Infect Chemother.
2019 Sep;51(3):256-262. 10.3947/ic.2019.51.3.256.
Investigation of a Mumps Outbreak in a Dental Clinic at a University Hospital
- Affiliations
-
- 1Division of Infectious Diseases, Department of Internal Medicine, Pusan National University Hospital, Busan, Korea. kyehyungs@gmail.com
- 2Department of Laboratory Medicine, Pusan National University Hospital, Busan, Korea.
- 3Biomedical Research Institute, Pusan National University Hospital, Busan, Korea.
- KMID: 2459041
- DOI: http://doi.org/10.3947/ic.2019.51.3.256
Abstract
- BACKGROUND
The Korean Society of Infectious Diseases recommends non-mandatory vaccination of newly employed healthcare workers (HCWs) with 2 measles-mumps-rubella (MMR) vaccine doses. Here, we aimed to investigate the seroprevalence of mumps among HCWs exposed to index patients with mumps and the efficacy of MMR vaccination as postexposure prophylaxis (PEP) when a mumps outbreak was encountered among HCWs in a tertiary university hospital in Korea.
MATERIALS AND METHODS
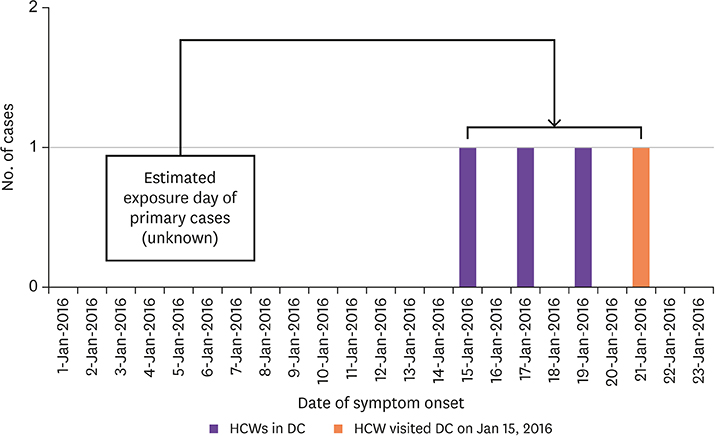
Four HCWs were diagnosed with mumps over a 4-day period in January 2016. Three were working at a dental clinic and one visited the clinic on the day of symptoms onset of the first patient. We investigated all HCWs who either worked in that dental clinic, visited the clinic, or being within 1.5 meter of the patients with mumps without wearing surgical masks. Seventy HCWs were exposed to 4 HCWs with mumps. We interviewed all the exposed HCWs to investigate mumps infection and MMR vaccination history; they were all tested for mumps IgG.
RESULTS
Of the 70 exposed HCWs, 56 (80%) were females; the median age was 34 years (range 21-59 years) and 3 had a history of mumps infection. The vaccination status verification of mumps among the HCWs was unavailable. As for serologic testing, 54 (77.1%) were seropositive. Seropositivity rate for the mumps virus in males was significantly lower than that in females (50.0% vs. 83.9% respectively, P = 0.007). A lower seroprevalence of mumps was observed among HCWs aged ≥40 years than those aged <40 years; however, this difference was not significant (65.2% vs. 83.0%, P = 0.096). During the initial intervention, all exposed HCWs were vaccinated because the turnaround time for serologic testing was expected to be >2 days. Thirty-four (62.9%) of 54 seropositive HCWs and 16 seronegative HCWs were administered MMR vaccines as PEP and following this, no additional cases of mumps were encountered during the maximum incubation period.
CONCLUSION
Of the exposed HCWs, 77.1% were mumps-seropositive. Seropositive rates differed according to factors such as age and sex. Eligible HCWs received a MMR vaccine as PEP and no additional mumps cases occurred during the incubation period. It was useful in our infection control activities during the mumps outbreak.
MeSH Terms
Figure
Reference
-
1. Choi KM. Reemergence of mumps. Korean J Pediatr. 2010; 53:623–628.
Article2. Munkhjargal I, Selenge J, Ambaselmaa A, Tuul R, Delgermaa P, Amarzaya S, Baigalmaa J, Byambajav B, Luo D. Investigation of a mumps outbreak in Mongolia, January to April 2011. Western Pac Surveill Response J. 2012; 3:53–58.
