Risk Factors for Pancreatitis and Cholecystitis after Endoscopic Biliary Stenting in Patients with Malignant Extrahepatic Bile Duct Obstruction
- Affiliations
-
- 1Department of Medicine, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea.
- 2Department of Gastroenterology, Samsung Medical Center, Sungkyunkwan University School of Medicine, Seoul, Korea. jongk.lee@samsung.com
- KMID: 2465803
- DOI: http://doi.org/10.5946/ce.2018.177
Abstract
- BACKGROUND/AIMS
For the treatment of malignant biliary obstruction, endoscopic retrograde biliary drainage (ERBD) has been widely accepted as a standard procedure. However, post-ERBD complications can affect the lives of patients. The purpose of this study was to identify the predictive factors for these complications, including the patient's status, cancer status, and stent type.
METHODS
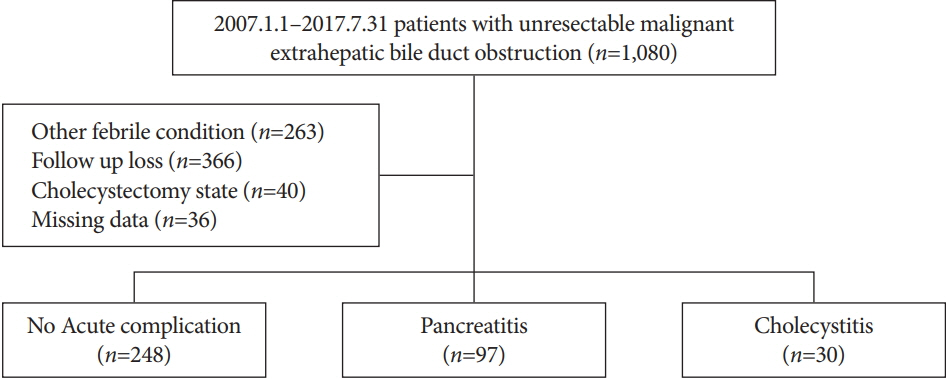
This was a retrospective analysis conducted in a single tertiary hospital from January 2007 to July 2017. The following variables were evaluated: sex, age, body mass index, cancer type, history of pancreatitis, gallbladder stone, previous biliary stenting, precut papillotomy, stent type, contrast injection into the pancreatic duct or gallbladder, cystic duct invasion by the tumor, and occlusion of the cystic duct orifice by a metal stent.
RESULTS
Multivariate analysis showed that contrast injection into the pancreatic duct was a risk factor for pancreatitis. Patients with a history of bile drainage showed a lower risk of pancreatitis. For cholecystitis, the analysis revealed contrast injection into the gallbladder and cystic duct invasion by the tumor as important predictive factors. Metal stents showed a greater risk of post-procedure pancreatitis than plastic stents, but did not affect the incidence of cholecystitis.
CONCLUSIONS
Considering that contrast injection is the most important factor for both complications, a careful approach by the physician is essential in preventing the occurrence of any complications. Further, choosing the type of stent is an important factor for patients at a risk of post-procedure pancreatitis.
MeSH Terms
Figure
Cited by 4 articles
-
Cholecystitis after Placement of Covered Self-Expandable Metallic Stents in Patients with Distal Malignant Biliary Obstructions
Masafumi Watanabe, Kosuke Okuwaki, Jun Woo, Mitsuhiro Kida, Hiroshi Imaizumi, Tomohisa Iwai, Hiroshi Yamauchi, Toru Kaneko, Rikiya Hasegawa, Takahiro Kurosu, Naoki Minato, Hiroki Haradome, Wasaburo Koizumi
Clin Endosc. 2021;54(4):589-595. doi: 10.5946/ce.2020.136.Strategies to Overcome Risks Associated with Endoscopic Biliary Stenting
Woo Hyun Paik, Yong-Tae Kim
Clin Endosc. 2019;52(6):525-526. doi: 10.5946/ce.2019.197.The feasibility of percutaneous transhepatic gallbladder aspiration for acute cholecystitis after self-expandable metallic stent placement for malignant biliary obstruction: a 10-year retrospective analysis in a single center
Akihisa Ohno, Nao Fujimori, Toyoma Kaku, Masayuki Hijioka, Ken Kawabe, Naohiko Harada, Makoto Nakamuta, Takamasa Oono, Yoshihiro Ogawa
Clin Endosc. 2022;55(6):784-792. doi: 10.5946/ce.2021.244.How should a therapeutic strategy be constructed for acute cholecystitis after self-expanding metal stent placement for malignant biliary obstruction?
Mamoru Takenaka, Masatoshi Kudo
Clin Endosc. 2022;55(6):757-759. doi: 10.5946/ce.2022.275.
Reference
-
1. Smith AC, Dowsett JF, Russell RC, Hatfield AR, Cotton PB. Randomised trial of endoscopic stenting versus surgical bypass in malignant low bileduct obstruction. Lancet. 1994; 344:1655–1660.2. ASGE Technology Assessment Committee, Pfau PR, Pleskow DK, et al. Pancreatic and biliary stents. Gastrointest Endosc. 2013; 77:319–327.
