J Korean Neurosurg Soc.
2019 Sep;62(5):536-544. 10.3340/jkns.2019.0087.
Long Term Outcome of In-Stent Stenosis after Stent Assisted Coil Embolization for Cerebral Aneurysm
- Affiliations
-
- 1Department of Neurosurgery, Dankook University College of Medicine, Cheonan, Korea. kimyj@dankook.ac.kr
- KMID: 2457943
- DOI: http://doi.org/10.3340/jkns.2019.0087
Abstract
OBJECTIVE
The objective of this study was to evaluatelong-term radiologic prognosis and characteristics of in-stent stenosis (ISS) after stent assisted coiling (SAC) for cerebral aneurysm and analyze its risk factors.
METHODS
Radiological records of 362 cases of SAC during 10 years were retrospectively reviewed. Patients were included in this study if they had follow-up angiogram using catheter selected angiography at least twice. All subjected were followed up from 12 months to over 30 months. Of 120 patients, 123 aneurysms were enrolled. Patient data including age, sex, aneurysm size, neck size, procedural complication, kinds of stent, ISS associated symptom, ruptured state, location of ISS, degree of ISS, radiologic prognosis of ISS, follow-up period of time, and medical comorbidities such as hypertension, diabetes mellitus (DM), dyslipidemia, and smoking were collected.Statistical comparisons of group clinical characteristics were conducted for the total population.
RESULTS
Among 123 casesof aneurysm, 22 cases (17.9%) of ISS were revealed on follow-up angiography. Multiple stenting was performed in three cases and intra-procedural rupture occurred in two cases. Most cases were asymptomatic and symptomatic stenosis was identified in only one case. Sixteen cases were ruptured aneurysm. Mild stenosis was observed in 11 cases. Moderate stenosis was found in eight cases and severe stenosis was identified in three cases. Mean timing of identification of ISS was 8.90 months. The most common type was proximal type. Most cases were improved or not changed on follow-up angiography. Only one case was aggravated from mild stenosis to occlusion of parent artery. Mean follow-up period was 44.3 months. We compared risk factors and characteristic between ISS group and non-ISS group using univariate analysis. Multiple stenting was performed for three cases (13.6%) of the ISS group and four cases (4.0%) of the non-ISS group, showing no statistical difference between the two groups (p=0.108). Additionally, the proportion of patients who had more than two risk factors among four medical risk factors (hypertension, DM, dyslipidemia, and smoking) was higher in the ISS group than that in the non-ISS group, the difference between the two was not statistically significant either (31.8% vs. 12.9%, p=0.05).
CONCLUSION
Clinical course and long-term prognosis of ISS might be benign. Most cases of ISS could be improved or not aggravated. Control of medical co-morbidity might be important. To the best of our knowledge, our study had more cases with longer follow-up period of time than other reports.
