J Korean Ophthalmol Soc.
2019 Aug;60(8):725-730. 10.3341/jkos.2019.60.8.725.
Thyroid Abnormality and Dry Eye Syndrome: a Cross-sectional Study from the Republic of Korea
- Affiliations
-
- 1Department of Ophthalmology, Soonchunhyang University Bucheon Hospital, Soonchunhyang University College of Medicine, Bucheon, Korea. sieh12@schmc.ac.kr
- 2Department of Ophthalmology, Soonchunhyang University Seoul Hospital, Soonchunhyang University College of Medicine, Seoul, Korea.
- KMID: 2455454
- DOI: http://doi.org/10.3341/jkos.2019.60.8.725
Abstract
- PURPOSE
To investigate the relationship between thyroid abnormality and dry eye syndrome (DES) in a nationally representative Korean population.
METHODS
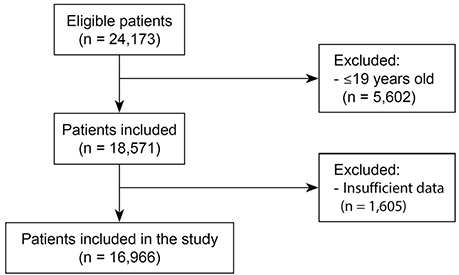
A population-based prospective cross-sectional study was conducted, using the thyroid abnormality data set of the Korean National Health and Nutrition Examination Survey, 2010 - 2012. A total of 16,966 Korean participants with DES were enrolled in the study.
RESULTS
The DES patients were predominantly women, non-smokers and non-drinkers, living in urban regions, with a low income and body mass index (BMI), and with a higher percentage of hypertension, hyperlipidemia, thyroid abnormalities, thyroid diseases, and thyroid cancers. After adjusting for all significant variables, thyroid abnormality (odds ratio [OR], 1.93; 95% confidence interval [CI], 1.43-2.61), thyroid disease (OR, 1.85; 95% CI, 1.37-2.52), and thyroid cancer (OR, 2.45; 95% CI, 1.06-5.67) were significantly associated with DES. There was also a significant association between DES and thyroid abnormalities (OR, 2.02; 95% CI, 1.47-2.76), thyroid diseases (OR, 1.93; 95% CI, 1.41-2.65), and thyroid cancer (OR, 2.62; 95% CI, 1.06-6.62) in the female group, but there was no significant association in the male group.
CONCLUSIONS
Thyroid abnormalities, thyroid diseases, and thyroid cancers were associated with DES in a nationally representative Korean population. Close evaluation of thyroid abnormalities is therefore needed when treating female patients.
Keyword
MeSH Terms
Figure
Reference
-
1. Yamada M, Li AW, Wall JR. Thyroid-associated ophthalmopathy: clinical features, pathogenesis, and management. Crit Rev Clin Lab Sci. 2000; 37:523–549.
Article2. Bartley GB, Fatourechi V, Kadrmas EF, et al. Chronology of Graves' ophthalmopathy in an incidence cohort. Am J Ophthalmol. 1996; 121:426–434.3. Burch HB, Wartofsky L. Graves' ophthalmopathy: current concepts regarding pathogenesis and management. Endocr Rev. 1993; 14:747–793.
Article4. da Fonseca FL, Yamanaka PK, Mazoti L, et al. Correlation among ocular surface disease, xerostomia, and nasal symptoms in patients with differentiated thyroid carcinoma subjected to radioiodine therapy: a prospective comparative study. Head Neck. 2017; 39:2381–2396.
Article5. Nowak M, Marek B, Kos-Kudła B, et al. Tear film profile in patients with active thyroid orbithopathy. Klin Oczna. 2005; 107:479–482.6. Craig JP, Nelson JD, Azar DT, et al. TFOS DEWS II report executive summary. Ocul Surf. 2017; 15:802–812.
