Ann Surg Treat Res.
2019 Dec;97(6):302-308. 10.4174/astr.2019.97.6.302.
Clinical significance and characteristics of left-sided gallbladder: case series study of 10 patients
- Affiliations
-
- 1Department of Surgery, Gachon University Gil Medical Center, Gachon University School of Medicine, Incheon, Korea. drkdj@gilhospital.com
- 2Department of Surgery, Hallym University Kangdong Sacred Heart Hospital, Hallym University School of Medicine, Seoul, Korea.
- KMID: 2464786
- DOI: http://doi.org/10.4174/astr.2019.97.6.302
Abstract
- PURPOSE
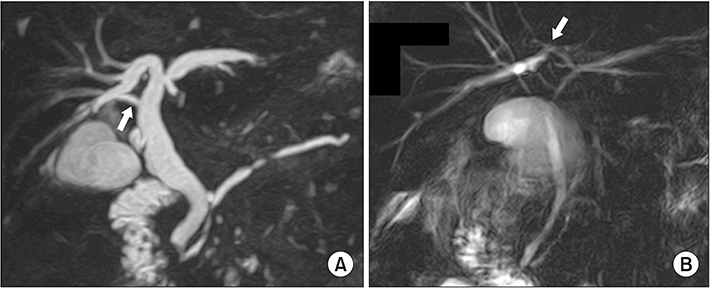
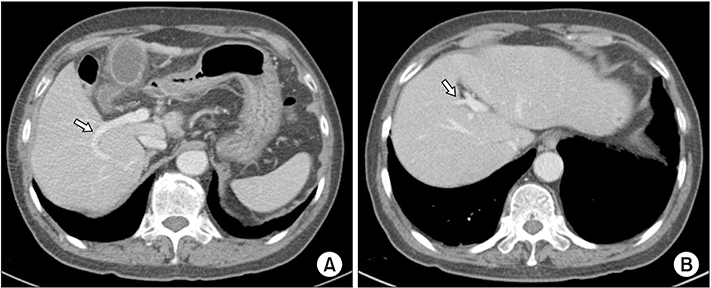
The aims of this case series study were to review the 10 patients who were diagnosed with left-sided gallbladder and analyze their anatomic variations in the bile duct, portal vein, and hepatic vessels.
METHODS
In this case series study, 10 patients with left-sided gallbladder were retrospectively analyzed at 2 tertiary referral centers between April 2004 and May 2019.
RESULTS
Mean age was 61.1 years; there were 7 women and 3 men. Ten patients underwent laparoscopic cholecystectomy for acute cholecystitis or symptomatic gallbladder stone. The mean operation time was 77.2 minutes. Three ports were used in laparoscopic cholecystectomy procedures. The mean postoperative hospital stay was 3.5 days, and there were no cases of surgery-related morbidity. Two patients had type 1 bile duct and 3 had type 3 bile duct (2 type 3B and 1 type 3A). The right posterior portal vein as the first branch of the main portal vein was observed in all patients. Segment IV branches of the left portal vein crossing over to the segment VIII territory were observed in 7 of the 10 patients.
CONCLUSION
Although left-sided gallbladder is a very rare disease, it is possible to diagnose it preoperatively and perform laparoscopic cholecystectomy safely by adjusting port position. The common important features of left-sided gallbladder include distribution of the left portal vein crossing over to the right side of the liver and increased size of the left portal vein. These variations may have important clinical implications in the management of hepatic resection including donor hepatectomy.