MeSH Terms
-
Aneurysm
Aneurysm, Ruptured
Angiography
Arteries
Catheters
Comorbidity
Constriction, Pathologic*
Diabetes Mellitus
Dyslipidemias
Embolization, Therapeutic*
Follow-Up Studies
Humans
Hypertension
Intracranial Aneurysm*
Long Term Adverse Effects
Neck
Parents
Prognosis
Retrospective Studies
Risk Factors
Rupture
Smoke
Smoking
Stents*
Smoke
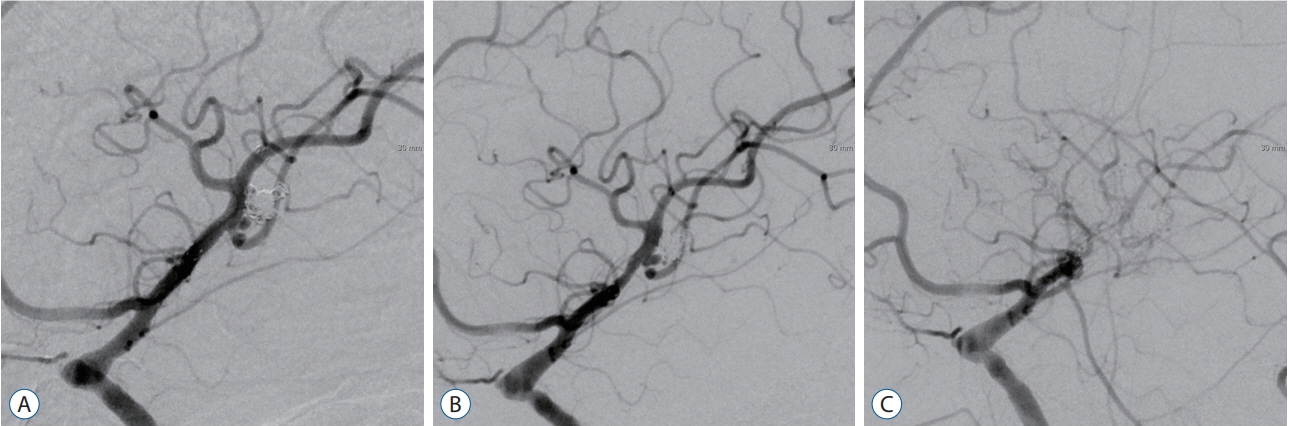
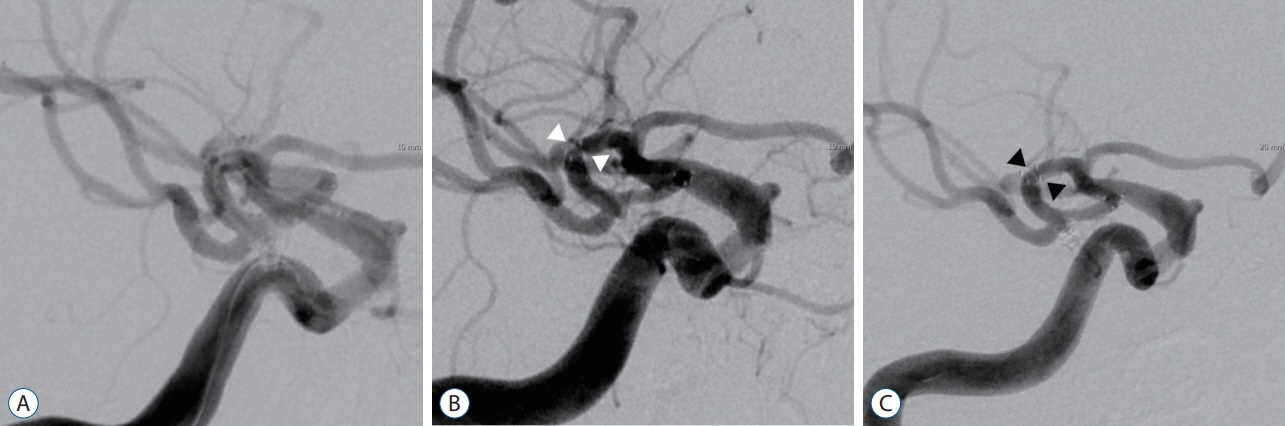
Figure
Cited by 1 articles
-
Neurotoxicity of Paclitaxel and Rapamycin in a Rat Model with Transient Blood-Brain Barrier Opening
Won-Sang Cho, Jung Hoon Choi, O-Ki Kwon
J Korean Neurosurg Soc. 2022;65(2):180-185. doi: 10.3340/jkns.2021.0077.
Reference
-
References
1. Akpek S, Arat A, Morsi H, Klucznick RP, Strother CM, Mawad ME. Self-expandable stent-assisted coiling of wide-necked intracranial aneurysms: a single-center experience. AJNR Am J Neuroradiol. 26:1223–1231. 2005.2. Banerjee C, Chimowitz MI. Stroke caused by atherosclerosis of the major intracranial arteries. Circ Res. 120:502–513. 2017.
Article3. Behme D, Weber A, Kowoll A, Berlis A, Burke TH, Weber W. Low-profile Visualized Intraluminal Support device (LVIS Jr) as a novel tool in the treatment of wide-necked intracranial aneurysms: initial experience in 32 cases. J Neurointerv Surg. 7:281–285. 2015.
Article4. Biondi A, Janardhan V, Katz JM, Salvaggio K, Riina HA, Gobin YP. Neuroform stent-assisted coil embolization of wide-neck intracranial aneurysms: strategies in stent deployment and midterm follow-up. Neurosurgery. 61:460–468. discussion 468-469. 2007.5. Cho YD, Sohn CH, Kang HS, Kim JE, Cho WS, Hwang G, et al. Coil embolization of intracranial saccular aneurysms using the Low-profile Visualized Intraluminal Support (LVISTM™) device. Neuroradiology. 56:543–551. 2014.
Article6. Fargen KM, Mocco J, Neal D, Dewan MC, Reavey-Cantwell J, Woo HH, et al. A multicenter study of stent-assisted coiling of cerebral aneurysms with a Y configuration. Neurosurgery. 73:466–472. 2013.
Article7. Feng X, Qian Z, Liu P, Zhang B, Wang L, Guo E, et al. Comparison of recanalization and in-stent stenosis between the low-profile visualized intraluminal support stent and enterprise stent-assisted coiling for 254 intracranial aneurysms. World Neurosurg. 109:e99–e104. 2018.
Article8. Fiorella D, Albuquerque FC, Deshmukh VR, McDougall CG. Usefulness of the Neuroform stent for the treatment of cerebral aneurysms: results at initial (3-6-mo) follow-up. Neurosurgery. 56:1191–1201. discussion 1201-1202. 2005.
Article9. Fiorella D, Albuquerque FC, Woo H, Rasmussen PA, Masaryk TJ, McDougall CG. Neuroform in-stent stenosis: incidence, natural history and treatment strategies. Neurosurgery. 59:34–42. 2006.