Article7. Eckstein AK, Finkenrath A, Heiligenhaus A, et al. Dry eye syndrome in thyroid-associated ophthalmopathy: lacrimal expression of TSH receptor suggests involvement of TSHR-specific autoantibodies. Acta Ophthalmol Scand. 2004; 82(3 Pt 1):291–297.8. Gilbard JP, Farris RL. Ocular surface drying and tear film osmolarity in thyroid eye disease. Acta Ophthalmol (Copenh). 1983; 61:108–116.
Article9. Iskeleli G, Karakoc Y, Abdula A. Tear film osmolarity in patients with thyroid ophthalmopathy. Jpn J Ophthalmol. 2008; 52:323–326.
Article10. Rocha EM, Mantelli F, Nominato LF, Bonini S. Hormones and dry eye syndrome: an update on what we do and don't know. Curr Opin Ophthalmol. 2013; 24:348–355.11. Ahn JM, Lee SH, Rim TH, et al. Prevalence of and risk factors associated with dry eye: the Korea National Health and Nutrition Examination Survey 2010-2011. Am J Ophthalmol. 2014; 158:1205–1214.e7.
Article12. Yoon KC, Mun GH, Kim SD, et al. Prevalence of eye diseases in South Korea: data from the Korea National Health and Nutrition Examination Survey 2008-2009. Korean J Ophthalmol. 2011; 25:421–433.
Article13. Schein OD, Muñoz B, Tielsch JM, et al. Prevalence of dry eye among the elderly. Am J Ophthalmol. 1997; 124:723–728.
Article14. Moss SE, Klein R, Klein BE. Prevalence of and risk factors for dry eye syndrome. Arch Ophthalmol. 2000; 118:1264–1268.
Article15. Shimmura S, Shimazaki J, Tsubota K. Results of a population-based questionnaire on the symptoms and lifestyles associated with dry eye. Cornea. 1999; 18:408–411.
Article16. Chia EM, Mitchell P, Rochtchina E, et al. Prevalence and associations of dry eye syndrome in an older population: the Blue Mountains Eye Study. Clin Exp Ophthalmol. 2003; 31:229–232.
Article17. Lee AJ, Lee J, Saw SM, et al. Prevalence and risk factors associated with dry eye symptoms: a population based study in Indonesia. Br J Ophthalmol. 2002; 86:1347–1351.
Article18. Starrenburg-Razenberg AJ, Castro Cabezas M, Gan IM, et al. Four patients with hypothyroid Graves' disease. Neth J Med. 2010; 68:178–180.19. Sabita P, Ajit T, Narayan SD, et al. Ocular manifestations in thyroid eye disorder: a cross-sectional study from Nepal. Int J Clin Med. 2016; 7:814–823.
Article20. Uchino M, Nishiwaki Y, Michikawa T, et al. Prevalence and risk factors of dry eye disease in Japan: Koumi study. Ophthalmology. 2011; 118:2361–2367.
Article21. Li H, Li J. Thyroid disorders in women. Minerva Med. 2015; 106:109–114.22. Morganti S, Ceda GP, Saccani M, et al. Thyroid disease in the elderly: sex-related differences in clinical expression. J Endocrinol Invest. 2005; 28:11 Suppl Proceedings. 101–104.23. Fairweather D, Frisancho-Kiss S, Rose NR. Sex differences in autoimmune disease from a pathological perspective. Am J Pathol. 2008; 173:600–609.
Article
- Full Text Links
- Actions
-
Cited
- CITED
-
- Close
- Share
- Similar articles
-
- Factors affecting dry eye syndrome and quality of life among college students in Korea: a cross-sectional study
- Risk Factors for Dry Eye in Thyroid-Associated Ophthalmopathy
- Association Between Serum 25-Hydroxyvitamin D Levels and Dry Eye in Korean Adults: A Study Based on Korean National Health and Nutrition Examination Survey, 2010–2011
- Clinical Significance of Tear Film Osmolarity for Non-Sjögren Dry Eye Diagnosis
- Points to consider when developing drugs for dry eye syndrome