Article3. Isayama H, Kawabe T, Nakai Y, et al. Cholecystitis after metallic stent placement in patients with malignant distal biliary obstruction. Clin Gastroenterol Hepatol. 2006; 4:1148–1153.
Article4. Isayama H, Komatsu Y, Tsujino T, et al. A prospective randomised study of “covered” versus “uncovered” diamond stents for the management of distal malignant biliary obstruction. Gut. 2004; 53:729–734.
Article5. Sawas T, Al Halabi S, Parsi MA, Vargo JJ. Self-expandable metal stents versus plastic stents for malignant biliary obstruction: a meta-analysis. Gastrointest Endosc. 2015; 82:256–267.e7.
Article6. Isayama H, Nakai Y, Kawakubo K, et al. Covered metallic stenting for malignant distal biliary obstruction: clinical results according to stent type. J Hepatobiliary Pancreat Sci. 2011; 18:673–677.
Article7. Saleem A, Leggett CL, Murad MH, Baron TH. Meta-analysis of randomized trials comparing the patency of covered and uncovered self-expandable metal stents for palliation of distal malignant bile duct obstruction. Gastrointest Endosc. 2011; 74:321–327.e1-e3.
Article8. Minami Y, Kudo M. Hepatocellular carcinoma with obstructive jaundice: endoscopic and percutaneous biliary drainage. Dig Dis. 2012; 30:592–597.
Article9. Almadi MA, Barkun AN, Martel M. No benefit of covered vs uncovered self-expandable metal stents in patients with malignant distal biliary obstruction: a meta-analysis. Clin Gastroenterol Hepatol. 2013; 11:27–37.e1.
Article10. Jang S, Stevens T, Parsi M, et al. Association of covered metallic stents with cholecystitis and stent migration in malignant biliary stricture. Gastrointest Endosc. 2018; 87:1061–1070.11. Kawakubo K, Isayama H, Nakai Y, et al. Risk factors for pancreatitis following transpapillary self-expandable metal stent placement. Surg Endosc. 2012; 26:771–776.
Article12. Shimizu S, Naitoh I, Nakazawa T, et al. Predictive factors for pancreatitis and cholecystitis in endoscopic covered metal stenting for distal malignant biliary obstruction. J Gastroenterol Hepatol. 2013; 28:68–72.
Article13. Prat F, Chapat O, Ducot B, et al. A randomized trial of endoscopic drainage methods for inoperable malignant strictures of the common bile duct. Gastrointest Endosc. 1998; 47:1–7.
Article14. Kaassis M, Boyer J, Dumas R, et al. Plastic or metal stents for malignant stricture of the common bile duct? Results of a randomized prospective study. Gastrointest Endosc. 2003; 57:178–182.
Article15. Gukovsky I, Li N, Todoric J, Gukovskaya A, Karin M. Inflammation, autophagy, and obesity: common features in the pathogenesis of pancreatitis and pancreatic cancer. Gastroenterology. 2013; 144:1199–1209.e4.
Article16. Pan XP, Dang T, Meng XM, Xue KC, Chang ZH, Zhang YP. Clinical study on the prevention of post-ERCP pancreatitis by pancreatic duct stenting. Cell Biochem Biophys. 2011; 61:473–479.
Article17. Ito K, Fujita N, Kanno A, et al. Risk factors for post-ERCP pancreatitis in high risk patients who have undergone prophylactic pancreatic duct stenting: a multicenter retrospective study. Intern Med. 2011; 50:2927–2932.
Article18. Suk KT, Kim HS, Kim JW, et al. Risk factors for cholecystitis after metal stent placement in malignant biliary obstruction. Gastrointest Endosc. 2006; 64:522–529.
Article19. Tsujino T, Kawabe T, Isayama H, et al. Management of late biliary complications in patients with gallbladder stones in situ after endoscopic papillary balloon dilation. Eur J Gastroenterol Hepatol. 2009; 21:376–380.
Article20. Tarnasky PR, Cunningham JT, Hawes RH, et al. Transpapillary stenting of proximal biliary strictures: does biliary sphincterotomy reduce the risk of postprocedure pancreatitis? Gastrointest Endosc. 1997; 45:46–51.
Article21. Sofi AA, Nawras A, Alaradi OH, Alastal Y, Khan MA, Lee WM. Does endoscopic sphincterotomy reduce the risk of post-endoscopic retrograde cholangiopancreatography pancreatitis after biliary stenting? A systematic review and meta-analysis. Dig Endosc. 2016; 28:394–404.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Percutaneous Endoscopic Biliary Stenting
- Helical CT Cholangiography with Multiplanar Reformation: Utility in Patients with Extrahepatic Biliary Obstruction
- Biliary Web: A Rare Cause of Extrahepatic Biliary Obstruction
- Usefulness of Endoscopic Brush Cytology from Malignant Biliary Obstruction
- The Role of MRCP in the Diagnosis of Extrahepatic Bile Duct Cancer : Comparison with EBCP