Neurointervention.
2019 Sep;14(2):99-106. 10.5469/neuroint.2019.00080.
Dichotomizing Level of Pial Collaterals on Multiphase CT Angiography for Endovascular Treatment in Acute Ischemic Stroke: Should It Be Refined for 6-Hour Time Window?
- Affiliations
-
- 1Department of Neurology, Ewha Womans University College of Medicine, Seoul, Korea.
- 2Department of Radiology, Seoul National University Bundang Hospital, Korea. jck0097@gmail.com
- 3Department of Neurology, Seoul National University Bundang Hospital, Korea.
- 4Department of Neurology, Gyeongsang National University Changwon Hospital, Changwon, Korea.
- 5Department of Radiology, Chungbuk National University College of Medicine, Cheongju, Korea.
- KMID: 2458489
- DOI: http://doi.org/10.5469/neuroint.2019.00080
Abstract
- PURPOSE
Although endovascular treatment is currently thought to only be suitable for patients who have pial arterial filling scores >3 as determined by multiphase computed tomography angiography (mpCTA), a cut-off score of 3 was determined by a study, including patients within 12 hours after symptom onset. We aimed to investigate whether a cut-off score of 3 for endovascular treatment within 6 hours of symptom onset is an appropriate predictor of good functional outcome at 3 months.
MATERIALS AND METHODS
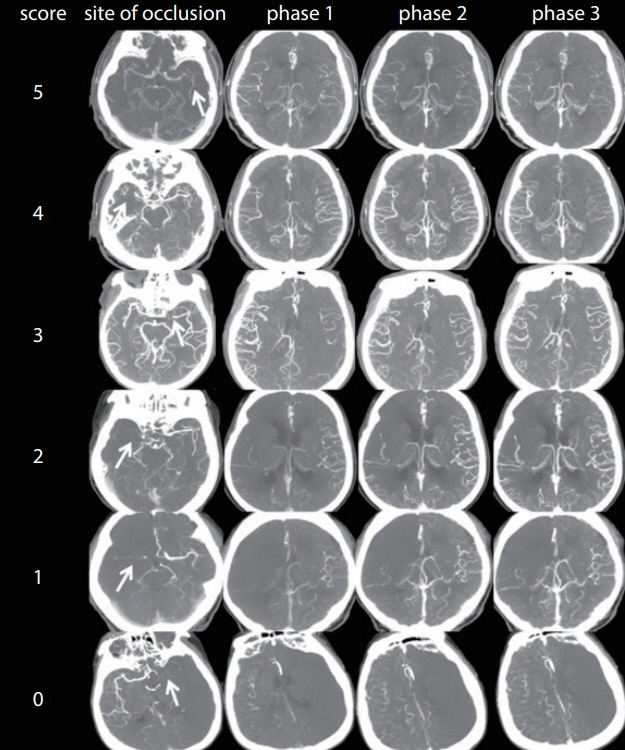
From April 2015 to January 2016, acute ischemic stroke patients treated with mechanical thrombectomy within 6 hours of symptom onset were enrolled into this study. Pial arterial filling scores were semi-quantitatively assessed using mpCTA, and clinical and radiological parameters were compared between patients with favorable and unfavorable outcomes. Multivariate logistic regression analysis was then performed to investigate the independent association between clinical outcome and pial collateral score, with the predictive power of the latter assessed using C-statistics.
RESULTS
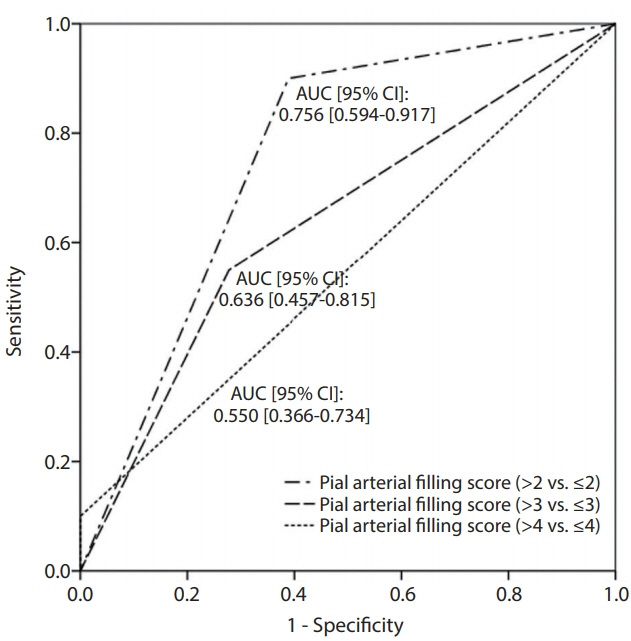
Of the 38 patients enrolled, 20 (52.6%) had a favorable outcome and 18 had an unfavorable outcome, with the latter group showing a lower mean pial arterial filling score (3.6±0.8 vs. 2.4±1.2, P=0.002). After adjusting for variables with a P-value of <0.1 in univariate analysis (i.e., age and National Institutes of Health Stroke Scale score at admission), pial arterial filling scores higher than a cut-off of 2 were found to be independently associated with favorable clinical outcomes (P=0.012). C-statistic analysis confirmed that our model had the highest prediction power when pial arterial filling scores were dichotomized at >2 vs. ≤2.
