Anesth Pain Med.
2019 Oct;14(4):460-464. 10.17085/apm.2019.14.4.460.
Use of methylene blue in vasoplegic syndrome that developed during non-cardiac surgery: A case report
- Affiliations
-
- 1Department of Anesthesiology and Pain Medicine, Kyung Hee University College of Medicine, Seoul, Korea. choikhang@gmail.com
- KMID: 2465346
- DOI: http://doi.org/10.17085/apm.2019.14.4.460
Abstract
- BACKGROUND
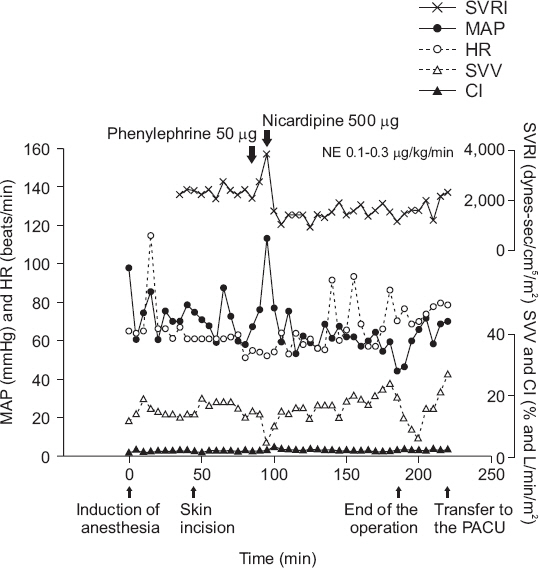
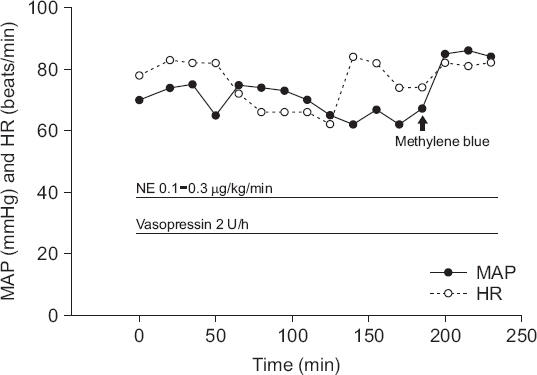
Vasoplegic syndrome is an increasingly recognized disease in perioperative medicine and is characterized by severe hypotension, normal or elevated cardiac output, and decreased systemic vascular resistance. It occurs commonly after cardiopulmonary bypass but may also occur after other types of surgery. CASE: Vasoplegic syndrome developed in our patient during posterior lumbar interbody fusion because of administering nicardipine after phenylephrine. However, the blood pressure did not increase as expected despite simultaneous use of norepinephrine and vasopressin to increase the reduced systemic vascular resistance.
CONCLUSIONS
We present a case of vasoplegic syndrome that developed during posterior lumbar interbody fusion and was treated successfully with methylene blue.
