Yonsei Med J.
2019 Sep;60(9):876-881. 10.3349/ymj.2019.60.9.876.
Architectural Changes in the Medial Gastrocnemius on Sonography after Nerve Ablation in Healthy Adults
- Affiliations
-
- 1Department and Research Institute of Rehabilitation Medicine, Yonsei University College of Medicine, Seoul, Korea. medicus@yuhs.ac
- 2Hafis Clinic, Seoul, Korea.
- KMID: 2457484
- DOI: http://doi.org/10.3349/ymj.2019.60.9.876
Abstract
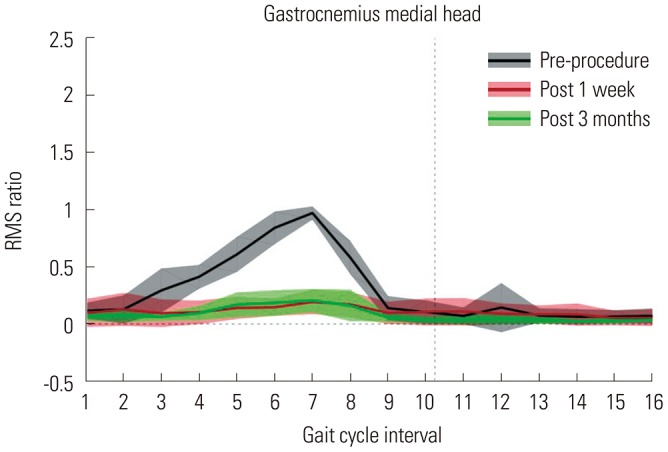
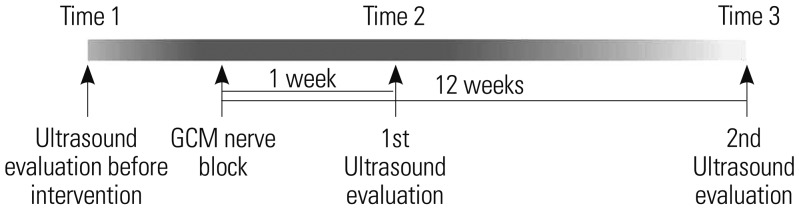
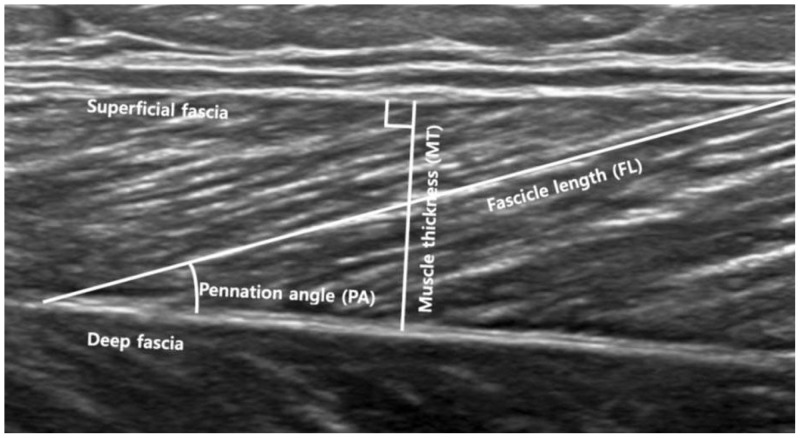
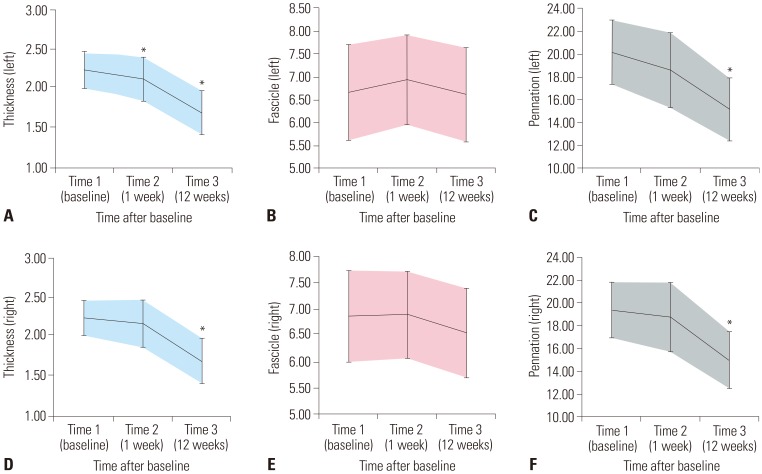
- Architectural changes in healthy muscle after denervation have not yet been reported. This study aimed to investigate architectural changes in the medial head of the gastrocnemius muscle (GCM) after aesthetic tibial nerve ablation in healthy adults using ultrasonography (US). The effects of tibial nerve ablation were verified by visual observation and surface electromyography analysis. US images of medial GCMs were taken by one trained physician using B-mode and real-time US with a linear-array probe before nerve ablation, at 1 week after nerve ablation and at 3 months after nerve ablation in an anatomic standing position with the feet about shoulder-width apart in 19 healthy adults (17 females and 2 males). Muscle thickness was significantly reduced on the left side at 1 week and 3 months after the procedure and on the right side at 3 months after the procedure (p<0.050). Although fascicle length was not significantly changed, pennation angle was significantly reduced on both sides at 3 months after the procedure (p<0.050). Muscle thickness and pennation angle of the muscle fascicle were significantly reduced, although fascicle length was not significantly changed, after tibial nerve ablation in the medial GCM of healthy adults.
