell T, Shore SL. Clinical evaluation and treatment of phaeochromocytoma. Annals of Clinical Biochemistry. 2018; 55(1):34–48.
Article13. Schwandt A, Denkinger M, Fasching P, et al. Comparison of MDRD, CKD-EPI, and Cockcroft-Gault equation in relation to measured glomerular filtration rate among a large cohort with diabetes. Journal of Diabetes and its Complications. 2017; 31(9):1376–1383.
Article14. Tanemoto M. Diagnosis of unilateral aldosterone hypersecretion in adrenal venous sampling. J Hypertens. 2019; 37(10):2110.
Article15. Khwaja A. KDIGO clinical practice guidelines for acute kidney injury. Nephron Clin Pract. 2012; 120(4):c179–c184.
Article16. Kim DH, Kwon HJ, Ji SA, et al. Risk factors for renal impairment revealed after unilateral adrenalectomy in patients with primary aldosteronism. Medicine (Baltimore). 2016; 95(27):e3930.
Article17. Kim IY, Park IS, Kim MJ, et al. Change in kidney function after unilateral adrenalectomy in patients with primary aldosteronism: identification of risk factors for decreased kidney function. Int Urol Nephrol. 2018; 50(10):1887–1895.
Article18. Sechi LA, Novello M, Lapenna R, et al. Long-term renal outcomes in patients with primary aldosteronism. JAMA. 2006; 295(22):2638–2645.
Article19. Fogari R, Preti P, Zoppi A, Rinaldi A, Fogari E, Mugellini A. Prevalence of primary aldosteronism among unselected hypertensive patients: a prospective study based on the use of an aldosterone/renin ratio above 25 as a screening test. Hypertens Res. 2007; 30(2):111–117.
Article20. Rossi GP, Bernini G, Caliumi C, et al. A prospective study of the prevalence of primary aldosteronism in 1,125 hypertensive patients. J Am Coll Cardiol. 2006; 48(11):2293–2300.
Article21. Ribstein J, Du Cailar G, Fesler P, Mimran A. Relative glomerular hyperfiltration in primary aldosteronism. J Am Soc Nephrol. 2005; 16(5):1320–1325.
Article22. Utsumi T, Kamiya N, Kaga M, et al. Development of novel nomograms to predict renal functional outcomes after laparoscopic adrenalectomy in patients with primary aldosteronism. World J Urol. 2017; 35(10):1577–1583.
Article23. Utsumi T, Kawamura K, Imamoto T, et al. Preoperative masked renal damage in Japanese patients with primary aldosteronism: identification of predictors for chronic kidney disease manifested after adrenalectomy. Int J Urol. 2013; 20(7):685–691.
Article24. Onohara T, Takagi T, Yoshida K, et al. Assessment of postoperative renal function after adrenalectomy in patients with primary aldosteronism. Int J Urol. 2019; 26(2):229–233.
Article25. Maertens S, Van Den Noortgate N. Kidney in old age. Acta Clinica Belgica. 2008; 63(1):8–15.
Article26. Gargiulo R, Suhail F, Lerma EV. Hypertension and chronic kidney disease. Disease-a-month: DM. 2015; 61(9):387.
Article27. Hamrahian SM. Management of hypertension in patients with chronic kidney disease. Current hypertension reports. 2017; 19(5):43.
Article28. Edeghere S, English P. Management of type 2 diabetes: now and the future. Clin Med (Lond). 2019; 19(5):403–405.
Article29. Zafari N, Churilov L, MacIsaac RJ, et al. Diagnostic performance of the Chronic Kidney Disease Epidemiology Collaboration (CKD-EPI) equation at estimating glomerular filtration rate in adults with diabetes mellitus: a systematic review and meta-analysis protocol. BMJ Open. 2019; 9(8):e031558.
Article30. Hollenberg NK. Aldosterone in the development and progression of renal injury. Kidney Int. 2004; 66(1):1–9.
Article31. Remuzzi G, Cattaneo D, Perico N. The aggravating mechanisms of aldosterone on kidney fibrosis. J Am Soc Nephrol. 2008; 19(8):1459–1462.32. Danforth DN, Orlando MM, Bartter FC, Javadpour N. Renal changes in primary aldosteronism. The Journal of Urology. 1977; 117(2):140–144.
Article33. Brown NJ. Contribution of aldosterone to cardiovascular and renal inflammation and fibrosis. Nat Rev Nephrol. 2013; 9(8):459–469.
Article34. Tomaschitz A, Pilz S, Ritz E, Meinitzer A, Boehm BO, Marz W. Plasma aldosterone levels are associated with increased cardiovascular mortality: the Ludwigshafen Risk and Cardiovascular Health (LURIC) study. Eur Heart J. 2010; 31(10):1237–1247.
Article35. Rocha R, Stier CT Jr. Pathophysiological effects of aldosterone in cardiovascular tissues. Trends Endocrinol Metab. 2001; 12(7):308–314.
Article36. Rossi G, Boscaro M, Ronconi V, Funder JW. Aldosterone as a cardiovascular risk factor. Trends Endocrinol Metab. 2005; 16(3):104–107.
Article37. Steichen O, Amar L. Diagnostic criteria for adrenal venous sampling. Curr Opin Endocrinol Diabetes Obes. 2016; 23(3):218–224.
Article38. Kline G, Holmes DT. Adrenal venous sampling for primary aldosteronism: laboratory medicine best practice. J Clin Pathol. 2017; 70(11):911–916.
Article39. Chen YY, Lin YH, Huang WC, et al. Adrenalectomy improves the long-term risk of end-stage renal disease and mortality of primary aldosteronism. J Endocr Soc. 2019; 3(6):1110–1126.
Article40. Hundemer GL, Curhan GC, Yozamp N, Wang M, Vaidya A. Renal outcomes in medically and surgically treated primary aldosteronism. Hypertension. 2018; 72(3):658–666.
Article41. Li H, Liu J, Liu J, et al. The association between a 24-hour blood pressure pattern and circadian change in plasma aldosterone concentration for patients with aldosterone-producing adenoma. Int J Endocrinol. 2019; 2019:4828402.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Hypertension Controlled by Adrenalectomy: A Case of Primary Aldosteronism
- Factors Associated with Resolution of Hypertension after Adrenalectomy in Patients with Primary Aldosteronism
- Is acute kidney injury after laparoscopic adrenalectomy related to the progression of chronic kidney disease in patients with primary aldosteronism?
- Anesthetic Experience of Adrenalectomy with Primary Aldosteronism
- Primary Aldosteronism: An Anesthetic Experience with Adrenalectomy