Keyword
MeSH Terms
Figure
Reference
-
1. Gomes WJ, Carvalho AC, Palma JH, Gonçalves I Jr, Buffolo E. Vasoplegic syndrome:a new dilemma. J Thorac Cardiovasc Surg. 1994; 107:942–3. PMID: 8127127.2. Mekontso-Dessap A, Houël R, Soustelle C, Kirsch M, Thébert D, Loisance DY. Risk factors for post-cardiopulmonary bypass vasoplegia in patients with preserved left ventricular function. Ann Thorac Surg. 2001; 71:1428–32. DOI: 10.1016/S0003-4975(01)02486-9. PMID: 11383777.3. Levy B, Fritz C, Tahon E, Jacquot A, Auchet T, Kimmoun A. Vasoplegia treatments:the past, the present, and the future. Crit Care. 2018; 22:52. DOI: 10.1186/s13054-018-1967-3. PMID: 29486781. PMCID: PMC6389278.4. Omar S, Zedan A, Nugent K. Cardiac vasoplegia syndrome:pathophysiology, risk factors and treatment. Am J Med Sci. 2015; 349:80–8. DOI: 10.1097/MAJ.0000000000000341. PMID: 25247756.5. McCartney SL, Duce L, Ghadimi K. Intraoperative vasoplegia:methylene blue to the rescue! Curr Opin Anaesthesiol. 2018; 31:43–9. DOI: 10.1097/ACO.0000000000000548. PMID: 29176374.6. Liu H, Yu L, Yang L, Green MS. Vasoplegic syndrome:an update on perioperative considerations. J Clin Anesth. 2017; 40:63–71. DOI: 10.1016/j.jclinane.2017.04.017. PMID: 28625450.7. Lambden S, Creagh-Brown BC, Hunt J, Summers C, Forni LG. Definitions and pathophysiology of vasoplegic shock. Crit Care. 2018; 22:174. DOI: 10.1186/s13054-018-2102-1. PMID: 29980217. PMCID: PMC6035427.8. Dhein S, Salameh A, Berkels R, Klaus W. Dual mode of action of dihydropyridine calcium antagonists:a role for nitric oxide. Drugs. 1999; 58:397–404. DOI: 10.2165/00003495-199958030-00002. PMID: 10493269.9. Berkels R, Taubert D, Bartels H, Breitenbach T, Klaus W, Roesen R. Amlodipine increases endothelial nitric oxide by dual mechanisms. Pharmacology. 2004; 70:39–45. DOI: 10.1159/000074241. PMID: 14646355.10. Russell JA, Walley KR, Singer J, Gordon AC, Hébert PC, Cooper DJ, et al. Vasopressin versus norepinephrine infusion in patients with septic shock. N Engl J Med. 2008; 358:877–87. DOI: 10.1056/NEJMoa067373. PMID: 18305265.11. Levin RL, Degrange MA, Bruno GF, Del Mazo CD, Taborda DJ, Griotti JJ, et al. Methylene blue reduces mortality and morbidity in vasoplegic patients after cardiac surgery. Ann Thorac Surg. 2004; 77:496–9. DOI: 10.1016/S0003-4975(03)01510-8. PMID: 14759425.12. Maslow AD, Stearns G, Butala P, Schwartz CS, Gough J, Singh AK. The hemodynamic effects of methylene blue when administered at the onset of cardiopulmonary bypass. Anesth Analg. 2006; 103:2–8. DOI: 10.1213/01.ane.0000221261.25310.fe. PMID: 16790616.13. Ozal E, Kuralay E, Yildirim V, Kilic S, Bolcal C, Kücükarslan N, et al. Preoperative methylene blue administration in patients at high risk for vasoplegic syndrome during cardiac surgery. Ann Thorac Surg. 2005; 79:1615–9. DOI: 10.1016/j.athoracsur.2004.10.038. PMID: 15854942.14. Fischer GW, Levin MA. Vasoplegia during cardiac surgery:current concepts and management. Semin Thorac Cardiovasc Surg. 2010; 22:140–4. DOI: 10.1053/j.semtcvs.2010.09.007. PMID: 21092891.15. Faber P, Ronald A, Millar BW. Methylthioninium chloride:pharmacology and clinical applications with special emphasis on nitric oxide mediated vasodilatory shock during cardiopulmonary bypass. Anaesthesia. 2005; 60:575–87. DOI: 10.1111/j.1365-2044.2005.04185.x. PMID: 15918829.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Restoration of Blood Pressure after Administering Methylene Blue for Vasoplegic Syndrome, which Developed after Open Heart Surgery for Septic Infective Endocarditis: A case report
- Methylene Blue for Vasoplegic Syndrome after Cardiopulmonary Bypass: A case report
- Skin Flap Necrosis by Bone Marking with Methylene Blue in Cochlear Implantation
- Effects of methylene blue or evan's blue on mouse embryo development, human sperm motility, serum E2 level and components of human intra tubal fluid
- Hysteroscopic Septotomy of a Complete Septate Uterus Using a Balloon with Methylene Blue