CONCLUSION
A pial arterial filling cut-off score of 2 as determined by mpCTA appears to be more suitable for predicting clinical outcomes following endovascular treatment within 6 hours of symptom onset than the cut-off of 3 that had been previously suggested.
Figure
Reference
-
1. Goyal M, Menon BK, van Zwam WH, Dippel DW, Mitchell PJ, Demchuk AM, et al. Endovascular thrombectomy after large-vessel ischaemic stroke: a meta-analysis of individual patient data from five randomised trials. Lancet. 2016; 387:1723–1731.
Article2. Hong KS, Ko SB, Yu KH, Jung C, Park SQ, Kim BM, et al. Update of the korean clinical practice guidelines for endovascular recanalization therapy in patients with acute ischemic stroke. J Stroke. 2016; 18:102–113.
Article3. Powers WJ, Derdeyn CP, Biller J, Coffey CS, Hoh BL, Jauch EC, et al. 2015 American Heart Association/American Stroke Association focused update of the 2013 guidelines for the early management of patients with acute ischemic stroke regarding endovascular treatment: a guideline for healthcare professionals from the American Heart Association/American Stroke Association. Stroke. 2015; 46:3020–3035.
Article4. Liebeskind DS. Collateral lessons from recent acute ischemic stroke trials. Neurol Res. 2014; 36:397–402.
Article5. Christoforidis GA, Karakasis C, Mohammad Y, Caragine LP, Yang M, Slivka AP. Predictors of hemorrhage following intra-arterial thrombolysis for acute ischemic stroke: the role of pial collateral formation. AJNR Am J Neuroradiol. 2009; 30:165–170.
Article6. Bang OY, Saver JL, Kim SJ, Kim GM, Chung CS, Ovbiagele B, et al. Collateral flow predicts response to endovascular therapy for acute ischemic stroke. Stroke. 2011; 42:693–699.
Article7. Christoforidis GA, Mohammad Y, Kehagias D, Avutu B, Slivka AP. Angiographic assessment of pial collaterals as a prognostic indicator following intra-arterial thrombolysis for acute ischemic stroke. AJNR Am J Neuroradiol. 2005; 26:1789–1797.8. van den Wijngaard IR, Boiten J, Holswilder G, Algra A, Dippel DW, Velthuis BK, et al. Impact of collateral status evaluated by dynamic computed tomographic angiography on clinical outcome in patients with ischemic stroke. Stroke. 2015; 46:3398–3404.
Article9. Menon BK, d’Esterre CD, Qazi EM, Almekhlafi M, Hahn L, Demchuk AM, et al. Multiphase ct angiography: a new tool for the imaging triage of patients with acute ischemic stroke. Radiology. 2015; 275:510–520.
Article10. Yu AY, Zerna C, Assis Z, Holodinsky JK, Randhawa PA, Najm M, et al. Multiphase ct angiography increases detection of anterior circulation intracranial occlusion. Neurology. 2016; 87:609–616.
Article11. Yang CY, Chen YF, Lee CW, Huang A, Shen Y, Wei C, et al. Multiphase ct angiography versus single-phase CT angiography: comparison of image quality and radiation dose. AJNR Am J Neuroradiol. 2008; 29:1288–1295.
Article12. Demchuk AM, Menon BK, Goyal M. Comparing vessel imaging: noncontrast computed tomography/computed tomographic angiography should be the new minimum standard in acute disabling stroke. Stroke. 2016; 47:273–281.13. Yoo AJ, Simonsen CZ, Prabhakaran S, Chaudhry ZA, Issa MA, Fugate JE, et al. Refining angiographic biomarkers of revascularization: improving outcome prediction after intra-arterial therapy. Stroke. 2013; 44:2509–2512.
Article14. Goyal M, Demchuk AM, Menon BK, Eesa M, Rempel JL, Thornton J, et al. Randomized assessment of rapid endovascular treatment of ischemic stroke. N Engl J Med. 2015; 372:1019–1030.15. Menon BK, Qazi E, Nambiar V, Foster LD, Yeatts SD, Liebeskind D, et al. Differential effect of baseline computed tomographic angiography collaterals on clinical outcome in patients enrolled in the interventional management of stroke iii trial. Stroke. 2015; 46:1239–1244.
Article16. Mortimer AM, Simpson E, Bradley MD, Renowden SA. Computed tomography angiography in hyperacute ischemic stroke: prognostic implications and role in decision-making. Stroke. 2013; 44:1480–1488.
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Imaging in Acute Anterior Circulation Ischemic Stroke: Current and Future
- Hemodynamics of Leptomeningeal Collaterals after Large Vessel Occlusion and Blood Pressure Management with Endovascular Treatment
- A Multicenter Survey of Acute Stroke Imaging Protocols for Endovascular Thrombectomy
- Reperfusion therapy in acute ischemic stroke
- An Update of Recent Guideline for the Endovascular Recanalization Therapy in Acute Ischemic Stroke