Keyword
MeSH Terms
Figure
Reference
-
1. Sunderland S, Ray LJ. Denervation changes in mammalian striated muscle. J Neurol Neurosurg Psychiatry. 1950; 13:159–177. PMID: 14774739.
Article2. Gans C. Fiber architecture and muscle function. Exerc Sport Sci Rev. 1982; 10:160–207. PMID: 6749514.
Article3. Lieber RL. Skeletal muscle structure and function: implications for rehabilitation and sports medicine. 1st ed. Baltimore: Williams & Wilkins;1992.4. Moreau NG, Teefey SA, Damiano DL. In vivo muscle architecture and size of the rectus femoris and vastus lateralis in children and adolescents with cerebral palsy. Dev Med Child Neurol. 2009; 51:800–806. PMID: 19459913.
Article5. Lebiedowska MK, Gaebler-Spira D, Burns RS, Fisk JR. Biomechanic characteristics of patients with spastic and dystonic hypertonia in cerebral palsy. Arch Phys Med Rehabil. 2004; 85:875–880. PMID: 15179639.6. Aiona M. Muscle length and force production in patients with cerebral palsy-the effects of tendon lengthening. IEEE. Pediatric gait: a new millennium in clinical care and motion analysis technology. 1st ed. Chicago: IEEE;2000. p. 30–38.7. Narici M. Human skeletal muscle architecture studied in vivo by non-invasive imaging techniques: functional significance and applications. J Electromyogr Kinesiol. 1999; 9:97–103. PMID: 10098710.
Article8. Narici MV, Binzoni T, Hiltbrand E, Fasel J, Terrier F, Cerretelli P. In vivo human gastrocnemius architecture with changing joint angle at rest and during graded isometric contraction. J Physiol. 1996; 496(Pt 1):287–297. PMID: 8910216.
Article9. Blazevich AJ, Cannavan D, Coleman DR, Horne S. Influence of concentric and eccentric resistance training on architectural adaptation in human quadriceps muscles. J Appl Physiol (1985). 2007; 103:1565–1575. PMID: 17717119.
Article10. Park ES, Sim E, Rha DW, Jung S. Architectural changes of the gastrocnemius muscle after botulinum toxin type A injection in children with cerebral palsy. Yonsei Med J. 2014; 55:1406–1412. PMID: 25048504.
Article11. Li L, Tong KY, Hu X. The effect of poststroke impairments on brachialis muscle architecture as measured by ultrasound. Arch Phys Med Rehabil. 2007; 88:243–250. PMID: 17270524.
Article12. Romkes J, Hell AK, Brunner R. Changes in muscle activity in children with hemiplegic cerebral palsy while walking with and without ankle-foot orthoses. Gait Posture. 2006; 24:467–474. PMID: 16413188.
Article13. Schroeder AS, Ertl-Wagner B, Britsch S, Schröder JM, Nikolin S, Weis J, et al. Muscle biopsy substantiates long-term MRI alterations one year after a single dose of botulinum toxin injected into the lateral gastrocnemius muscle of healthy volunteers. Mov Disord. 2009; 24:1494–1503. PMID: 19489066.
Article14. Fleckenstein JL, Watumull D, Conner KE, Ezaki M, Greenlee RG Jr, Bryan WW, et al. Denervated human skeletal muscle: MR imaging evaluation. Radiology. 1993; 187:213–218. PMID: 8451416.
Article15. Hides JA, Cooper DH, Stokes MJ. Diagnostic ultrasound imaging for measurement of the lumbar multifidus muscle in normal young adults. Physiother Theory Pract. 1992; 8:19–26.
Article16. Hides J, Richardson C, Jull G, Davies S. Ultrasound imaging in rehabilitation. Aust J Physiother. 1995; 41:187–193. PMID: 25026042.
