J Clin Neurol.
2020 Jan;16(1):140-144. 10.3988/jcn.2020.16.1.140.
Antiphospholipid and Antinuclear Antibodies in Children with Idiopathic Epilepsy: A 2-Year Prospective Study
- Affiliations
-
- 1Third Department of Pediatrics, National and Kapodistrian University of Athens, “Attikon†Hospital, Athens, Greece. attilakos@hotmail.com
- 2Department of Pathophysiology, Faculty of Medicine, National and Kapodistrian University of Athens, Athens, Greece.
- 3Second Department of Pediatrics, National and Kapodistrian University of Athens, “P&A Kyriakou†Children's Hospital, Athens, Greece.
- KMID: 2467796
- DOI: http://doi.org/10.3988/jcn.2020.16.1.140
Abstract
- BACKGROUND AND PURPOSE
The high prevalence of antiphospholipid antibodies (aPL) and antinuclear antibodies (ANA) in patients with epilepsy may be associated with either the disease itself or the antiepileptic treatment. The purpose of this prospective study was to determine the prevalence of aPL and ANA in children with idiopathic epilepsy before and during treatment with antiepileptic drugs.
METHODS
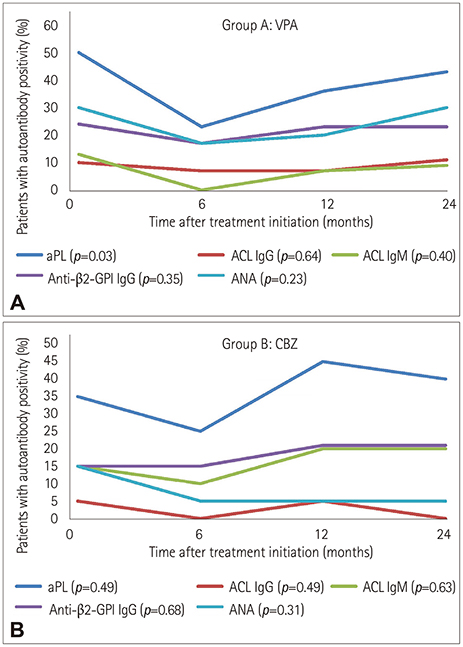
aPL, including both anticardiolipin and anti-β2-glycoprotein I antibodies, and ANA statuses were determined in 40 healthy children, 30 children treated with sodium valproate (VPA) monotherapy, and 20 children treated with carbamazepine (CBZ) monotherapy before and at 6, 12, and 24 months after treatment initiation.
RESULTS
Fifteen children (50%) in the VPA-treated group and 7 (35%) in the CBZ-treated group showed positivity for aPL before treatment initiation, compared with only 4 of the 40 controls. Nine children (30%) in the VPA-treated group and 4 (20%) in the CBZ-treated group showed positivity for ANA before treatment initiation, compared with only 2 of the 40 controls. The subgroup analysis found nonsignificant associations at the different time points regarding the positivity of all of the autoantibodies. Only patients treated with VPA had a significantly decreased risk of aPL positivity after 6 months of treatment.
CONCLUSIONS
The increased prevalence of autoantibodies in children with idiopathic epilepsy is strongly associated with the disease itself.
Keyword
MeSH Terms
-
Antibodies
Antibodies, Antinuclear*
Antibodies, Antiphospholipid
Anticonvulsants
Autoantibodies
beta 2-Glycoprotein I
Carbamazepine
Child*
Epilepsy*
Humans
Prevalence
Prospective Studies*
Valproic Acid
Antibodies
Antibodies, Antinuclear
Antibodies, Antiphospholipid
Anticonvulsants
Autoantibodies
Carbamazepine
Valproic Acid
beta 2-Glycoprotein I
Figure
Reference
-
1. Rumsey DG, Myones B, Massicotte P. Diagnosis and treatment of antiphospholipid syndrome in childhood: a review. Blood Cells Mol Dis. 2017; 67:34–40.
Article2. Agmon-Levin N, Damoiseaux J, Kallenberg C, Sack U, Witte T, Herold M, et al. International recommendations for the assessment of autoantibodies to cellular antigens referred to as anti-nuclear antibodies. Ann Rheum Dis. 2014; 73:17–23.
Article3. Constantin T, Kálovics T, Ponyi A, Nagy E, Sallai K, Szabó L, et al. Prevalence of antiphospholipid and antinuclear antibodies in children with epilepsy. Med Sci Monit. 2009; 15:CR164–CR169.4. Dlott JS, Roubey RA. Drug-induced lupus anticoagulants and antiphospholipid antibodies. Curr Rheumatol Rep. 2012; 14:71–78.
Article5. Brey RL, Muscal E, Chapman J. Antiphospholipid antibodies and the brain: a consensus report. Lupus. 2011; 20:153–157.
Article6. Julian T, Hadjivassiliou M, Zis P. Gluten sensitivity and epilepsy: a systematic review. J Neurol. 2019; 266:1557–1565.
Article7. Verrot D, San-Marco M, Dravet C, Genton P, Disdier P, Bolla G, et al. Prevalence and signification of antinuclear and anticardiolipin antibodies in patients with epilepsy. Am J Med. 1997; 103:33–37.
Article8. Peltola JT, Haapala A, Isojärvi JI, Auvinen A, Palmio J, Latvala K, et al. Antiphospholipid and antinuclear antibodies in patients with epilepsy or new-onset seizure disorders. Am J Med. 2000; 109:712–717.
Article9. Eriksson K, Peltola J, Keränen T, Haapala AM, Koivikko M. High prevalence of antiphospholipid antibodies in children with epilepsy: a controlled study of 50 cases. Epilepsy Res. 2001; 46:129–137.
Article10. Specchio N, Fusco L, Claps D, Vigevano F. Epileptic encephalopathy in children possibly related to immune-mediated pathogenesis. Brain Dev. 2010; 32:51–56.
Article11. Arnson Y, Shoenfeld Y, Alon E, Amital H. The antiphospholipid syndrome as a neurological disease. Semin Arthritis Rheum. 2010; 40:97–108.
Article12. Angelini L, Granata T, Zibordi F, Binelli S, Zorzi G, Besana C. Partial seizures associated with antiphospholipid antibodies in childhood. Neuropediatrics. 1998; 29:249–253.
Article13. Cimaz R, Romeo A, Scarano A, Avcin T, Viri M, Veggiotti P, et al. Prevalence of anti-cardiolipin, anti-β2 glycoprotein I, and anti-prothrombin antibodies in young patients with epilepsy. Epilepsia. 2002; 43:52–59.
Article14. Graf J. Central nervous system manifestations of antiphospholipid syndrome. Rheum Dis Clin North Am. 2017; 43:547–560.
Article15. Liimatainen S, Peltola M, Fallah M, Kharazmi E, Haapala AM, Peltola J. The high prevalence of antiphospholipid antibodies in refractory focal epilepsy is related to recurrent seizures. Eur J Neurol. 2009; 16:134–141.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Antiphospholipid Syndrome Presented with Pulmonary Embolism and Deep Venous Thrombosis in Child
- Antiphospholipid Antibody Syndrome
- Bilateral Central Retinal Vein Occlusion in Primary Antiphospholipid Syndrome
- A case of primary antiphospholipid antibody syndrome showing vegetation on the mitral valve through echocardiography
- Brachial Artery Thrombosis in an 8-year-old Boy with Antiphospholipid Antibodies Induced by Mycoplasma pneumoniae Infection: a Case Report