Article3. Bonebrake AL, Silkaitis C, Monga G, Galat A, Anderson J, Trad JT, Hedley K, Burgess N, Zembower TR. Effects of mumps outbreak in hospital, Chicago, Illinois, USA, 2006. Emerg Infect Dis. 2010; 16:426–432.
Article4. Fiebelkorn AP, Lawler J, Curns AT, Brandeburg C, Wallace GS. Mumps postexposure prophylaxis with a third dose of measles-mumps-rubella vaccine, Orange County, New York, USA. Emerg Infect Dis. 2013; 19:1411–1417.
Article5. Park SH. Resurgence of mumps in Korea. Infect Chemother. 2015; 47:1–11.
Article6. Choi WS, Sniadack DH, Jee Y, Go UY, So JS, Cho H, Bae GR, Lee DH, Kim K, Yoon HS, Chung YS, Kang C, Park H, Park O, Lee JK. Outbreak of measles in the Republic of Korea, 2007: importance of nosocomial transmission. J Infect Dis. 2011; 204:Suppl 1. S483–S490.
Article7. Choe YH, Kim BN. Measle-mumps-rubella. Korean Society of Infectious Diseases. Vaccination for adult. 2nd ed. Seoul: MIP;2012. p. 236–253.8. DiaSorin. LIAISON® Mumps IgG, 2019. Accessed 3 September 2019. Available at: https://www.diasorin.com/sites/default/files/allegati_prodotti/scheda_mumps_igg.pdf.9. Choe YJ, Jee Y, Oh MD, Lee JK. Measles Elimination Activities in the Western Pacific Region: Experience from the Republic of Korea. J Korean Med Sci. 2015; 30:Suppl 2. S115–S121.
Article10. Oh MD, Lee JK. Milestones in history of adult vaccination in Korea. Clin Exp Vaccine Res. 2012; 1:9–17.
Article11. Ryu JU, Kim EK, Youn YS, Rhim JW, Lee KY. Outbreaks of mumps: an observational study over two decades in a single hospital in Korea. Korean J Pediatr. 2014; 57:396–402.
Article12. Dayan GH, Rubin S. Mumps outbreaks in vaccinated populations: are available mumps vaccines effective enough to prevent outbreaks? Clin Infect Dis. 2008; 47:1458–1467.
Article13. Heo JY, Choe KW, Yoon CG, Jeong HW, Kim WJ, Cheong HJ. Vaccination policy in Korean armed forces: current status and future challenge. J Korean Med Sci. 2015; 30:353–359.
Article14. National Institute of Health. Evaluation of mumps outbreak and serology, 2002. Accessed 26 April 2019. Available at: http://www.nih.go.kr/NIH.15. Woo TM. Postexposure management of vaccine-preventable diseases. J Pediatr Health Care. 2016; 30:173–182. quiz 183-4.
Article16. Orlíková H, Malý M, Lexová P, Šebestová H, Limberková R, Jurzykowská L, Kynčl J. Protective effect of vaccination against mumps complications, Czech Republic, 2007-2012. BMC Public Health. 2016; 16:293.
Article17. Rhie K, Park HK, Kim YS, Yeom JS, Park JS, Seo JH, Park ES, Lim JY, Park CH, Woo HO, Youn HS. Factors associated with mumps meningitis and the possible impact of vaccination. Korean J Pediatr. 2016; 59:24–29.
Article18. Gouma S, Hahné SJ, Gijselaar DB, Koopmans MP, van Binnendijk RS. Severity of mumps disease is related to MMR vaccination status and viral shedding. Vaccine. 2016; 34:1868–1873.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Epidemiologic Investigation of a Mumps Outbreak in a Middle School in Pohang, Korea: Effect of vaccination during outbreak
- Mumps outbreak in Incheon, Korea, 2009
- Evaluation of Mumps Vaccine Effectiveness by outbreak investigation in one kindergarten in Ulsan city, 2006
- An Outbreak of Mumps in Taejon, Korea, 1998
- Mumps Transmission Control Status and Inapparent Infection Rate among Middle and High School Students during the 2007-2008 Mumps Outbreak in Daegu