MeSH Terms
Figure
Reference
-
1. Zografos GC, Lagoudianakis EE, Grosomanidis D, Koronakis N, Tsekouras D, Chrysikos J, et al. Management of incidental left-sided gallbladder. JSLS. 2009; 13:273–275.2. Idu M, Jakimowicz J, Iuppa A, Cuschieri A. Hepatobiliary anatomy in patients with transposition of the gallbladder: implications for safe laparoscopic cholecystectomy. Br J Surg. 1996; 83:1442–1443.3. Nagai M, Kubota K, Kawasaki S, Takayama T, BandaiY , Makuuchi M. Are left-sided gallbladders really located on the left side? Ann Surg. 1997; 225:274–280.4. Maetani Y, Itoh K, Kojima N, Tabuchi T, Shibata T, Asonuma K, et al. Portal vein anomaly associated with deviation of the ligamentum teres to the right and malposition of the gallbladder. Radiology. 1998; 207:723–728.5. Hsu SL, Chen TY, Huang TL, Sun CK, Concejero AM, Tsang LL, et al. Left-sided gallbladder: its clinical significance and imaging presentations. World J Gastroenterol. 2007; 13:6404–6409.6. Colovic R, Colovic N, Barisic G, Atkinson HD, Krivokapic Z. Left-sided gallbladder associated with congenital liver cyst. HPB (Oxford). 2006; 8:157–158.7. Rao PG, Katariya RN, Sood S, Rao PL. Situs inversus totalis with calculus cholecystitis and mucinous cystadenomas of ovaries. J Postgrad Med. 1977; 23:89–90.8. Schachner A. Anomalies of the gall-bladder and bile-passages: with the report of a double gall-bladder and a floating gallbladder. Ann Surg. 1916; 64:419–433.9. Hay SA, Soliman HE, Sherif HM, Abdelrahman AH, Kabesh AA, Hamza AF. Neonatal jaundice: the role of laparoscopy. J Pediatr Surg. 2000; 35:1706–1709.10. Korn O, Csendes A, Bastías J. Anomalies of extrahepatic biliary duct and gallbladder associated with intestinal malrotation: a case report. Surgery. 1988; 103:496–498.11. Matsusue S, Kashihara S, Koizumi S. Pancreatectomy for carcinoma of the head of the pancreas associated with multiple anomalies including the preduodenal portal vein. Jpn J Surg. 1984; 14:394–398.12. Hunter JG. Exposure, dissection, and laser versus electrosurgery in laparoscopic cholecystectomy. Am J Surg. 1993; 165:492–496.13. Choi JW, Kim TK, Kim KW, Kim AY, Kim PN, Ha HK, et al. Anatomic variation in intrahepatic bile ducts: an analysis of intraoperative cholangiograms in 300 consecutive donors for living donor liver transplantation. Korean J Radiol. 2003; 4:85–90.14. Koc Z, Oguzkurt L, Ulusan S. Portal vein variations: clinical implications and frequencies in routine abdominal multidetector CT. Diagn Interv Radiol. 2007; 13:75–80.15. De Cecchis L, Hribernik M, Ravnik D, Gadzijev EM. Anatomical variations in the pattern of the right hepatic veins: possibilities for type classification. J Anat. 2000; 197 Pt 3:487–493.16. Ding GQ, Cai W, Qin MF. Is intraoperative cholangiography necessary during laparoscopic cholecystectomy for cholelithiasis? World J Gastroenterol. 2015; 21:2147–2151.17. Kim NS, Jin HY, Kim EY, Hong TH. Cystic duct variation detected by near-infrared fluorescent cholangiography during laparoscopic cholecystectomy. Ann Surg Treat Res. 2017; 92:47–50.18. Horwood J, Akbar F, Davis K, Morgan R. Prospective evaluation of a selective approach to cholangiography for suspected common bile duct stones. Ann R Coll Surg Engl. 2010; 92:206–210.19. Brown LM, Rogers SJ, Cello JP, Brasel KJ, Inadomi JM. Cost-effective treatment of patients with symptomatic cholelithiasis and possible common bile duct stones. J Am Coll Surg. 2011; 212:1049–1060.e1-7.20. Lee DH, Ahn YJ, Lee HW, Chung JK, Jung IM. Prevalence and characteristics of clinically significant retained common bile duct stones after laparoscopic cholecystectomy for symptomatic cholelithiasis. Ann Surg Treat Res. 2016; 91:239–246.21. Almodhaiberi H, Hwang S, Cho YJ, Kwon Y, Jung BH, Kim MH. Customized left-sided hepatectomy and bile duct resection for perihilar cholangiocarcinoma in a patient with left-sided gallbladder and multiple combined anomalies. Korean J Hepatobiliary Pancreat Surg. 2015; 19:30–34.22. Kaneoka Y, Yamaguchi A, Isogai M, Harada T. Hepatectomy for cholangiocarcinoma complicated with right umbilical portion: anomalous configuration of the intrahepatic biliary tree. J Hepatobiliary Pancreat Surg. 2000; 7:321–326.23. Shimizu T, Hayashi M, Inoue Y, Komeda K, Asakuma M, Hirokawa F, et al. Living-donor liver transplantation from donor with a left-sided gallbladder with portal vein anomaly. Transplantation. 2012; 94:e60–e61.24. Hwang S, Lee SG, Park KM, Lee YJ, Ahn CS, Kim KH, et al. Hepatectomy of living donors with a left-sided gallbladder and multiple combined anomalies for adult-to-adult living donor liver transplantation. Liver Transpl. 2004; 10:141–146.25. Rocca JP, Rodriguez-Davalos MI, Burke-Davis M, Marvin MR, Sheiner PA, Facciuto ME. Living-donor hepatectomy in right-sided round-ligament liver: importance of mapping the anatomy to the left medial segment. J Hepatobiliary Pancreat Surg. 2006; 13:454–457.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Left-sided Gallbladder: 2 cases
- Laparoscopic cholecystectomy and common bile duct exploration for gallstone and common bile duct stone in a patient with a left-sided gallbladder: a case report
- Preduodenal Portal Vein and Left Sided Gallbladder in Hepatolithiasis Patient: A case report
- Laparoscopic Cholecystectomy in Patients with a Left-sided Gallbladder
- Left-sided Gallbladder with Intrahepatic Portal Vein Anomalies: A Single Center Experiences