Article17. Stokes M, Hides J, Nassiri DK. Musculoskeletal ultrasound imaging: diagnostic and treatment aid in rehabilitation. Physical Therapy Reviews. 1997; 2:73–92.
Article18. Whittaker JL, Teyhen DS, Elliott JM, Cook K, Langevin HM, Dahl HH, et al. Rehabilitative ultrasound imaging: understanding the technology and its applications. J Orthop Sports Phys Ther. 2007; 37:434–449. PMID: 17877280.
Article19. Burkholder TJ, Fingado B, Baron S, Lieber RL. Relationship between muscle fiber types and sizes and muscle architectural properties in the mouse hindlimb. J Morphol. 1994; 221:177–190. PMID: 7932768.
Article20. Sacks RD, Roy RR. Architecture of the hind limb muscles of cats: functional significance. J Morphol. 1982; 173:185–195. PMID: 7120421.
Article21. An KN, Hui FC, Morrey BF, Linscheid RL, Chao EY. Muscles across the elbow joint: a biomechanical analysis. J Biomech. 1981; 14:659–669. PMID: 7334026.
Article22. Brand RA, Pedersen DR, Friederich JA. The sensitivity of muscle force predictions to changes in physiologic cross-sectional area. J Biomech. 1986; 19:589–596. PMID: 3771581.
Article23. Edgerton VR, Apor P, Roy RR. Specific tension of human elbow flexor muscles. Acta Physiol Hung. 1990; 75:205–216.24. Huijing PA. Architecture of the human gastrocnemius muscle and some functional consequences. Acta Anat (Basel). 1985; 123:101–107. PMID: 4061024.
Article25. Lieber RL, Steinman S, Barash IA, Chambers H. Structural and functional changes in spastic skeletal muscle. Muscle Nerve. 2004; 29:615–627. PMID: 15116365.
Article26. Lieber RL, Fridén J. Functional and clinical significance of skeletal muscle architecture. Muscle Nerve. 2000; 23:1647–1666. PMID: 11054744.
Article27. Kawakami Y, Abe T, Fukunaga T. Muscle-fiber pennation angles are greater in hypertrophied than in normal muscles. J Appl Physiol (1985). 1993; 74:2740–2744. PMID: 8365975.
Article28. Manske SL, Boyd SK, Zernicke RF. Muscle and bone follow similar temporal patterns of recovery from muscle-induced disuse due to botulinum toxin injection. Bone. 2010; 46:24–31. PMID: 19853070.
Article29. Shen J, Ma J, Lee C, Smith BP, Smith TL, Tan KH, et al. How muscles recover from paresis and atrophy after intramuscular injection of botulinum toxin A: study in juvenile rats. J Orthop Res. 2006; 24:1128–1135. PMID: 16602109.
Article30. Glass GE, Hussain M, Fleming AN, Powell BW. Atrophy of the intrinsic musculature of the hands associated with the use of botulinum toxin-A injections for hyperhidrosis: a case report and review of the literature. J Plast Reconstr Aesthet Surg. 2009; 62:e274–e276. PMID: 18203669.
Article31. Choi WH, Song CW, Kim YB, Ha CS, Yang GH, Woo HD, et al. Skeletal muscle atrophy induced by intramuscular repeated dose of botulinum toxin type A in rats. Drug Chem Toxicol. 2007; 30:217–227. PMID: 17613007.
Article32. Tok F, Ozçakar L, Safaz I, Alaca R. Effects of botulinum toxin-A on the muscle architecture of stroke patients: the first ultrasonographic study. J Rehabil Med. 2011; 43:1016–1019. PMID: 21915584.
Article33. Kawano A, Yanagizono T, Kadouchi I, Umezaki T, Chosa E. Ultrasonographic evaluation of changes in the muscle architecture of the gastrocnemius with botulinum toxin treatment for lower extremity spasticity in children with cerebral palsy. J Orthop Sci. 2018; 23:389–393. PMID: 29146092.
Article34. Seynnes OR, Maganaris CN, de Boer MD, di Prampero PE, Narici MV. Early structural adaptations to unloading in the human calf muscles. Acta Physiol (Oxf). 2008; 193:265–274. PMID: 18266998.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Comparison of Tendon Reflex Responses between Two Heads of Gastrocnemius in Spastic Hemiplegia and Healthy Subjects
- Spasticity and Electrophysiologic Changes after Extracorporeal Shock Wave Therapy on Gastrocnemius
- Soft Tissue Coverage Using a Combined Gastrocnemius-medial Sural Artery Perforator Flap
- Anatomic Motor Point Localization for the Treatment of Gastrocnemius Muscle Spasticity
- Architectural Changes of the Gastrocnemius Muscle after Botulinum Toxin Type A Injection in Children with Cerebral Palsy