Article10. Gao B, Safain MG, Malek AM. Enterprise stenting for intracranial aneurysm treatment induces dynamic and reversible age-dependent stenosis in cerebral arteries. J Neurointerv Surg. 7:297–302. 2015.
Article11. Hoit DA, Malek AM. Three-dimensional rotational angiographic detection of in-stent stenosis in wide-necked aneurysms treated with a self-expanding intracranial stent. Neurosurgery. 57:1228–1236. discussion 1228-1236. 2005.
Article12. Kanaan H, Jankowitz B, Aleu A, Kostov D, Lin R, Lee K, et al. In-stent thrombosis and stenosis after neck-remodeling device-assisted coil embolization of intracranial aneurysms. Neurosurgery. 67:1523–1532. discussion 1532-1533. 2010.
Article13. Kulcsár Z, Göricke SL, Gizewski ER, Schlamann M, Sure U, Sandalcioglu IE, et al. Neuroform stent-assisted treatment of intracranial aneurysms: long-term follow-up study of aneurysm recurrence and in-stent stenosis rates. Neuroradiology. 55:459–465. 2013.
Article14. Lane A, Vivian P, Coulthard A. Magnetic resonance angiography or digital subtraction catheter angiography for follow-up of coiled aneurysms: do we need both? J Med Imaging Radiat Oncol. 59:163–169. 2015.
Article15. Lubicz B, Collignon L, Raphaeli G, Pruvo JP, Bruneau M, De Witte O, et al. Flow-diverter stent for the endovascular treatment of intracranial aneurysms: a prospective study in 29 patients with 34 aneurysms. Stroke. 41:2247–2253. 2010.
Article16. Lylyk P, Miranda C, Ceratto R, Ferrario A, Scrivano E, Luna HR, et al. Curative endovascular reconstruction of cerebral aneurysms with the pipeline embolization device: the Buenos Aires experience. Neurosurgery. 64:632–642. discussion 642-643; quiz N6. 2009.17. Maldonado IL, Machi P, Costalat V, Mura T, Bonafé A. Neuroform stent-assisted coiling of unruptured intracranial aneurysms: short- and midterm results from a single-center experience with 68 patients. AJNR Am J Neuroradiol. 32:131–136. 2011.
Article18. Mocco J, Fargen KM, Albuquerque FC, Bendok BR, Boulos AS, Carpenter JS, et al. Delayed thrombosis or stenosis following enterprise-assisted stent-coiling: is it safe? Midterm results of the interstate collaboration of enterprise stent coiling. Neurosurgery. 69:908–913. discussion 913-914. 2011.
Article19. Neeb ZP, Edwards JM, Alloosh M, Long X, Mokelke EA, Sturek M. Metabolic syndrome and coronary artery disease in Ossabaw compared with Yucatan swine. Comp Med. 60:300–315. 2010.20. Poncyljusz W, Bilinski P, Safranow K, Baron J, Zbroszczyk M, Jaworski M, et al. The LVIS/LVIS Jr. stents in the treatment of wide-neck intracranial aneurysms: multicentre registry. J Neurointerv Surg. 7:524–529. 2015.
Article21. Prabhakaran S, Warrior L, Wells KR, Jhaveri MD, Chen M, Lopes DK. The utility of quantitative magnetic resonance angiography in the assessment of intracranial in-stent stenosis. Stroke. 40:991–993. 2009.
Article22. Takemoto K, Tateshima S, Rastogi S, Gonzalez N, Jahan R, Duckwiler G, et al. Disappearance of a small intracranial aneurysm as a result of vessel straightening and in-stent stenosis following use of an Enterprise vascular reconstruction device. J Neurointerv Surg. 6:e4. 2014.
Article23. van Amerongen MJ, Boogaarts HD, de Vries J, Verbeek AL, Meijer FJ, Prokop M, et al. MRA versus DSA for follow-up of coiled intracranial aneurysms: a meta-analysis. AJNR Am J Neuroradiol. 35:1655–1661. 2014.
Article24. Vendrell JF, Costalat V, Brunel H, Riquelme C, Bonafe A. Stent-assisted coiling of complex middle cerebral artery aneurysms: initial and midterm results. AJNR Am J Neuroradiol. 32:259–263. 2011.
Article25. Yoon KW, Kim YJ. In-stent stenosis of stent assisted endovascular treatment on intracranial complex aneurysms. J Korean Neurosurg Soc. 48:485–489. 2010.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- In-Stent Stenosis of Stent-Assisted Coil Embolization of the Supraclinoid Internal Carotid Artery Aneurysm
- A Complicated Case of Endovascular Stent Assisted Coil Embolization of an Aneurysm
- Stent-assisted Coil Embolization of Cerebral Aneurysms: Review Article
- Stent-Assisted Coil Embolization for the Proximal Middle Cerebral Artery Fusiform Aneurysm
- Staged Y-shaped Stent Assisted Coil Embolization in a Wide-Neck Basilar Tip Aneurysm: Case Report